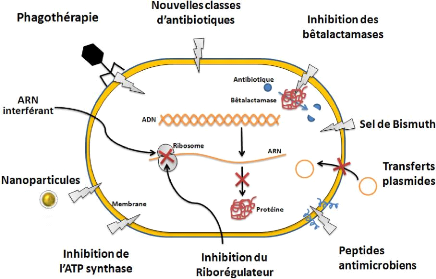
Figure 31. Stratégies et les cibles
bactériennes utilisées pour lutter contre la résistance
aux
antibiotiques (Lemaoui et al. 2017).
REFERENCES
BIBLIOGRAPHIQUE
72
Références bibliographiques
Références bibliographiques
· Abbas M, Cherkaoui A, Fankhauser C, Schrenzel
J et Harbarth S. Carbapénémases ; implications cliniques
et épidémiologique pour la Suisse. Méd Suisse
338: 882-884. 2012.
· Ahmed Z.B., Ayad A., Mesli E., Messai Y.,
Bakour R. et Drissi M. CTX-M-15 extended-spectrum beta-lactamases in
Enterobacteriaceae in the intensive care unit of Tlemcen Hospital,
Algeria. East Mediterr Health J, 18, 382-6.
2012.
· Ahoyo A.T., Baba-Moussa L., Anago A.E., Avogbe
P., Missihoun T.D., Loko F., Prevost G., Sanni A. and Dramane K.
[Incidence of infections dues to Escherichia coli strains
producing extended spectrum betalactamase, in the Zou/Collines Hospital Centre
(CHDZ/C) in Benin]. Med Mal Infect, 37, 746-52.
2007.
· Aibinu I.E., Pfeider Y., Ogunsola F., Odugbemi
T., Koenig W. et Gheberemedhin B.. Emergence of bêta-lactamases
OXA-10, VEB-1 and CMY in Providencia spp. from Nigeria. J
Antimicrob Chemother, 66, 1931-1932.
2011.
· Aktas Z, Kayacan CB and Schneider I.
Carbapenem- hydrolyzing oxacillinase OXA-48, persists in Istanbul, Turkey.
Chemother; 54:101-6. 2008.
· Al-Agamy M.H., Shibl A.M. and Tawfik A.F.
Prevalence and molecular characterization of extended-spectrum
beta-lactamase-producing Klebsiella pneumoniae in Riyadh, Saudi
Arabia. Ann Saudi Med. 29(4): 253-257. 2009.
· Ambler R.P., Coulson A.F.W., Frére
J.M., Ghuysen J.M., Joris B., Forsman M., Levesque R.C., Tiraby A. and Waley
S.G. A standard numbering scheme for the class A f3-lactamases.
Biochem. J. 276: 269-270. 1991.
· Ambler, R.P. The structure of
f3-lactamases. Phil Trans R Soc Lond Biol Sci. 289: 321331.
1980.
· Andersson D.I. and Hughes D.
Antibiotic resistance and its cost: is it possible to reverse
resistance? Nat Rev Microbial; 8:260-71. 2010.
· Anonyme. 2014. Antimicrobial
Resistance: Global report on surveillance 2014. FRANCE: (WHO) World Health
Organization.
· Arlet G. et Philippon, A. Les
nouvelles f3-lactamases à l'aube du troisième millénaire.
Rev Franç Lab. 352 : 41-55. 2003.
73
Références bibliographiques
· Armand-Lefèvre L. Antibiotic
resistance in the community: Myth or reality? The threat of ESBL producing
enterobacteria doi. j.antinf. 01.004. 2017.
· Asensio A., Oliver A., Gonzalez-Diego P.,
Baquero F., Perez-Diaz J.C., Ros P., Cobo J., Palacios M., Lasheras D. and
Canton R. Outbreak of a multiresistant Klebsiella pneumoniae
strain in an intensive care unit: antibiotic use as risk factor for
colonization and infection. Clin Infect Dis. 30: 55-60.
2000.
· Avril J.L., Denis F., Dabernat H. et Monteil
H. Bactériologie Clinique. 3éme
édition. Ellipses. Paris. 171-172. 2000.
· Baba Ahmed-Kazi Tani Z., Decré D.,
Genel N., Boucherit-Otmani Z., Arlet G. and Drissi, M. Molecular and
Epidemiological Characterization of Enterobacterial Multidrug65 Resistant
Strains in Tlemcen Hospital (Algeria) (2008-2010). Microbial Drug
Resistance. 19(3): 185-190. 2013.
· Bandoh K., Muto Y., Watanabe K., Katoh N. and
Ueno K. Biochemical properties and purification of metallo-B-lactamase
from Bacteroïdes fragiIis. Antimicrob. Agents Chemother.
35(2): 371-372. 1991.
· Barrial K. et Scotet J.
Classification raisonnée des â-lactamases chez les
bacilles Gram négatif. Perspective d'évolution. Tig.
Bact. 3-10. 2006.
· Bebrone C. Metallo-beta-lactamases
(classification, activity, genetic organization, structure, zinc coordination)
and their superfamily. Biochem Pharmacol. 74: 1686-701.
2007.
· Belmonte O., Drouet D., Alba J., Moiton M.-P.,
Kuli B., Lugagne-Delpon N., Mourlan C. et Jaffar-Bandjee M.C.
Evolution de la résistance des entérobactéries
aux antibiotiques sur l'île de la Réunion : émergence des
bêta-lactamases à spectre élargi. Pathologie Biologie
58, 18-24. 2010.
· Ben Ayed H., Gargouri M., Ben Jemaa T., Ben
Yahia M., Smaoui F., Marrakchi C., Koubaa M. et Ben Jemaa M. Facteurs
prédisposant d'infection urinaire à bactéries
multi-résistantes aux antibiotiques. Médecine et Maladies
Infectieuses, Vol 47, Issue 4, p S30. Juin 2017.
· Ben Redjeb, S., Ben Hassen, A., Hammami, A.,
and Kechrid, A. Epidémiologie des résistances
bactériennes en Tunisie. «Résistance aux
antibiotiques». Press. Méd. 1-5. 2000.
74
Références bibliographiques
· Benammar S., Benmehidi M., Bouziane F.,
Boukhalfa S. et Makhloufi M. Qu'en est-il de la résistance des
entérobactéries aux C3G en ville et à l'hôpital ?
Laboratoire de Microbiologie du CHU Batna, Algérie. J. Med Mal;
03: 071. 2017.
· Bennett P.M. Plasmid encoded
antibiotic resistance: acquisition and transfer of antibiotic resistance genes
in bacteria. Br J Pharmacol; 153 Suppl 1:S347-57.
2008.
· Béreaud J. Le technicien
d'analyse biologique guide et pratique. Edition médicales
internationales. Londres-Paris-new York. 871-984. 2001.
· Bialek-Davenet S., Marcon E., Leflon-Guibout
V., Lavigne J.P., Bert F., Moreau R. and Nicolas-Chanoine M.H. In
vitro selection of ram R and sox R mutants overexpressing.
2011.
· Bonnet R. Growing group of
extended-spectrum-beta-lactamases: the CTX-M enzymes. Antimicrob Agents
Chemother. 48: 1-14. 2004.
· Bonnet R., Sampaio J.L., Chanal C., Sirot D.,
De Champs C., Viallard J.L., Labia R. and Sirot J. A novel class A
extended-spectrum â-lactamase (BES-1) in Serratia marcescens
isolated in Brazil. Antimicrob. Agents Chemother. 44: 3061-3068.
2000a.
· Boulahbal F. Manuel de microbilogie.
2éme édition. Office des publications universitaires.
Algérie. 20-273. 2010.
· Bourdjilat F., Bouchrif B., Dersi N., Perrier
Gros-Claude J.D., Amarouche, H. et Timinouni M. Emergence of
extended-spectrum beta-lactamase-producing Escherichia coli in
community-acquired urinary infections in Casablanca, Morocco. J Infect Dev
Ctries 5, 850-855. 2011.
· Bourigault C., Corvec S., Bemer P., Juvin
M.E., Guillouzouic A., Crémet L., Reynaud A., Leprince C. et Lepelletier
D. Impact de l'augmentation de l'incidence des
entérobactéries productrices de bêta-lactamases à
spectre étendu (EBLSE) sur l'application des précautions
complémentaires dans un centre hospitalier universitaire. Pathologie
Biologie, Volume 61, Issue 5, Pages 217-222. October
2013.
· Boyer A., Clouzea B., Mzali f., Hilbert G. et
Gruson D. Les nouvelles résistances aux antibiotiques.
jarca. 2011.
· Bradford P. A. Extended-spectrum
beta-lactamases in the 21st century: characterization, epidemiology, and
detection of this important resistance threat. Clin Microbiol Rev,
14, 933-951. 2001a.
75
Références bibliographiques
· Bradford P.A. Automated thermal
cycling is superior to traditional methods for nucleotide sequencing of
blaSHV genes. Antimicrob. Agents Chemother. 43: 2960-2963.
1999.
· Bradford P.A. What's New in
beta-lactamases? Curr Infect Dis Rep, 3, 13-19.
2001b.
· Brisse S. and Verhoef J. Phylogenetic
diversity of Klebsiella pneumoniae and Klebsiella oxytoca
clinical isolates revealed by randomly amplified polymorphic DNA, gyrA
and parC genes sequencing and automated ribotyping. Int J
Syst Evol Microbiol. 51: 915-924. 2001.
· Bush K. and Jacoby G.A. Updated
functional classification of beta-lactamases. Antimicrob Agents Chemother;
54:969-76. 2010.
· Bush K. Extended-spectrum
beta-lactamases in North America, 1987-2006. Clin Microbiol Infect, 14
Suppl 1, 134-43. 2008.
· Bush K. Updated functional
classification of b-lactamases. Antimicrob Agents Chemother. p
54:969-76. 2010.
· Bush K., Jacoby G.A. and Medeiros A.A.
A functional classification scheme for Blactamases and its correlation
with molecular structure. Antimicrob Agents Chemother. 39(6):
1211-1233. 1995.
· Buyck J.M., Luyckx C., Ioli M.G.G., Krause
K.M., Nichols W.W., Tulkens P.M. and Bambeke F.V. Pharmacodynamics of
ceftazidime/avibactam against extracellular and intracellular forms of
Pseudomonas aeruginosa. JAC. 16-94. 2016.
· Canton R., Novais A., Valverde A., Machado E.,
Peixe L., Baquero F. et Coque T. M. Prevalence and spread of
extended-spectrum beta-lactamase-producing Enterobacteriaceae in
Europe. Clin Microbiol Infect, 14 Suppl 1, 144-53.
2008.
· Carattoli A. Resistance Plasmid
Families in Enterobacteriaceae Antimicrob. Agents Chemother; 53:
2227-2238. 2009.
· Carrer A., Poirel L., Yilmaz M.
Spread of OXA-48- encoding plasmid in Turkey and beyond. Journal
Antimicrob Agents Chemother, 54: 1369-73. 2010.
· CA-SFM 2013. Recommandations Paris
2013.
· CA-SFM/EUCAST 2014. Recommandations Paris
2014.
· Castanheira M, Deshpande LM and Mathai
D. Early dissemination of NDM-1- and OXA-181-producing
Enterobacteriaceae in Indian hospitals: report from the SENTRY
76
Références bibliographiques
Antimicrobial Surveillance Program, 2006-2007. Antimicrob
Agents Chemother; 55: 1274-8. 2011.
· Cavallo J.D., Faber R., Jehl F., Rapp C. et
Garrabé E. Bétalactamines. Mal. inf. 1: 129-20.
2004.
· Chopra I., O'Neill A. and Miller K.
The role of mutators in the emergence of antibiotic-resistant
bacteria. Drug Resist Updates. 6: 137-145. 2003.
· Chow J.W., Fine M.J., Shlaes D.M., Quinn J.P.,
Hooper D.C., Johnson M.P., Ramphal R., Wagener M.M., Miyashiro D.K. and Yu V.L.
Enterobacter bacteremia: clinical features and emergence of
antibiotic resistance during therapy. Ann Intern Med. 115(8): 585-590.
1991.
· Colodner R., Rock W., Chazan B., Keller N.,
Guy N., Sakran W. and Raz R. Risk Factors for development of
Extended-Spectrum Beta-lactamase-Producing Bacteria in Nonhospitalized
Patients. Eur J Microbiol Infect Dis. 23: 163-167.
2004.
· Cuzon G, Ouanich J, Gondret R, Naas T et Nordmann
P. Outbreak of OXA-48-positive carbapenem-resistant Klebsiella
pneumoniae isolates in France. Antimicrob Agents Chemother; 55:
2420-3. 2011.
· Datta N. and Kontomichalou, P.
Penicillinase synthesis controlled by infectious factors in
Enterobacteriaceae. Nature 208: 239-241. 1965.
· Davies J. Origins, acquisition and
dissemination of antibiotic resistance determinants.207:15-27.
1997.
· Dbaibo G.S. Old and new targets of
antibacterial therapy. Leb. Med. J. 48: 177-181.
2000.
· Decoster A.
Entérobactéries (internet). FLM. 1-16. 2005.
Available from:
http://anne.decoster.free.fr/btelechar/bpoly/enteroba05.pdf.
· Decousser J.W., Poirel L. and Nordmann P.
"Characterization of a chromosomally encoded extended-spectrum class A
beta-lactamase from Kluyvera cryocrescens". Antimicrob. Agents
Chemother. 45(12): 3595-3598. 2001.
· Delrras C. Microbiologie pratique
pour le laboratoire d'analyses ou de contrôle sanitaire. Edition
médicales internationales. Lavoisier. Paris. 247 p.
2007.
· Diamantis L, Beziz D., Bonnet-zamponi D.,
Armaingaud D., Ombandza E., Pitsch A., Aufaure S., Tangre L, F. Tubach F et
Gauzit R. Antibiorésistance des entérobactéries
isolées d'ECBU réalisés dans huit établissements
pour personnes âgées dépendantes (EHPAD) en France.
j.Med Mal ; 03.070.2017.
77
Références bibliographiques
· Domingues S, Da Silva G.J and Nielsen K.M.
Integrons: vehicles and pathways for horizontal dissemination in
bacteria. Mob Genent Elements; 2(5): 211-223.
2012.
· Drieux L., Brossier F., Sougakoff W. and
Jarlier V. Phenotypic detection of extended-spectrum beta-lactamase
production in Enterobacteriaceae: review and bench guide. Clin Microbiol
Infect. 14: 90-103. 2008.
· Duval V., Maiga I., Maiga A., Guillard T.,
Brasme L., Forte D., Madoux J., Vernet-Garnier V. and De Champs C.
High Prevalence of CTX-M-Type Bêta-Lactamases among Clinical
Isolates of Enterobacteriaceae in Bamako, Mali. Antimicrobial
Agents and Chemotherapy 53, 4957-4958.
2009.
· Ebongue C.O., Tsiazok M.D., Nda Mefo'o J.P.,
Ngaba G.P., Beyiha G. et Adiogo D. Evolution of antibiotic resistance
of Enterobacteriaceae isolated at the Douala General Hospital from 2005 to
2012. Pan Afr Med J; 20: 227. 2015.
· El Salabi A, Walsh T.R and Chouchani C.
Extended spectrum -lactamases, Carbapenemases and mobile genetic
elements responsible for antibiotics resistance in Gram-negative bacteria.
Crit Rev Microbiol; 39: 113-122. 2013.
· Elhani D. Les bêta-lactamases
à spectre étendu : le défi s'accentue. Ann Biol
Clin. 70 (2) ; 117-40. 2012.
· Farmer J.J, Boatwright K.D and Janda J.M.
Enterobacteriaceae: Introduction and identification. Manual of
Clinical microbiology. Washington, DC, USA: ASM press. 9th ed: 649-669.
2007.
· Feizabadi M.M., Mahamadi-Yeganeh S.,
Mirsalehian A., Mirafshar S.M., Mahboobi M., Nili F. and Yadegarinia D.
Genetic characterization of ESBL producing strains of Klebsiella
pneumoniae from Tehran hospitals. J Infect Dev Ctries. 4:
609-615. 2010.
· Follath F., Costa E., Thommen A., Frei R.,
Burdeska A. and Meyer J. Clinical consequences of development of
resistance to third generation cephalosporins. Eur J Clin Microbiol.
6(4): 446-450. 1987.
· Frank T., Arlet G., Gautier V.A.T. et Bercion
R. Extended-spectrum â-Lactamase- producing
Enterobacteriaceae, Central African Republic. Emerging Infectious
Diseases, 12, 863-865. 2006.
· Fritzh K., Bottger E.C., Zinkernagel M.,
Haller O., Eckert J. et Deplazes P. Manuel de poche de microbiologie.
293-764. 2008.
78
Références bibliographiques
· Gangoue-pieboji J., Bedenic B., Koulla-shiro
S., Randegger C., Adiogo D., Ngassam P., Ndumbe P., Hacheler H.
Extended-spectrum â-lactamase producing enterobacteriacea
in Yaounde , Cameroon. Journal Clin Micr. 43: 3273-3277.
2005.
· Garrity M.G., D. J. Brenner, N.R. Krieg et
J.T. Staley. BERGEY'S MANUAL_ OF Systematic Bacteriology,
Second Edition, Volume Two, The Proteobacteria
Part B, the Gammaproteobacteria.
2005.
· Gaudy C. et Buxeraud J. Antibiotiques
: Pharmacologie et thérapeutique. 16-17. 2005.
· Gazengel J.M. Le préparateur
en pharmacie. Technique et documentation 19-21. 2007.
· Georgopapadakou N.H.
Penicillin-binding proteins and bacterial resistance to
â-lactams. Antimicrob. Agents Chemother. 37: 2045-2053.
1993.
· Giraud-Morin C. and Fosse T. [Recent
evolution and characterization of extended-spectrum beta-lactamase producing
enterobacteria in the CHU of Nice (2005-2007)]. Pathol Biol
(Paris), 56, 417-23. 2008.
· Gniadkowski M. Evolution and
epidemiology of extended spectrum beta-lactamases and ESBL producing
micro-organisms. Clin. Microbial infect. 7: 557 -608.
2001.
· Goldstein F.W., Pean Y. and Gertner J.
Resistance to ceftriaxone and other betalactams in bacteria isolated
in the community. The Vigil'Roc Study Group. Antimicrob. Agents
Chemother. 39(11): 2516-2519. 1995.
· Goossens H. and Grabein B. Prevalence
and antimicrobial susceptibility data for extended-spectrum b-lactamase and
AmpC-producing Enterobacteriaceae from the MYSTIC Program in Europe
and the United States (1997-2004). Diagnostic Microbiology and Infectious
Disease 53, 257-264. 2005.
· Grall N. et Muller-Serieys C.
Carbapénèmes. Mal. inf. 1-16.
2013.
· Grosjean J.C. Darchambaud M. et Pasquier C.
Bacteriologie et virology pratique. 2éme édition. Boeck.
Paris. 131-133. 2011.
· Gülmez D, Woodford N and Palepou
MF. Carbapenem-resistant Escherichia coli and Klebsiella
pneumoniae isolates from Turkey with OXA-48-like carbapenemases and outer
membrane protein loss. Int J Antimicrob Agents; 31:523-6.
2008.
· Gupta V. and Datta, P.
Extended-spectrum beta-lactamases (ESBL) in community isolates from
North India: frequency and predisposing factors. Int J Infect Dis. 11:
88-89. 2007.
79
Références bibliographiques
· Haeggman S., Löfdahl S., Paauw A.,
Verhoef J. and Brisse S. Diversity and evolution of the class A
chromosomal beta-lactamase gene in Klebsiella pneumoniae.
Antimicrob. Agents Chemother. 48: 2400-2408. 2004.
· Hailaji A., Ould Salema M.L. et Ghaber S.M.
La sensibilité aux antibiotiques des bactéries
uropathogènes dans la ville de Nouakchott -- Mauritanie N.S.M.
Journal progrès en urologie ; 26, 346-352.
2016.
· Hall L.M., Livermore D.M., Gur D., Akova M.
and Akalin H.E. OXA-11, an extended-spectrum variant of OXA-10 (PSE-2)
â-lactamase from Pseudomonas aeruginosa. Antimicrob. Agents
Chemother. 37(8): 1637-1644. 1993.
· Hammond D.S., Schooneveldt J.M., Nimmo G.R.,
Huygens F. and Giffard P.M. blaSHV genes in Klebsiella
pneumoniae: different allele distributions are associated with different
paromoters within individual isolates. Antimicrob. Agents Chemother.
49: 256263. 2005.
· Harbottle H, Thakur S, Zhao D and White
G. Genetics of antimicrobial resistance. Anim Biotechnol;
17(2): 111-124. 2006.
· Hardman J.G. et Limbird L.E. Les
bases pharmacologiques de l'utilisation des medicaments. 9éme
édition. Nieuwegein, Pays-Bas, Mc Graw-Hill. 1069-1098.
1998.
· Hart C.A. Klebsiella,
Citrobacter, Enterobacter and Serratia spp. Principles and
practice of Clinical Bacteriology. England, UK: John Wiley and Sons Ltd. 2nd
ed: 377- 386. 2006.
· Hawkey P.M. Prevalence and clonality
of extended-spectrum beta-lactamases in Asia. Clin Microbiol Infect,
14 Suppl 1, 159-65. 2008.
· Hawkey P.M. Prevalence and clonality
of extended-spectrum â-lactamase in Asia clin Micr Infect; 14:
159-65. 2012.
· Hennequin C., Robin F., Cabrolier N., Bonnet
R. and Forestier C. Characterization of a DHA-1-producing
Klebsiella pneumoniae strain involved in an outbreak and role of the
AmpR regulator in virulence. Antimicrob. Agents Chemother. 56(1):
288-294. 2012.
· Hirakata Y., Matsuda J., Miyazaki Y., Kamihira
S., Kawakami S., Miyazawa Y., Ono, Y., Nakazaki N., Hirata Y., Inoue M.,
Turnidge J.D., Bell J.M., Jones R.N., Kohno S. et Participants T.S.A.P.
Regional variation in the prevalence of extended-spectrum
b-lactamase-producing clinical isolates in the Asia-Pacific region (SENTRY
1998-2002). Diagnostic Microbiology and Infectious Disease,
52, 323-329. 2005.
80
Références bibliographiques
· Humeniuk C., Arlet G., Gautier V., Grimont P.,
Labia R. and Philippon A. f3-lactamases of Kluyvera
ascorbata, probable progenitors of some plasmid-encoded CTX-M types.
Antimicrob. Agents Chemother. 46: 3045-9. 2002.
· Isendhal J., Turlej-Rogacka A., Manjuba C.,
Rodrigues A., Giske C.G. and Naucler P. Fecal Carriage of
ESBL-Producing E. coli and K. pneumoniae in Children in
Guinea-Bissau: A Hospital-Based Cross-Sectional Study. PLoS ONE,
7, e51981. 2012.
· Ito H, Arakawa Y and Ohsuka S.
Plasmid-mediated dissemination of the metallo-beta-lactamase gene
blaIMP among clinically isolated strains of Serratia
marcescens. Antimicrob Agents Chemother, 39: 824-9.
1995.
· Jacobson K.L., Cohen S.H., Inciardi J.F., King
J.H., Lippert W.E., Iglesias T. and Van Couwenberghe C.J. The
relationship between antecedent antibiotic use and resistance to
extended-spectrum cephalosporins in group I beta-lactamase-producing
organisms. Clin Infect Dis. 21(5): 1107-1113.
1995.
· Jacoby G.A. and Medeiros A.A. More
extended-spectrum f3-lactamases. Antimicrob. Agents Chemother. 35:
1697-1704. 1991.
· Jacoby G.A. and Munoz-Price L.S. The
new f3-lactamases. N Engl J Med. 352: 380391.
2005.
· Jacqueline C. and Tattevin P.
Ceftaroline, a cephalosporin with activity against methicillin
resistant Staphylococcus aureus: Experimental and clinical data,
therapeutic applications. J. Anti-infect. 14 (1): 3-10.
2012.
· Janvier A., Mérens A., Delaune D.,
Soler C. et Cavallo J.D. Portage digestif
d'entérobactéries de résistantes aux
céphalosporines de troisième génération dans une
population d'adultes jeunes asymptomatiques : évolution entre 1999 et
2009 F. Pathologie Biologie ; 59 : 97-101, 2011.
· Jarlier V., Nicolas M.H., Fournier G. and
Philippon A. Extended-broads-pectrum f3-lactamases conferring
transferable resistance to newer f3-lactam agents in Enterobacteriaceae:
hospital prevalence and susceptibility patterns. Rev Infect Dis. 10:
867-878. 1988.
· Jaurin B. and Grundstrom T. ampC
cephalosporinase of Escherichia coli K12 has a different evolutionary
origin from that of f3-lactamases of the penicillinase type. Proc Nat1 Acad
Sci. USA. 78(8): 4897-4901. 1981.
· Joly B. et Reynaud A.,
Entérobactéries : Systématique et méthodes de
diagnostic. Edition Te. 3-182. 2007.
81
Références bibliographiques
· Kado C.I. and Liu S.T. Rapid
procedure for detection and isolation of large and small plasmids. J.
Bacteriol. 145: 1365-1373. 1981.
· Kardas-Soma L., Lucet J., Pelat C.,
Perozziello A., Boëlle P., Andremont A. et Yazdanpanah Y. PADS
1-05 - Modélisation des coûts et bénéfices des
stratégies de contrôle de la transmission des
entérobactéries productrices de â-lactamases à
spectre étendu (EBLSE) dans un service de réanimation.
Médecine et Maladies Infectieuses, Volume 46, Issue 4,
Supplement 1, Page 89, June 2016.
· Kassis-Chikhani N., Vimont S., Asselat K.,
Trivalle C., Minassian B., Sengelin C., Gautier V., Mathieu D., Dussaix E. and
Arlet G. CTX-M â-lactamase-producing Escherichia coli
in longterm care facilities, France. Emerg Infect Dis ; 10:
1697-1698. 2004.
· Kenneth V.I., Rolston M.A., Jamal L., Nesher
Samuel A., Shelburne R., Issam A., Randall. In vitro activity
of ceftaroline and comparator agents against Grampositive and Gram-negative
clinical isolates from cancer patients. Intern. J. Antimicr. Agen.
2017.
· Kizilca O, Siraneci R, Yilmaz A, Hatipoglu N
et Ozturk E, Kiyak A. Risk factors for community-acquired urinary
tract infection caused by ESBL-producing bacteria in children. Pediatr
Int; 54(6):858--62. 2012.
· Kliebe C., Nies B. A., Meyer J. F.,
Tolxdoref-Neutzling R. M. et Wiedemann B. Evolution of plasmid-coded
resistance to broad-spectrum cephalosporins. Antimicrob Agents Chemother,
28, 302-7. 1985.
· Knothe H., P. Shah V. Krcmery M. Antal and
Mitsuhashi S. Transferable resistanceto cefotaxime, cefoxitin,
cefamandole and cefuroxime in clinical isolates of Klebsiella pneumoniae
and Serratia marcescens. J Infect. 11:315-317.
1983.
· Kong K.F., Schneper L. and Mathee K.
Beta-lactam antibiotics: From antibiosis to resistance and
bacteriology. APMIS. 118 (1): 1-36. 2010.
· Kumar A. and Schweizer H.P. Bacterial
resistance to antibiotics: Active efflux and reduced uptake. Adv Drug
Delivery Rev. 57: 1486-1513. 2005.
· Lahlou A., Chegri M. et L'kassmi H.
Épidémiologie et résistance aux antibiotiques des
entérobactéries isolées d'infections urinaires à
l'hôpital militaire Moulay-Ismail de Meknès I. j Ant ;
11, 90-96. 2009.
· Laupland K.B., Church D.L., Vidakocich J.,
Mucenski M. and Pitout J.D. Community-onser extended-spectrum
beta-lactamase ESBL producing Escherichia coli: Importance of
international travel. J. Infect. 57p. 2008.
82
Références bibliographiques
· Lautenbach E., Patel J.B., Bilker W.B.,
Edelstein P.H. and Fishman N.O. Extendedspectrum
f3-lactamase-producing Escherichia coli and Klebsiella
pneumoniae: risk factors for infection and impact of resistance on
outcomes. Clin Infect. 32: 1162- 1171. 2001.
· Lemaoui C.E, Layaida H, Badi A et Foudi N.
Stratégies de lutte contre la résistance aux
antibiotiques. Review article Journal des Anti-infectieux, Volume 19, Issue 1,
Pages 12-19. March 2017.
· Livermore D.M. «Beta-Lactamases
in laboratory and clinical resistance». Clin Microbiol Rev. 8(4):
557-584. 1995.
· Livermore D.M., Canton R., Gniadkowski M.,
Nordmann P., Rossolini G.M., Arlet G., Poirel L. and Woodford N.
CTX-M: changing the face of ESBLs in Europe. Journal Antimicrob
Chemother. 59(2): 165-174. 2007.
· Lonchel C., Melin P., Gangoue-Pieboji J.,
Okomo Assoumou M.C., Boreux R. et De Mol P. Extended-spectrum
beta-lactamase-producing Enterobacteriaceae in Cameroonian hospitals.
Eur J Clin Microbiol Infect Dis, 32, 79-87.
2013b.
· Lonchel C., Melin P., Gangoue-Pieboji J.,
Okomo Assoumou M.C., Boreux R. et De Mol. Prevalence and spread of
extended-spectrum f3-lactamase-producing Enterobacteriaceae in
Ngaoundere, Cameroon. Clinical Microbiology Infectious, 19,
416-420. 2013a.
· Lonchel C.M., Meex C.,
Gangoué-Piéboji J., Boreux R., Assoumoui M.C., Lelin P and de Mol
P. Proportion of extended-spectrum f3-lactamase producing
enterobacteriaceae in community setting in nagaoundere , Cameroon.
Infect. Diseas. 12: 53p. 2012.
· Luvsansharav U.O., Hirai I., Niki M., Nakata
A., Yoshinaga A., Moriyama T. and Yamamoto Y. Prevalence of fecal
carriage of extended-spectrum f3-lactamaseproducing Enterobacteriaceae among
healthy adult people in Japan. J Infect Chemother. 17(5): 722- 725.
2011.
· Martinez J.L. The role of natural
environments in the evolution of resistance traits in pathogenic bacteria.
Proc Biol Sci; 276:2521-30. 2009.
· Matthew M., Hedges R.W. and Smith J.T.
Types of f3-lactamase determined by plasmids in gram-negative
bacteria. J Bacteriol. 138(3): 657-662. 1979.
83
Références bibliographiques
· Mayer K., Opal S. and Medeiros A.
Mechanisms of antibiotic resistance. In: Mandell, Douglas and Bennett's
Principles and Practice of Infectious Diseases. 5th edition, Churchill
Livingstone. 2: 236-253. 2000.
· Mendonça N., Ferreira E., Louro D.,
Caniça M. and ARSIP Participants. Molecular epidemiology and
antimicrobial susceptibility of extended- and broad-spectrum
â-lactamaseproducing Klebsiella pneumoniae isolated in Portugal.
Int J Antimicrob Agents. 34: 29-37. 2009.
· Mérabaud M.I.
Entérobactéries à BLSE en pédiatrie en
1996. Thèse n°10303. 2003.
· Messai Y., Iabadene H., Benhassine T.,
Alouache S., Tazir M., Gautier V., Arlet G. et Bakour R. Prevalence
and characterization of extended-spectrum b-lactamases in Klebsiella
pneumoniae in Algiers hospitals (Algeria). Pathologie Biologie,
56, 319-325. 2008.
· Metuor Dabire A.
Caractérisations moléculaire et cinétique des
types de Ji-lactamases à spectre élargi (BLSE) de souches
bactériennes collectées au Centre Hospitalier Universitaire
Pédiatrique Charles De Gaulle (CHUP-CDG) de Ouagadougou. Biologie
Moléculaire / Enzymologie thèse de doctorat unique,
Université de Ouagadougou. 149p. 2014.
· Naas T. et Vaux S. Bactéries
hautement résistantes aux antibiotiques : épidémiologie
mondiale et française. 44-47. 2012.
· Naas T., Cuzon G., Villegas M.V. et
al. Genetic structures at the origin of acquisition of the ß-lactamase
blaKPC gene. Antimicr. Agen. Chemo. 52 : 63-1257.
2008.
· Nadmi H., Elotmani F., Talmi M., Zerouali K.,
Perrier Gros C. et Timinouni M. Profil de résistance aux
antibiotiques des entérobactéries uropathogènes
communautaires à El Jadida (Maroc). Journal Médecine et
maladies infectieuses ; 40 : 303-305, 2010.
· Nauciel C. et Vildé J.L.
Bactériologie médicale. 2éme édition.
Masson. Paris. 20-126. 2005.
· Nedjai S., Barguigua A., Djahmi N., Jamali L.,
Zerouali K., Dekhil M. and Timinouni M. Prevalence and
characterization of extended spectrum beta-lactamase-producing Enterobacter
cloacae strains in Algeria. J Infect Dev Ctries, 7,
804-811. 2013.
· Neulier C., Birgand G., Ruppé E.,
Armand-Lefèvre L., Lolom I., Yazdanpanah Y., Lucet J.C. et Andremont A.
Enterobacteriaceae bacteremia: Risk factors for
84
Références bibliographiques
ESBLPE. Médecine and Maladies Infectieuses,
Volume 44, Issue 1, 32-38, January 2014.
· Neuwirth C., Siebor E., Duez J.M.,
Péchinot A. and Kazmierczak A. Imipenem resistance in
clinical isolates of Proteus mirabilis associated with alterations in
penicillinbinding proteins. J Antimicrob Chemother. 36(2): 335-342.
1995.
· Nordmann P, Boulanger A.E. and Poirel L.
NDM-4 metallo-ss-lactamase with increased carbapenemase activity from
Escherichia coli. Antimicrob Agents Chemother. 12 Jan
2012.
· Nordmann P, Naas T. and Poirel L.
Global spread of Carbapenemase-producing Enterobacteriaceae. Emerg
Infect Dis; 17: 1791-8. 2011.
· Nordmann P. et Carrer A. Les
carbapénèmases des entérobactéries, Arch.
Péd. 16 (4) : S154-162. 2010.
· Nordmann P., Cuzon G. and Naas T. The
real threat of Klebsiella pneumoniae carbapenemase-producing bacteria.
Lancet. Infect. Dis. 9: 228-36. 2009.
· Nordmann P., Dortet L. and Poirel L.
Carbapenem resistance in Enterobacteriaceae: here is the storm!
Tren. Mol. Med. 18 (5): 263-272. 2012.
· Okalla Ebongue C., Dongmo Tsiazok M, Nda
Mefo'o J.P., Ngaba N.P., Beyiha G. et Adiogo D. Evolution of
antibiotic resistance of Enterobacteriaceae isolated at the Douala General
Hospital from 2005 to 2012. Pan Afr Med J; 20: 227.
2015.
· Papanicolaou G.A., Medeiros A.A., and Jacoby
G.A. Novel plasmid mediated betalactamase (MIR-1) conferring
resistance to oxyimino-and alpha-methoxy beta-lactams in clinical isolates of
Klebsiella pneumoniae. Antimicrob. Agents Chemother. 34:
2200-2209. 1990.
· Paterson D.L. and Bonomo R.A.
Extended-spectrum beta-lactamases: a clinical update. Clin
Microbiol Rev. 18: 657-686. 2005.
· Peery J., Staley J.T et Lory S.
Microbilogie .Edition Dunod. 423 p. 2004.
· Peirano G., Van Greuneb C.H.J. and Pitout
J.D.D. Characteristics of infections caused by extended-spectrum
â-lactamase-producing Escherichia coli from community hospitals
in South Africa. Diagnostic Microbiology and Infectious Disease, 69,
449-453. 2011.
85
Références bibliographiques
· Pepperell C., Kus J.V., Gardam M.A., Humar A.
and Burrows L.L. Low-Virulence Citrobacter Species Encode
Resistance to Multiple Antimicrobials. Antimicrob. Agents Chemother.
46(11): 3555-3560. 2002.
· Philippon A. and Arlet G.
f3-Lactamases de bacilles à Gram négatif : le mouvement
perpétuel ! Ann Biol Clin. 64(1): 37-51.
2006.
· Philippon A.
Entérobactéries des f3-lactamines. Biol. méd. 3
(4) : 1-18. 2008.
· Philippon A. et arlet G.
Entérobactéries et bétalactamine : Phénotypes de
résistance naturelle. Pathol. Biol. 60: 112-126.
2012.
· Philippon A., Arlet G. and Jacoby G.A.
Plasmid-determined AmpC-type f3-lactamases. Antimicrob. Agents
Chemother. 46: 1-11. 2002.
· Pietsch M., Eller C., Wendt C., Holfelder M.,
Falgenhauer L., Fruth A., Grössl T., Leistner R., Valenza G., Werner G.,
Pfeifer Y. RESET Study Group. Molecular characterisation of
extended-spectrum f3-lactamase (ESBL)-producing Escherichia coli
isolates from hospital and ambulatory patients in Germany. Veterinary
Microbiology, Volume 200, Pages 130-137. February
2017.
· Pitout J.D., Thomson K.S., Hanson N.D.,
Ehrhardt A.F., Moland E.S.et Sanders C. C. Beta-Lactamases responsible
for resistance to expanded-spectrum cephalosporins in Klebsiella
pneumoniae, Escherichia coli, and Proteus mirabilis isolates
recovered in South Africa. Antimicrob Agents Chemother, 42,
1350-4. 1998.
· Poirel L, Héritier C and Nordmann
P. Chromosome-encoded ambler class D beta-lactamase of Shewanella
oneidensis as a progenitor of carbapenem-hydrolyzing oxacillinase.
Antimicrob Agents Chemother; 48:348-51. 2004.
· Poirel L, Héritier C, Tolun V et
Nordmann P. Emergence of oxacillinase-mediated resistance to imipenem
in Klebsiella pneumoniae. Antimicrob Agents Chemother; 48;
1522. 2004.
· Poirel L., Pitout J.D. and Nordmann
P. Carbapenemases: Molecular diversity and clinical consequences.
Fut Micr; 2: 12-501. 2007.
· Poole K. "Resistance to beta-lactam
antibiotics." Cell Mol Life Sci. 61(17): 2200-2223.
2004.
86
Références bibliographiques
· Porres-Osante N., Dupont H., Torres C.,
Ammenouche N., De-Champs C. and Mammeri H. Avibactam activity against
extended-spectrum AmpC ß-lactamases. J. Antimicr. Chemo.
2014.
· Queenan A.M., Bush K. Carbapenemases:
The versatile beta-lactamases. Clin Micr Rev. 20: 440-58.
2007.
· Rahal K., Belouni R. and Benslimani A.
Standardisation de l'antibiogramme en médicine humaine à
l'échelle nationale. Rec de L'OMS. 4éme édition.
Algérie. 46-52. 2005.
· Rakotovao-Ravahatra Z.D., Randriatsarafara
F.M., Rasoanandrasana S., Raverohanta L. et Rakotovao A.L.
Phénotypes de résistance des souches d'Escherichia coli
responsables d'infection urinaire au laboratoire du Centre
Hospitalo-Universitaire de Befelatanana Antananarivo. Pan African Medical
Journal ; 26.166.11828. 2017.
· Recchla G.D and Hall R.M. Origins of
the mobile gene cassettes found in integrons. Trends Microbiol; 5(10):
389-394. 1997.
· Robin F., Gibolda l. et Bonneta R.
Résistance naturelles et acquise aux f3-lactamine chez les
entérobactéries : Comment les identifier en pratique quotidienne.
franco labos. 445 : 47-57. 2012.
· Rodriguez-Bano J., Lopez-Cerero L., Navarro
M.D., Diaz de Alba P. and Pascual A. Faecal carriage of
extended-spectrum beta-lactamase-producing Escherichia coli:
prevalence, risk factors and molecular epidemiology. J Antimicrob
Chemother. 62(5): 1142-1149. 2008b.
· Rodriguez-Villalobos M. et Struelens
M.J. Résistance bactérienne par f3-lactamase à
spectre étendu : Implication pour le réanimateur.
Réanimation. 15 : 205-2013. 2003.
· Rodriguez-Villalobos M. et Struelens,
M.J. Résistance bactérienne par f3-lactamases à
spectre étendu: implications pour le réanimateur. Rev
Réanimation 15. (3): 205-213. 2006.
· Rossolini G.M., D'Andrea M.M. and Mugnaioli C.
The spread of CTX- M- type extended- spectrum beta- lactamases. Clin
Microbiol Infect 14 Suppl 1:33- 41. 2008.
· Rubin M.A. and Samore M.H.
Antimicrobial Use and Resistance. Curr Infect Dis Rep. 4:
491-497. 2002.
87
Références bibliographiques
· Ruppé E., Woerther P.l., Diop A.M.,
Da-costa A. et Costa Arlet G. Carriage of CTX-M-15 producing
Escherichia coli isolates amoung children living in a remote in
Senegal. Anti. Agen. Chem. 53: 7-3135.
2009.
· Schwaber M.J and Carmeli Y. Mortality
and delay in effective therapy associated with extended-spectrum beta-lactamase
production in Enterobacteriaceae bacteraemia: a systematic review and
meta-analysis. J Antimicrob Chemother. 60: 913-920.
2007.
· Schwarz S. and Chaslus-Dancla E. "Use
of antimicrobials in veterinary medicine and mechanisms of resistance." Vet
Res. 32(3-4): 201-225. 2001.
· Seid J. and Asrat D. Occurrence of
extended spectrum â-lactamase enzymes in clinical isolates of
Klebsiella species from Harar region, eastern Ethiopia. Acta
Tropica 95, 143148. 2005.
· Sekhsokh Y., Chadli M. et El Hamzaoui S.A.
Fréquence et sensibilité aux antibiotiques des
bactéries isolées dans les urines. Méd et Mal inf
; 38 : 324-327. 2008.
· Singelton P. Bactériologie
pour la médcine, la biologie et la biotechnologie .6éme
édition. Dunod. Paris. 40-316. 2005.
· Sire J.M., Nabeth P., Perrier-Gros-Claude
J.D., Bahsoun I., Siby T., Macondo E.A., Gaye-Diallo A., Guyomard S., Seck A.,
Breurec S. and Garin B. Antimicrobial resistance in outpatient
Escherichia coli urinary isolates in Dakar, Senegal. J Infect Dev
Ctries, 1, 263-8. 2007.
· Sirot J. Prospective survey of
colonization and infection caused by expandedspectrum-beta-lactamase-producing
members of the family Enterobacteriaceae in an intensive care unit. J Clin
Microbiol. 27(12): 2887-2890. 1989.
· Snyder L. and Champness W. Molecular
genetics of bacteria. Washington, D.C. ASM Press.
2007.
· Soge O.O., Queenan A.M., Ojo K.K., Adeniyi
B.A. et Roberts M.C. CTX-M-15 extended-spectrum (beta)-lactamase from
Nigerian Klebsiella pneumoniae. J Antimicrob Chemother,
57, 24-30. 2006.
· Sood S. and Gupta R. Antibiotic
resistance pattern of community acquired uropathogens at a tertiary care
hospital in Jaipur, Rajasthan. Indian J Community Med; 37(1):39-44.
2012.
· Spratt B.G., Zhang Q.Y., Jones D.M.,
Hutchison A., Brannigan J.A. and Dowson C.G. Recruitment of a
penicillin-binding protein in gene from Neisseria flavescens
88
Références bibliographiques
during the emergence of penicillin resistance in
Neisseria meningitidis. Proc Natl Acad Sci. USA. 86(22):
8988-8992. 1989.
· Storberg V. ESBL-producing
Enterobacteriaceae in Africa - a non-systematic literature review of
research published 2008-2012. Infections Ecology and Epidemiology,
4, 1-16. 2014.
· Stürenburg E. and Dietrich M.
Extended spectrum beta- lactamases implication for the clinical
microbiology, therapy, and infection control. J Infect. 47: 273-295.
2003.
· Tandé D., Jallot N., Bougoudogo F.,
Montagnon T., Gouriou S. and Sizun J. Extended-Spectrum 3-Lactamase-
Producing Enterobacteriaceae in Malian Orphanage. Emerging
Infectious Diseases, 15, 472-474.
2009.
· Tandé D., Jallot N., Bougoudogo F.,
Montagnou T., Gouriou S. and Sizun J. Extended- spectrum
béta-lactamase producing enterobacteriacea isolates in Mexico.
Micr Drug Resis. 17: 497-505.
2005.
· Tansarli G.S., Poulikakos P., Kapaskelis A.
and Falagas M.E. Proportion of extended-spectrum beta-lactamase
(ESBL)-producing isolates among Enterobacteriaceae in Africa:
evaluation of the evidence--systematic review. J Antimicrob Chemother,
69, 1177-84. 2014.
· Thibaut S., Marquet A., Collet C, Grandjean
G., Boutoille D., Caillon J. Épidémiologie des
bactériuries des souches d'infections urinaires communautaires :
comparaison entre les patients vivant à domicile et en
établissements d'hébergements pour personnes âgées
dépendantes (EHPAD) M. Réseau Med Qual, CHU de Nantes EN
France. J Med Mal; 03.072. 2017.
· Thomas C.M and Nielsen K.M.
Mechanisms of, and barriers to, horizontal gene Transfer between
bacteria. Naature Review Microbiology, 3: 711-721.
2005.
· Thomson K.S. and Moland E.S. The new
3-lactamases of Gram negative bacteria at the dawn of the new millennium.
Microbes Infect. 2: 1225-1235. 2000.
· Tiouit D, Naim M. et Amhis W.
Médecine du Maghreb 2001 n°91 : Traitement antibiotique des
infections urinaires Page 35 à 38. 2001.
· Touati A., Medboua C., Touati D., Denine R.,
Brasme L. and de Champs C. CTXM-15- producing Enterobacteriaceae
isolates causing bloodstream infections at the Beni-Messous hospital in Algeirs
(Algeria). Int Res J Microbiol. 3: 181-185. 2012.
89
Références bibliographiques
· Villegas M.V., Kattan J.N., Quinteros M.G.,
Casellas J.M. Prevalence of extended-spectrum â-lactamase in
South America. Clin Micr Infect. 14: 8-154. 2008.
· Vodovar D, Marcad2 G, Raskine L, Malissin I et
Mégarbane B. Entérobactéries productrices de
bêta-lactamases a spectre élargi. Rev Méd Int,
Vol:34, issue 11 p:687693. Nov 2013.
· Vora S. et Auckenthaler R. Que
signifie «bêtalactamases à spectre élargi» en
pratique?. Rev Med Suisse. 5: 1991-1994.2009.
· Walsh C. Antibiotics: actions,
origins, resistance. American Society for Microbiology press.
Washington. 2003.
· Walsh T.R. Clinically signifi cant
carbapenemases: an update. Curr Opin Infect Dis; 21:367-71.
2008.
· Walsh T.R. Combinatorial genetic
evolution of multiresistance. Curr Opin Microbiol 9:476-82.
2006.
· WEBER Ph. Etat actuel de la
sensibilité à la ciprofloxacine des bactéries
isolées en pratique en ville: résultats d'une enquête
multicentrique. Méd Mal Infect ; 23 :342-7.
1993.
· Weldhagen G.F., Poirel L. and Nordmann P.
Ambler class A extended-spectrum â-lactamases in Pseudomonas
aeruginosa: novel developments and clinical impact. Antimicrob. Agents
Chemother. 47: 2385-2392. 2003.
· Wiener J., Quinn J.P., Bradford P.A., Goering
R.V., Nathan C., Bush K. and Weinstein R.A. Multiple
antibiotic-resistant Klebsiella and Escherichia coli in
nursing homes. JAMA. 281(6): 517-523. 1999.
· Winokur P.L., Canton R., Casellas J.M. et
Legakis N. Variations in the Prevalence of Strains Expressing an
Extended-Spectrum b-Lactamase Phenotype and Characterization of Isolates from
Europe, the Americas, and the Western Pacific Region. Clinical Infectious
Diseases 32, S94-S103. 2001.
· Woerther P.-L., Angebault C., Jacquier H.,
Hugede H.C., Janssens A.C., Sayadi S., El Mniai A., Armand-Lefévre L.,
Ruppé E., Barbier F., Raskine L., Page A.L., Rekeneire N. and Andermont
A. Massive Increase, Spread, and Exchange of Extended Spectrum
b-Lactamase-Encoding Genes Among Intestinal Enterobacteriaceae in
Hospitalized Children With Severe Acute Malnutrition in Niger. Clinical
Infectious Diseases 53, 677-685.
2011.



