|
SCHOOL OF PUBLIC HEALTH
COLLEGE OF HEALTH SCIENCES
UNIVERSITY OF GHANA
By
JEAN-PIERRE KASEREKA MAKELELE (Mr.Dr)
THIS DISSERTATION IS SUBMITTED
TO THE SCHOOL OF PUBLIC HEALTH,
UNIVERSITY OF GHANA, LEGON
IN PARTIAL FULFILMENT OF THE REQUIREMENT FOR
THE AWARD OF MASTER OF PUBLIC HEALTH DEGREE
AUGUST 2005
bb
KNOWLEDGE AND PERCEPTION TOWARDS PREMARITAL COUNSELING
AND TESTING ON HUMAN IMMUNODEFICIENCY VIRUS INFECTION AMONG UNMARRIED YOUNG
ADULTS IN KINTAMPO DISTRICT OF GHANA

DEDICATION
To my wife Lucie Tshongo Kavira Makelele, that I missed too
much and who reciprocally suffered patiently my long absence, for your motherly
cordial care you provided to our children during my study leave, for your
caring love and mutual understanding,
To my children Amos Makelele M'Yisa, Dieu-Exauce Makelele
Vutokii, Miriam Makelele Mukiranya, Esther Kavuo Makelele and to you all my
dependants for the suffering you faced from the lack of fatherly care due to
my studies, and for your prayerful supports , your encouragement , your good
wishes and warm regards to your father,
To my whole family members, especially my Mother Kahindo
Mukiranya who kept praying for me throughout this hard course,
To every body who has ever supported me somehow; either
morally, materially or financially towards the attainment of the current
educational level and the successful end of this course,
To all of you, my beloved Brothers and Sisters,
Through Jesus Christ who strengthens us,
I dedicate this piece of work.
AKNOWLEDGEMENT
I acknowledge a grant from my Sponsor Word Council of Churches
(COE-WCC)/Switzerland which made it possible to achieve my study dream and the
Union Evangelical Mission (UEM-VEM)/Germany for the additional financial
support which solved my life hardship in Ghana, thereby enabling me to produce
this work.
I thank the Director Prof. Isabella A. Quakyi and the entire
staff of School of Public Health of University of Ghana, Legon, for the entire
knowledge they insistently and consistently imparted in us and for their moral
support and encouragement.
I thank Dr Seth Owusu- Agyei and Mr. Alfred.A.D. OBUOBI, my
Academic Supervisors, who, despite their busy work schedule, diligently and
profoundly assisted me in planning, conducting, correcting and enriching this
work; and to Dr E.T.ADJASE, my field Supervisor, for approving the study topic,
for his unlimited constructive advice as well as fatherly support which made my
stay in Kintampo very enjoyable and comfortable, and finally for the training
care which we received while on the field. This has successfully provided me
enough field knowledge, skills and experiences.
I thank the entire staffs of Kintampo District Health
Directorate, of Kintampo Rural Health Training School (KRHTS) and of Kintampo
Health Research Centre (KHRC) for all their fruitful, caring, supervisory, and
skilled expertise and support during this study,
Finally I thank my course mates, my key informants and all
respondents for their generous contribution towards the achievement of this
work.
TABLE OF CONTENTS
|
Pages
|
|
DECLARATION...........................................................................
|
ii
|
|
DEDICATION..............................................................................
|
iii
|
|
AKNOWLEDGEMENT...................................................................
|
iv
|
|
TABLE OF
CONTENTS..................................................................
|
v
|
|
ABBREVIATIONS...........................................................................
|
ix
|
|
ABSTRACT..................................................................................
|
x
|
|
LIST OF DIAGRAM, MAP, FIGURES AND TABLES
|
Xii
|
|
|
|
Chapter One
INTRODUCTION.......................................
|
1
|
|
|
|
I.1. BACKGROUND
INFORMATION..............................................
|
1
|
|
I.1.1. Marriage and its reproductive health
implication.......................
|
1
|
|
I.1.2. Scope and objectives of premarital
Screening............................
|
2
|
|
I.1.3. Study
Area...................................................................
|
4
|
|
I.2. STATEMENT OF THE
PROBLEM.............................................
|
7
|
|
I.3. CONCEPTUAL FRAMEWORK: PROBLEM ANALYSIS DIAGRAM...
|
10
|
|
I.4. RATIONALE OF THE
STUDY.................................................
|
11
|
|
I.5. GOAL AND OBJECTIVES OF THE
STUDY................................
|
12
|
|
|
|
Chapter Two LITTERATURE
REVIEW.......................................
|
14
|
|
|
|
2.0. Definition of concepts
|
14
|
|
2.1. Premarital examination in Ghana and in Kintampo
District..........
|
14
|
|
2.2. HIV-AIDS situation in west Africa and
Ghana.........................
|
16
|
|
2.2.1. In West
Africa..................................................
|
16
|
|
2.2.2. In
Ghana.........................................................
|
17
|
|
2.3. HIV VCT and premarital HIV counseling and
testing
|
20
|
|
2.4. Procurement of Materials for VCT
|
23
|
|
2.5. Factors influencing willingness to undergo HIV
PCT
|
23
|
|
2.6. Reasons for undergoing HIV VCT
|
24
|
|
2.7. Barriers to HIV VCT/PCT
|
24
|
|
2.8. Marriage between HIV discordant or HIV
seropositive couples
|
24
|
|
|
|
Chapter Three
METHODOLOGY..........................................
|
25
|
|
|
|
3.1. STUDY DESIGN AND STUDY POPULATION
...........................
|
25
|
|
3.2. VARIABLES UNDER
STUDY.................................................
|
25
|
|
3.3. DATA COLLECTION TECHNIQUES AND TOOLS
......................
|
28
|
|
3.3.1. Data Collection
Techniques...........................................
|
28
|
|
3.3.2. Data Collection
Tools..................................................
|
28
|
|
3.4.
SAMPLING........................................................................
|
28
|
|
3.4.1. Sample size calculation
..............................................
|
28
|
|
3.4.2. Sampling method
......................................................
|
29
|
|
3.5. DATA
COLLECTION............................................................
|
32
|
|
3.6. DATA PROCESSING AND
ANALYSIS.....................................
|
34
|
|
3.6.1. Qualitative data
...........................................................
|
34
|
|
3.6.2. Quantitative data
.........................................................
|
34
|
|
3.6.2.1. Data quality control
.........................................
|
34
|
|
3.6.2.2. Data presentation and
statistical analysis .................
|
34
|
|
3.6.2.3. Score allocation for level
of knowledge and perception
towards HIV
PCT.......................................
|
35
|
|
3.7. SOME ETHICAL
CONSIDERATIONS.......................................
|
35
|
|
3.8. LIMITATION OF THE
STUDY................................................
|
36
|
|
3.9. RETRO INFORMATION AND DISSEMINATION OF
FINDINGS...........................................................................
|
37
|
|
|
|
Chapter Four
FINDINGS.......................................................
|
38
|
|
|
|
4. 1. SOCIO-DEMOGRAPHIC CHARACTERISTICS OF
RESPONDENTS..................................................................
|
38
|
|
4.1.1. Distribution of respondents by age and
sex.............................
|
38
|
|
4.1.2. Educational background of respondents
...............................
|
39
|
|
4.1.3. Religion, ethnic group and occupation
background of
respondents................................................................
|
40
|
|
4.2. PREMARITAL SEX HISTORY AND HIV-AIDS RISK FACTORS
AMONG SURVEYED
RESPONDENTS.....................................
|
41
|
|
4.3. GENERAL AWARENESS AND KNOWLEDGE OF RESPONDENTS
ON HIV/AIDS, VCT AND HIV
PCT..........................................
|
44
|
|
4.4. SCORE OBTAINED ON AWARENESS AND KNOWLEDGE OF
RESPONDENTS ON HIV
PCT................................................
|
49
|
|
4.5. GENERAL PERCEPTION OF RESPONDENTS TOWARDS HIV
PCT.
|
52
|
|
4.6. SCORE OBTAINED ON PERCEPTIONS OF RESPONDENTS
TOWARDS HIV
PCT............................................................
|
55
|
|
4.7. RELATIONSHIP BETWEEN SCORE OF KNOWLEDGE AND
SCORE OF PERCEPTION AMONG
RESPONDENTS....................
|
57
|
|
4.8. FACTORS INFLUENCING PERCEPTION OF THE NEED OF
HIV
PCT
SERVICES..................................................................
|
58
|
|
4.9. FACTORS INFLUENCING WILLINGNESS TO UNDERGO HIV
PCT..................................................................................
|
59
|
|
4.10. DEDUCTION OF PROBABILITY FOR RESPONDENTS TO
PERCEIVE THE NEED OF HIV PCT SERVICE AND TO INTE
ND
UNDERGOING HIV
PCT................................................
|
60
|
|
4.11. PREFERENCE TO UNDERGO HIV VCT FOR MARITAL REASON
OR
NOT........................................................................
|
61
|
|
4.12. BARRIERS TO HIV PCT ACCEPTANCE AND IMPLEMENTATION
IN KINTAMPO
DISTRICT...................................................
|
61
|
|
4.13. KEY ISSUES TOWARDS HIV PCT HEALTH PRACTICE
IN KINTAMPO
DISTRICT................................................
|
64
|
|
4.13.1. Views on frequency of HIV test before
marriage among
would-be
couples...................................................
|
64
|
|
4.13.2. Views of respondents on who should send
would-be couples at
the hospital for HIV
PCT....................................................
|
66
|
|
4.13.3. Views on to who the HIV test result
should communicated
after a PCT
session.......................................................
|
66
|
|
4.13.4. Ways to promote HIV PCT in K'po
district.........
|
67
|
|
4.13.5. Ways to create easier accessibility to
HIV PCT
in K'po
district........................................................
|
68
|
|
4.13.6. Ways to make HIV PCT more effective,
acceptable and
attractive for young people in
K'po district........................
|
69
|
|
4.13.7. Health facilities where HIV PCT centre
should be established in
K'po
district............................................................
|
70
|
|
4.14. POSSIBLE DECISIONS THAT WOULD-BE COUPLES ARE MORE
LIKELY TO MAKE GIVEN DIFFERENT SCENARIOS OF
HIV
TEST
RESULTS.....................................................................
|
71
|
|
4.15. POINTS OF VIEW OF RESPONDENTS ABOUT MARRIAGE
BETWEEN DISCORDANTS COUPLES AND HIV INFECTED
COUPLES............................................................................
|
72
|
|
|
|
Chapter Five
DISCUSSION.....................................................
|
74
|
|
|
|
5.1. PREMARITAL SEX HISTORY AND HIV-AIDS RISK FACTORS
AMONG SURVEYED
RESPONDENTS....................................
|
74
|
|
5.2. KNOWLEDGE AND PERCEPTION OF RESPONDENTS TOWARDS
HIV
PCT...........................................................................
|
75
|
|
5.2.1. Indicators on awareness and knowledge on
HIV PCT...............
|
75
|
|
5.2.2. Level of knowledge on HIV
PCT.......................................
|
79
|
|
5.2.3. Indicators of perception of respondents
towards HIV PCT.........
|
81
|
|
5.2.4. Relationship between level of knowledge
and level of perception
of respondents towards HIV
PCT.......................................
|
88
|
|
5.3. FACTORS INFLUENCING PERCEPTION OF THE NEED OF
HIV
PCT S
ERVICES..................................................................
|
89
|
|
5.4. FACTORS INFLUENCING WILLINGNESS TO UNDERGO HIV PCT
|
92
|
|
5.5. PREFERENCE TO UNDERGO HIV VCT FOR MARITAL REASON
OR
NOT.........................................................................
|
97
|
|
5.6. BARRIERS TO HIV PCT ACCEPTANCE AND IMPLEMENTATION
IN KINTAMPO
DISTRICT...................................................
|
98
|
|
5.7. KEY ISSUES TOWARDS HIV PCT HEALTH PRACTICE IN
KINTAMPO
DISTRICT.......................................................
|
102
|
|
5.7.1. Views on frequency of HIV test before
marriage among
would-be
couples......................................................
|
102
|
|
5.7.2. Views on who should send would-be couples
at the
hospital for HIV
PCT.............................................
|
103
|
|
5.7.3. Views of respondents on to who the HIV
test result should
communicated after a PCT
session....................................
|
104
|
|
5.7.4. Ways to promote HIV PCT in K'po
district............................
|
105
|
|
5.7.5. Ways to create easier accessibility to
HIV PCT in K'po district..
|
108
|
|
5.7.6. Ways to make HIV PCT more effective,
acceptable
and attractive for young people in K'po
district........................
|
109
|
|
5.7.7. Health facilities where HIV PCT centre
should be established in
K'po
district............................................................
|
111
|
|
5.8. POSSIBLE DECISIONS THAT WOULD-BE COUPLES ARE MORE
LIKELY TO MAKE GIVEN DIFFERENT SCENARIOS OF HIV
TEST
RESULTS AND POINT OF VIEW OF RESPONDENTS ABOUT
MARRIAGE BETWEEN DISCORDANTS COUPLES
AND HIV INFECTED
COUPLES................................................
|
112
|
|
|
|
Chapter Six CONCLUSION AND RECOMMENDATIONS
................
|
114
|
|
|
|
REFERENCES...........................................................................
|
123
|
|
|
|
ANNEX 1. QUESTIONNAIRE FOR THE
SURVEY.................................
|
A
|
|
ANNEX 2a: INTERVIEW GUIDE FOR HEALTH CARE
PROVIDERS.........
|
H
|
|
ANNEX 2b: IN-DEPHT INTERVIEW GUIDE FOR RELIGION
LEADERS.....
|
J
|
|
ANNEX 3: FOCUS GROUP DISCUSSION GUIDE
(FGDG)........................
|
L
|
|
ANNEX 4. DESCRIPTION OF VARIABLES UNDER STUDY
AND SCORING
SCALE....................................................................
|
N
|
ABBREVIATIONS
AIDS : Acquired Immuno deficiency syndrome
BCC : Behavior change communication
CI : Confidence Interval
DA : District Assembly
DDHS : Director of District health service
DHD : District Health Directorate
DHMT : District Health Medical Team
ECC/CBCA : Eglise du Christ au Congo, Communauté
Baptiste au Centre de
l'Afrique
FGD : Focus group discussion
GDHS : Ghana Demographic Health Survey
GES : Ghana Education Service
HIV : Human immuno deficiency virus
IDI : In-depth Interview or In-depth Interviewee
IEC : Information, Education and Communication.
JSS : Junior secondary school
K'po : Kintampo
KDH : Kintampo District Hospital
KDSS : Kintampo Demographic Surveillance Survey
KHRC : Kintampo Health Research centre
MPH : Master of Public Health
MTCT : Mother-to-child transmission (of HIV)
NA : Not applicable
NACP : National AIDS Control Program
NGO : Non Governmental Organization
NK : Not known or don't know
OAU : Organization of African Union
PCT : Premarital (prenuptial) counseling and testing
PLWA : People living with AIDS
PLWHA : Person living with HIV/AIDS
PMTCT : Prevention of Mother-to-child transmission (of
HIV)
PMTCT : Prevention of mother-to-child transmission of HIV
RA : Research assistants (field interviewers).
SD : Standard deviation
SE : Standard error
SSS : Senior secondary school
STD : Sexually transmitted diseases
STI : Sexually transmitted infection
UG : University of Ghana
UNAIDS : United Nation-Acquired Immuno Deficiency syndrome
UNDP : United Nation Development Program
UNPFA : United Nation Population Fund
VCT : Voluntary counseling and testing
WHO : World Health organization
ABSTRACT
HIV PCT, as part of VCT, is recognized worldwide as a core
strategy of limiting the spread of HIV in new couples and their offspring. The
study on «Knowledge and perception towards PCT on HIV infection among
unmarried young adults in Kintampo District» was one of the preliminary
studies needed for the implementation of VCT services in the District.
AIM: The general objective of the study was
to generate useful information on current level of knowledge and perception of
unmarried young adults towards HIV premarital counseling and testing (HIV PCT)
in order to predict their acceptance and behaviours towards utilization of such
service and to deduce appropriate program/policy for intervention in the
relevant area.
METHODS: We analyzed data from a cross
sectional survey among 150 unmarried young adults between 15 and 30 years old
and from FGDs and IDIs. The survey was carried out in 3 of the 8 sub-districts
in the district. Compounds where to find respondents were randomly selected and
an interviewer-administered questionnaire was used. We allocated scores of
knowledge on HIV PCT and of perception towards HIV PCT to given answers. We
also applied 2 Logit models to determine predictors of willingness to undergo
HIV PCT and of perceived need towards HIV PCT service.
FINDINGS: Out of 150 respondents, 71% lived
in urban and 29% in rural areas. Respondents were of a mean age of 21.0 years
(SD 4.48), the majority of them (76%) being aged between 15-24 years. The sex
ratio was 104 [little predominance of males (51%)]. In general 97% of
respondents had Good Knowledge on HIV PCT, with 41.3% showing
Adequate good Knowledge, versus 55.7% showing Average good
knowledge on HIV PCT. Only 3% of respondents showed Poor
knowledge on HIV PCT. The entire totality (100%) of respondents in both
sexes had Adequate positive perception towards HIV
PCT. There was a significant weak positive linear relationship between level of
knowledge and level of perception (p-value 0.007). Willingness to undergo HIV
PCT was strongly positively associated with readiness of a respondent to know
and accept his/her HIV result (p<0.001). Willingness to undergo HIV PCT was
negatively associated with age, post-primary educational level, being student,
having ever had premarital sex, perceiving the need of HIV PCT services and
suggestion that HIV PCT should be provided free of charge, with no significant
associations. Willingness to undergo HIV PCT was slightly positively associated
with Akan & Mo Ethnic groups, urban residence, being Christian and female,
level of knowledge and level of perception towards HIV PCT and suggestion of
confidentiality in PCT services, with no significant associations.
CONCLUSION: In view of the study findings
showing good knowledge and adequate positive perception towards HIV PCT among
unmarried young adults, HIV PCT service for would-be couples is needed and
feasible at present in Kintampo District. Majority of unmarried young adults
showed positive acceptance towards utilization of such service.
Not all populations of unmarried young groups have an equal
likelihood of accepting to undergo HIV PCT. Therefore Public health
intervention (BCC/IEC) in the district on HIV PCT should be adapted
specifically for each population segment and address perceived barriers to HIV
PCT. A policy document is needed to specify the scope and procedures of
premarital examinations in light of the findings in this study.
KEY WORDS: HIV/AIDS; Kintampo District;
marriage, premarital counseling and testing (PCT), unmarried young
adults, would-be couples.
|
LIST OF DIAGRAM, MAP, FIGURES AND TABLES
|
Page
|
|
|
|
DIAGRAMS
|
|
|
|
|
Diagram 1: Conceptual framework: problem analysis diagram
.................................................................
|
10
|
|
Diagram 2: Relationship between variables: assumptions of
logit models....................................
|
27
|
|
|
|
FIGURES
|
|
|
|
|
Figure 0: Map of Kintampo District showing Centroids of study
(villages/Towns) and roads network...
|
32
|
|
Figure 1: Distribution of surveyed respondents by age and
sex..................................................
|
39
|
|
Figure 2: Distribution of surveyed respondents by educational
level and sex.................................
|
40
|
|
Figure 3: Distribution of Respondents by Religion, Ethnic group
and Occupation...........................
|
41
|
|
Figure 4: Distribution of respondents by sex and age at first
sexual intercourse..............................
|
42
|
|
Figure 5: Distribution of respondents according to their scores
of knowledge on HIV PCT................
|
51
|
|
Figure 6: Distribution of Respondents by location and score of
knowledge on HIV PCT...................
|
52
|
|
Figure 7: Distribution of respondents by sex and their score of
perception towards HIV PCT..............
|
56
|
|
Figure 8: Distribution of respondents by sex and suggestion on
the required number of HIV tests to
undergo before
marriage....................................................................................
|
65
|
|
Figure 9: Distribution of respondents according to their choices
on the person who should send would-
be couples for HIV
PCT...................................................................................
|
66
|
|
Figure 10: Suggestion of respondents about to whom the HIV test
result should be communicated after
a PCT
session..............................................................................................
|
66
|
|
Figure 11: Frequency of ways suggested by respondents to make
easier accessibility to HIV PCT in the
District......................................................................................................
|
68
|
|
Figure 12: Trend of possible decisions on marriage that
respondents are more likely to make given
different scenarios of HIV test results after a
HIV PCT session....................................
|
71
|
|
Figure 13: Points of view of respondents about marriage
between HIV discordant would-be couples
and both infected would-be
couples....................................................................
|
73
|
|
Figure 14. Steps and actions needed in order to promote HIV
PCT in the K'po District, based on
Suggestions of beneficiary
respondents...............................................................
|
107
|
|
Figure 15: Steps and actions needed to make HIV PCT practice
more acceptable and attractive
for young adults in K'po district, based
on suggestions of beneficiary respondents .........
|
110
|
|
|
|
TABLES
|
|
|
|
|
Table 1: Sub- districts of Kintampo District and their
respective populations.................................
|
5
|
|
Table 2: Sampling characteristics of selected towns and
villages per sub-district...........................
|
31
|
|
Table 3: Distribution of respondents according to premarital sex
history and sex............................
|
41
|
|
Table 4: Trend of general awareness and knowledge on HIV/AIDS,
VCT and HIV PCT...................
|
44
|
|
Table 5: Level of knowledge on HIV
PCT..........................................................................
|
50
|
|
Table 6: Trend of general perception of respondents towards HIV
PCT.......................................
|
53
|
|
Table 7: Level of perceptions towards HIV
PCT..................................................................
|
56
|
|
Table 8: Linear Regression: Regress score of perception =score of
knowledge, CL 95%.........................
|
57
|
|
Table 9. Factors (predictors) influencing Perceived need of HIV
PCT service (p1) among unmarried
young adults in Kintampo
District.........................................................................
|
58
|
|
Table 10. Factors (predictors) influencing willingness to
undergo HIV PCT service (p2) among
unmarried young adults in Kintampo
District..........................................................
|
59
|
|
Table 11: Distribution of respondents according to their
probability of perceiving the need of HIV PCT
and of willingness to undergo HIV
PCT................................................................
|
60
|
|
Table 12. Distribution of respondents by sex and HIV testing
choices.........................................
|
61
|
|
Table 13: Respondents' perception of barriers to HIV PCT
acceptance and implementation...............
|
61
|
|
Table 14: Distribution of respondents by religion and perception
of Islam as a barrier to HIV PCT
Implementation.............................................................................................
|
64
|
|
Table 15: Suggestions from respondents on ways to promote HIV PCT
in Kintampo District..............
|
67
|
|
Table 16 : Suggestions for the HIV PCT practice to be more
effective, acceptable and attractive to
unmarried young people in Kintampo
district.........................................................
|
69
|
|
Table 17: Health facilities where respondents suggest HIV PCT
services to be established................
|
70
|
Chapter One
INTRODUCTION
I.1. BACKGROUND INFORMATION
1.1.1. MARRIAGE AND ITS REPRODUCTIVE HEALTH
IMPLICATION
Legal relationship between a husband and a wife 1, 2,
3, marriage can maintain good sexual reproductive health if it is safe or
rather create ill-sexual reproductive health in couples, if it is
unsafe.4 In fact a marriage may be legal-and
miserable; religious-and diseased. This is partly due to the colossal ignorance
of the public in regard to sex and health implication of marriage, and partly
due to the fact that marriage is mainly controlled by lawyers and priests or
pastors- most of who take no regard for the health status of would-be couples
and their offspring- than by would-be couples themselves and medical
doctors.4 Health aspects related to marriage union require
enlightened interventions from health policy-makers and practitioners to ensure
that marriage is safe for both partners and their offspring, that
it is not leading them to some diseases.4 In fact
marriage union can expose to several diseases such as STI including HIV-AIDS,
genetic diseases (such as sickle cell anemia or thalassemia in children),
rhesus incompatibility, among others 4,5,6,7,8. According to WHO,
«safe sex is a consensual sexual contact with a partner who is not
infected with any sexually transmitted pathogens and involving the use of
appropriate contraceptive measures to prevent pregnancy unless the couple is
intentionally attempting to have a child» 7,9.
In her book in early 1922, Ettie A. Rout4
recognized venereal diseases as the chief obstacle to safe (healthy) marriage,
fact that is still true and even far true nowadays with the incurable HIV-AIDS
which has come to endanger further the humanity. Therefore one of the main
means recommended by WHO to promote sexual reproductive health and safe
marriage in new couples is prior medical control of marriage in paying close
attention and care about the health status of would-be couples as a
prerequisite to pass through before the official celebration of marriage.
3, 4, 5, 6 Indeed most STIs/HIV-AIDS transmission in new couples and
their offspring could be avoided by strict adherence to safe marriage practices
through prenuptial medical counseling and testing of would-be
couples10. That is why, according to WHO, a number of countries
require individuals who are about to enter into marriage to undergo an
examination designed to confirm or infirm the absence of specific diseases,
including those transmitted sexually such as HIV-AIDS and that if evidence of
an infectious disease is found, the marriage cannot be contracted until the
affected would-be couple has undergone treatment and is no longer infective
11.
One of the countries where premarital examination and
counseling is regular is China where law on premarital examination legally
requires every Chinese man and woman planning to get married to undergo a
medical check -up before they tie the knot. 12,13
1.1.2. SCOPE AND OBJECTIVES OF PREMARITAL SCREENING
Pre-marital screening is a comprehensive group of tests
specially designed for those who are planning to get married 14.
Generally, premarital check-up is broadly designed to detect many types of
diseases or health-related problems in would-be couples and when possible to
take preventive or therapeutic intervention and/or provide appropriate
counseling to help them decide. The main specific objectives of premarital
examination commonly recommended and that medical practitioners are called to
carry out in would-be couples, not exhaustively nor exclusively, are as
follows:
1) To assess the copulation ability of would-be couples
5,14,15
2) To assess the fertility or fecundability ability of
would-be couples 5,14,15,16
3) To detect Sexually Transmitted Infections (STIs), including
HIV/AIDS among would-be couples 2,3,5,11,14,15,17,18.
4) To detect the possibility of blood incompatibility
reactions between would-be couples, mainly negative rhesus factor in women when
the would-be husband is rhesus positive 3,6,14,15,19,20,21,22.
5) To detect genetic diseases in would-be couples susceptible
to be hereditarily transmitted to children, e.g. sickle cell anemia,
Thalassemia... 3,5,7,14,15,21,23,24.
6) To detect diseases or factors in would-be couples
susceptible to cause congenital abnormalities or serious pathologies to
children, e.g. Toxoplasmosis,
Rubella... 5,6,7,12,13,14,15,16,18,21,23.
7) To detect chronic diseases in would-be couples that can
destabilize life in family, such as diabetes mellitus, cardiac diseases, mental
deficiency etc 5,6,14,15,21.
8) To establish a pre gestational health status baseline as
part of the engaged woman (would-be mother)'s health profile, determining in
advance her obstetrical prognosis and assess her readiness for child bearing
6,13,14,15,18,20,22,25.
9) To verify whether or not there is an ongoing unknown/hidden
and illegitimate premarital pregnancy in engaged woman 26.
10) To give counseling and health education on safe sexuality
and family planning 27.
11) To exceptionally conduct vaccination for some Preventable
Disease, such as Hepatitis B and Rubella vaccine 15,27. This is
rarely done.
12) Finally, most controversially, premarital examination in
some part of the world , particularly in China, also routinely aims to verify
whether or not a woman's hymen is still intact, even though doctors say that it
is not a reliable guide to virginity 12.
These objectives demonstrate how complex and vast the scope of
premarital examination is and how it can vary from a country to another
depending on the prevailing burden of diseases or health-related problems
generated from marriage and on the national strategies chosen to address them.
For academic purpose and due to time and financial constraints
this study will deal only with premarital check-up on HIV-AIDS. This is because
a VCT service is planned to be implemented in Kintampo District in the near
future28. Thus this preliminary study aims to unveil the knowledge
and perceptions of unmarried young adults on Premarital HIV VCT and to provide
useful information to policy-makers and health authorities for appropriate
methods and strategies to promote premarital HIV counseling and testing in
Kintampo.
1.1.3. STUDY AREA
Kintampo district is located in Brong Ahafo Region in Ghana.
It is one of the 13 Districts in the Brong Ahafo Region. The District has a
surface area of 7162 square kilometers and is bound to the North by the Black
Volta, Wenchi District to the West, and in the East by the Atebubu District and
the Techiman and Nkoranza to the South and South East respectively.
The District has a population of 162008 inhabitants as of end
2004 (This is based on the year 2000 national population census), of whom 27541
(17%) are adolescents and 21060 (13%) are adults aged more than 50 years. The
main indigenous ethnic groups are the Bono`s (most found in Jema Health
sub-district), and the Mos (most found in New Longoro sub-district).
Settlements are mainly concentrated in the Southern part and a long the main
truck road linking the District capital to the Northern Region.28,30
For administrative convenience of health service delivery,
Kintampo District has been demarcated into 8 sub-districts with respective
populations below:
Table 1: Sub- districts of Kintampo District and
respective populations
|
Sub-District
|
Population 2004
|
Observation
|
|
Kintampo*
|
38,882
|
Table 1 shows that the most 2 populous sub-districts are
Kintampo and Dawadawa.
*3 Sub-Districts were the study
took place.
Source: DHD Kintampo 28,30
|
|
Dawadawa
|
34,345
|
|
Jema Health*
|
19,603
|
|
New Longoro*
|
13,771
|
|
Amona
|
15,877
|
|
Kunsu/Apesika
|
19,927
|
|
Anyima
|
11,827
|
|
Busuama
|
7,776
|
|
Total
|
162,008
|
As a whole there are 13 health facilities of which 9 (69%) are
governmental and 4 (31%) are private. 28
Farming is the main occupation in the District.
The 3 sub-districts under study are partly urban and rural.
While Kintampo sub-district is mainly urban, of heterogeneous ethnic groups and
even of multinational residents, New Longoro and Jema are mainly rural area of
homogenous ethnic group, respectively constituted mainly by the Mos and the
Bonos.
The main religion groups in the District and the sub-districts
under study are Christian and Moslem.
Malaria is the leading cause of morbidity and mortality in
Kintampo District. Sexually transmitted infections, including HIV/AIDS are also
among the major public health problems in the District and the 3
sub-districts.28
The STI/HIV-AIDS situation in Kintampo District is favored by
the fact that Kintampo is a major transit centre for all kind of travelers
among them drivers and traders from foreign countries (Burkina Faso, Mali,
Niger....). A part from this fact, it is observed that, due to trading taking
place over 24 hours and girls/young women selling the whole night their
foodstuffs, drivers and other travelers are more likely to solicit those girls
for sex at early age , putting them at high risk of HIV infection. With the
high HIV-AIDS prevalence in adults aged 15-49 years which is the interval age
where most young people get married in the area, also given the trend of
HIV-AIDS prevalence among blood donors in 2004 and of reported AIDS cases in
Kintampo District Hospital and Annor Asare Memorial Clinic (18 cases in 1998,
24 in 1999, 45 in 2000, 52 in 2001, 108 in 2002, 142 in 2003 and 133 in
2004)30, the HIV menace is considerable in the area. Furthermore sex
workers in Kintampo welcome multiple partners, national and foreigner clients.
According to a reliable key informant source quoted in a previous study, they
require different price for unprotected sex which is expensive and protected
sex which is cheaper.32
Because nowadays premarital unprotected sex with multiple
partners seems common among young adults in the area, unmarried young adults
are at high risk of contracting HIV-AIDS before marriage.
So far one of the main activities carried out in 2004 in
Kintampo District was the intensification of Behavior Change Communication in
addressing the HIV/AIDS menace.30, 31
As yet Brong Ahafo Region runs only one VCT centre in
Sunyani43. To extend VCT coverage in the Region, one more VCT center
is planned to be implemented in Kintampo in the future.
I.2. STATEMENT OF PROBLEM
Although recommended by UNAIDS/WHO 10,11,44 , HIV
Premarital counseling and testing (PCT) is not yet implemented in Kintampo,
leading to uncontrolled marriages with risk of spreading HIV infection in new
couples and their offspring. This stands true since in Brong Ahafo Region,
including Kintampo District, the HIV/AIDS prevalence is reported to be of 3.6%
in 2003 and of 4.5% in 2004, the most affected group being females and adults
aged 15-49 years, with the peak ages of 25-39 years.29,38 Therefore
given the high HIV prevalence among young people, the probability for a
unmarried young adult to come across a HIV infected fiancé(e) is
considerable.
Furthermore, estimations and projections of HIV-AIDS
prevalence and mortality suggest that marriages between HIV-AIDS discordant
couples and HIV-AIDS seropositive couples in a society could result, within
decades, in decimation of generations by early deaths of HIV infected parents
and children if adequate HIV preventive and precautionary measures are not
taken appropriately 8,10. This means that policy makers and all
bodies who are involved in marriage celebration and legalization, such as
political and health authorities, lawyers, registrars, traditional chiefs and
religious leaders; have a big responsibility in managing marriage matters and
defining regulations and procedures related to the quality control of marriage.
In fact like birth control is needed in all developed society, quality control
of marriage is also necessary in order to ensure that marriage is safe to both
partners, their offspring and the whole nation. In this purpose WHO/UNAIDS
recommend HIV premarital counseling and testing in order to prevent the spread
of the disease in new couples and their children 10,11,42. That is
why some churches in Ghana and in Kintampo are currently conducting sometimes
HIV premarital testing in would-be couples.
Therefore policy makers should make sure that there are clear
policies that include not only all requirements needed before marriage but also
and especially restricting and limiting rules against unsafe marriages. In
Ghana as yet there is no specific law that regulates premarital examinations.
Yet Ghanaian people still need this service and some churches are currently
allowing would-be couples to undergo HIV premarital examination on either
compulsory or voluntary basis. In this context, HIV premarital counseling and
testing is offered without any detailed regulatory law/policy. Meanwhile many
are those marriages that continue to occur without any HIV premarital
check-ups, putting at HIV risk partners and their offspring. That is why VCT,
including HIV premarital counseling and testing, is recognized nationwide among
current strategies in the national framework to limit the spread of the disease
in Ghana 35. For this purpose a VCT service is planned to be
implemented in Kintampo.
Since the HIV premarital testing will be incorporated in VCT
service in Kintampo, the research questions we ask ourselves are the
following:
· Do unmarried young adults in Kintampo really perceive
and express the need of HIV premarital counseling and testing program in
Kintampo and what are factors associated with the perception of this need?
· How far do young people in Kintampo know about HIV
premarital examinations and what are their perceptions towards premarital
counseling and testing?
· What are the factors that influence the willingness of
young people towards HIV premarital counseling and testing?
· Is HIV premarital examination really a core way to
catch young adults to VCT in Kintampo District as it can be inferred from the
findings in the previous study?32
· What are some barriers against the acceptability and
the institutionalization of HIV premarital examination in VCT services in
Kintampo?
· What key suggestions would unmarried young adults make
towards a very effective, operational, attractive, acceptable and accessible
HIV PCT program in Kintampo?
· What are the points of view of unmarried young adults
on marriage between HIV discordant or HIV seropositive couples and what
possible decisions on marriage are they likely to make in regard to HIV
positive test results?
· What kind of programmes should be carried out in order
to promote HIV premarital counseling and testing in Kintampo district?
Hopefully the study attempts to answer those questions as
clearly as possible.
Poor public knowledge on HIV PCT?
Bad perception towards
HIV PCT?
Low perceived need for HIV premarital screening
services
HIV Premarital examinations not accepted by the
community of Kintampo District
Unwillingness of would-be couples to undergo HIV
PCT
Premarital HIV counselling and testing (PCT) not yet
implemented in Kintampo
Lack of VCT/PCT facilities
Inexistence of Law/Policy conducive to HIV
premarital examinations in the District and Ghana?
Poor utilization of VCT services
in KINTAMPO District
Inadequate control of spread of HIV-AIDS in new
couples/families
Barriers against
HIV PCT
Little solution for those HIV infected
Lack of trained personnel & counselors
Source: The researcher
I.3. CONCEPTUAL FRAMEWORK: PROBLEM ANALYSIS DIAGRAM
(Diagram 1)
Intervention A: As in the previous study majority of people
said not every body can go for VCT unless he/she is about to enter into
marriage in order to decide whether to marry or have children32, we
assume that full implementation of HIV premarital health care in VCT package
will be a potential way to catch young people for VCT, thereby enhancing the
patronization of VCT service in Kintampo by would-be couples.
Intervention A
I.4. RATIONALE OF THE STUDY
VCT service is planned to be implemented in the District in
the future. That is why exploratory studies are being conducted to gather
useful information in this pre-VCT implementation period. This second pre-VCT
implementation study focusing on HIV PCT among unmarried young adults aged
between 15-30 years is conducted as an evidence-based research. In fact being a
follow-up and a complementary research to the previous preliminary study on
«Formative research for the implementation of VCT service in
Kintampo»32, the present study actually looks at the health
need of HIV PCT expressed indirectly by majority of respondents in that survey
which targeted all the community members both married and unmarried ones aged
between 15-49 years. In fact in this previous study 92.1% of respondents said
not every body should go for HIV VCT, 15.7% mentioned that the main reason to
go for VCT is when one wants to get married while 93% said VCT benefit is to
help decide whether to marry or have children. All these findings clearly and
relevantly support the need of HIV premarital health care services and strongly
demonstrate how VCT implementation in Kintampo District should go together with
the implementation of HIV PCT as it is recommended by WHO/UNAIDS
10,11,42.
Now since most people who get married in Kintampo are in the
age range between 15-40 years (Source: marriage registration in Kintampo
Magistrate court and data from some churches) while the most affected by
HIV/AIDS in Ghana and in the District are in the age group of 15-49
years29, also because it is reported worldwide that more than half
of people living with HIV/AIDS (PLWHA) were infected before they were 25 years
of age with young people aged 15-24 accounting for more than 50 percent of all
HIV infections worldwide44 and in Ghana 29, implementing
HIV premarital examinations in the area will help to detect those young adults
unknown carriers of the HIV/AIDS; so that appropriate measures can be taken
early to reduce the HIV spread and further new infections in new
couples/families and their offspring.
Given the fact that authors and WHO recognize that operational
researches on human sexuality perception and counseling are strongly needed in
order to improve reproductive sexual health7,9,11,54,55,56, and
considering that a nation's collective attitude and perception towards human
sexuality is culturally determined and can profoundly influence several aspects
of reproductive health and related policy-making 39, including HIV
premarital examinations, we hope that the study results on knowledge and
perceptions towards HIV premarital medical examination will constitute a data
base on which policy makers can refer to in examining the matter on the
horizon.
Knowing fewer researches have been undertaken on the ground on
HIV PCT, we think the study will generate practical suggestions from primary
beneficiaries, that District Health Authorities in Kintampo could take into
account in order to implement a highly locally owned and compatible HIV PCT
program which meets the real expectations of the beneficiary population and
consequently culminates in success, like it has been proved in many other parts
of the world. 10,57
I.5. GOAL AND OBJECTIVES OF THE STUDY
Broad objective:
The community youth-based research aim is to generate useful
information on current level of knowledge and perceptions of unmarried young
adults towards HIV premarital counseling and testing (PCT) in order to predict
their acceptance and behaviours towards utilization of such service and to
deduce appropriate program/policy for intervention in the relevant area.
Specific objectives:
Ø Primary:
1. To identify factors (predictors) that influence the
willingness of young unmarried adults to undergo HIV premarital counseling and
testing.
Ø Secondary:
2. To determine factors (predictors) influencing perception of
health need towards HIV premarital medical counseling and testing among
unmarried young adults.
3. To determine whether unmarried young adults will prefer to
undergo HIV VCT for marital reason or not.
4. To identify any barriers to the acceptance and the
implementation of HIV PCT in Kintampo and collect evident suggestions from
respondents for an effective HIV PCT service.
5. To determine the point of view of unmarried young adults on
marriage between HIV discordant or HIV seropositive couples and identify
possible decisions on marriage that they are likely to make in regard to HIV
positive test results after PCT.
Chapter Two
LITTERATURE REVIEW
2.0. DEFINITION OF CONCEPTS
- Adolescent: a young person who is developing from a child
into an adult 1,33
Early adolescence: between 10-13 years Mid adolescence:
14-15 years.
Late adolescence: between 16-19 years
- Youth: the time of life when a person is young, especially
before a child becomes an adult1
- Adult: a fully grown person who is legally responsible for
their actions1
Note that in this study we are dealing with unmarried young
adults aged between 15 (mid adolescents) and 30 years.
- Knowledge: the state of knowing about a particular fact or
situation1. The study deals with the state of knowing about HIV
PCT.
- Perception: the way you notice things, the ability to
understand the true nature of something1 . The study deals with the
way respondents notice HIV PCT and understand its true nature.
2.1. PREMARITAL EXAMINATION IN GHANA AND IN
KINTAMPO
«Laws on Premarital examination» is classified by
WHO among core specific legislations for the prevention of Sexually Transmitted
Infections (STIs) and other diseases in new couples in a country 11.
Yet so far in Ghana there is no specific law about premarital counseling and
testing that describes its objectives, practical procedures and formal legal
processes. However current existing policies (National Population Policy 1994,
Adolescent reproductive Health Policy 2000 and National Reproductive Health
Service Policy and Standards 2003, National HIV/AIDS and STI Policy) clearly
mention the importance of «Information and counseling'' for young people,
including premarital counseling and testing 9,33,34,61. For instance
the section 4.3.7 of the objectives of the above revised National Population
Policy strongly shows the government's responsibilities towards young people,
and I quote «To educate the youth on population matters which directly
affect them such as sexual relationships, fertility regulation, adolescent
health, marriage and childbearing, in order to guide them towards responsible
parenthood and small family sizes»34. The right for young
people to have access to all information and counseling regarding reproductive
health is also reemphasized in the adolescent reproductive health policy in
section 3.2 which states: « ... Available evidence suggest that
adolescents behave responsibly when they are well informed, especially on
issues such as career development, relationships and reproductive health.
Therefore at this stage individuals need adequate and reliable information to
enable them make the right decisions and choices...»33. In
addition in the national strategic framework for HIV-AIDS, access to HIV VCT
(including HIV premarital exam) is considered nation wide as a crucial service
in the national response to combat HIV/AIDS 35,36. All these
literatures, just to mention a few, demonstrate that Ghanaian young people have
the right to access HIV premarital counseling and testing services in order to
make informed and right decisions and choices towards marriage.
In Ghana, like in most countries in sub-Saharan Africa,
pre-marital HIV VCT is being widely promoted, particularly by churches and
religious groups. Meanwhile in practice due to the expressed need of such
service by young adults, HIV premarital examination is being carried out, not
commonly, in certain towns, including Kintampo town. In fact report from the
laboratory of Kintampo District Hospital (KDH) indicates that since January
2004 till July 2005, 14 would-be couples aged between 24 - 34 years old were
received for HIV PCT, of whom 12 (86%) were sent by their churches while 2
(14%) came voluntarily. None of them tested HIV positive. These data showing a
timid starting of the service in an embryonic stage constitute an undeniable
and strong opportunity which will enable the smooth official implementation of
HIV PCT in the District.
In general premarital examination is done on voluntary demand
and consent of some would-be couples or in most cases by some churches that
impose it instead. Furthermore, the examination has a selective meaning since
in most cases it targets only HIV-AIDS testing and forgets about all other
required premarital tests, thus resulting in an incomplete premarital check-up.
2.2. HIV-AIDS SITUATION IN WEST AFRICA AND GHANA
Since HIV-AIDS is nowadays the common most well known scourge
that frightens humanity and that justify for many people the necessity of
premarital check-up which is one of the preventive measures to reduce the
spread of the infection, most young adults are likely to opt for HIV premarital
check-up only because of fear of being married to an HIV seropositive
fiancé(e). Therefore it is fair to elucidate in this paper the
particular magnitude of this scourge in the region.
4.1.2. 2.2.1. In West Africa
Although varying in scale and intensity, the epidemic in
West Africa appears to have stabilized in most countries.
Median HIV prevalence measured among women in 112 antenatal clinics in the sub
region remained at an average 3% to 4% between 1997 and 2002.37
Overall, HIV prevalence is lowest in the Sahel countries and highest in
Burkina Faso, Côte d'Ivoire and
Nigeria--the latter having the third-largest number of people
living with HIV in the world (after South Africa and India). In the two
countries flanking it--Ghana and Benin--HIV
prevalence is in the 2% to 4% range with little change noted over time
37.
A variety of factors (economic changes and cooperation,
transportation links, periods of instability and war...) experienced across the
West African sub region have all contributed to increased mobility and,
subsequently, the cross-border spread of HIV in Ghana. 29
4.1.3. 2.2.2. In Ghana
In Ghana HIV prevalence was in the 2% to 4% range (median
prevalence of 3.6%) in 2003 29 versus 0.4% to 7.4% range (median
prevalence of 3.1%) in 2004 38 with little change noted over time
37. By the end of 2003, close to 4 percent (3.6%) of the country's
adult population was estimated to be HIV infected. This corresponds to about
395,000 Ghanaians aged 15-49 years, most of who do not even know they carry the
virus. HIV prevalence differs from Region to Region, the least being in the
Upper West (1.8% in 2003 versus 1.7% in 2004) and the highest in the Eastern
Region (6.6% in 2003 versus 6.5% in 2004).
Being among regions with high HIV prevalence, Brong Ahafo
Region including Kintampo District recorded a prevalence of 3.6% in 2003
29 versus 4.5% in 2004 38 , suggesting an increasing
trend of the epidemic in the region.
In Ghana, as in the rest of Africa, two main transmission
mechanisms account for most new HIV infections: Heterosexual contact (80%) and
mother-to-child transmission `MTCT`(15%). Other mode of contamination through
contaminated blood (transfusions, sharing of needles or blades...) account for
5% 29.
Although the probability of transmitting HIV during
intercourse can be quite low 39, a number of factors increase the
risk of infection dramatically. One is the presence in either partner during
unprotected sex of a sexually transmitted infection (STI), such as syphilis or
gonorrhea. These diseases cause genital ulcers and sores that facilitate the
penetration of the virus during the coitus. The 2003 sentinel surveillance
results showed that a significant number of Ghanaian young adults suffer from
STIs, and many have multiple sexual partners but don't use condoms to protect
themselves 29. It is estimated that most new HIV infections in Ghana
are due to heterosexual contact 29. Programmes designed to reduce
the spread of HIV should focus on reducing transmission through unsafe sexual
contact. HIV Premarital screening meets this strategy.
HIV Premarital examinations will also impact on HIV
Mother-To-Child Transmission.
HIV has spread more slowly in Ghana than in many other African
countries. For example, in several southern African countries, HIV prevalence
among people 15-49 years old is now estimated at more than 15%. No one is quite
sure why the epidemic has spread more slowly in Ghana and in some other West
African countries. What should be kept in mind is that many eastern and
southern African countries had prevalence rates in the late 1980s similar to
those currently found in Ghana and that the situation worsened very rapidly
29. All this demonstrates how an unchecked HIV-AIDS epidemic
including uncontrolled marriages could still result in much higher increased
HIV prevalence levels in Ghana, hence the necessity of preventive measures
among which is HIV premarital examination in order to reduce particularly HIV
prevalence in new couples and their future offspring. Ghana should not wait
until it reaches much higher HIV prevalence to now formalize HIV premarital
counseling and testing like it was in Ethiopia 40.
The threat of HIV/AIDS and the concern for Africa's future
generation were earlier reflected in the 1992 Organization of African Union
(OAU) Declaration on AIDS in Africa. It is pertinent to extensively quote a
part of this Declaration as quoted by UNDP
41., thus:
«... The hope of Africa is its younger
generation who still has a chance to escape infection, we must seize this
opportunity and ensure that today's girls and boys, who will be the mothers and
fathers of tomorrow's children, are safe from HIV...»
This declaration strongly implies the necessity of preventive
interventions to protect younger African people from the threatening HIV-AIDS
infection. In fact more than 7,000 young people are newly infected with HIV
each day throughout the world42. In Africa alone, an estimated 1.7
million young people are infected annually.43,44
Some countries including Ghana are now acknowledging the
importance of targeting youth in their HIV prevention and care strategies and
include VCT and premarital HIV testing for youth in their agenda. Preventing
HIV among young people through VCT and HIV PCT is particularly urgent in
sub-Saharan Africa, where in many countries young people comprise more than 30
percent of the population and general HIV prevalence rates is often
high.44 National guidelines for the Republic of Ghana state that it
shall «seek to ensure the expansion of the access of young people to
youth-friendly facilities and services including HIV and STI (sexually
transmitted infection) prevention, management and testing, counseling and the
provision of care and support services.»35
In Ghana there is near universal awareness of HIV-AIDS, 98 %
among females and 99 % among males in the whole country, the level of awareness
of HIV-AIDS in Brong Ahafo Region (Kintampo District included) being 99.5% and
100% respectively in women and men. However, risk perception is still low:
about one-third of the population believes they are not personally vulnerable
to HIV infection. 29,53 This high HIV awareness rate is a strong
opportunity upon which prevention programs could be based.
2.3. HIV PREMARITAL COUNSELING AND TESTING (PCT)
4.1.4. 2.3.1. DEFINITION
HIV premarital counseling and testing is a specific form of
HIV VCT by which an individual who is about to enter into marriage undergoes
counseling enabling him/her to make an informed choice about being tested for
HIV in order to be able to make informed, right and responsible decision about
marriage and production of offspring. However, some countries classify HIV PCT
as a mandatory HIV testing rather than voluntary.10,35,42,45
4.1.5. 2.3.2. JUSTIFICATION OF PREMARITAL EXAMINATION
Why is pre-marital examination
important?
Many people are not aware of their state of
health. An individual might look healthy but he may be a silent carrier to
potentially contagious infections or serious hereditary disorders. A routine
medical test will reveal such conditions so that necessary precautions or
course of treatment could be initiated to avoid affecting the partner or
passing on the disease to the next generation. Therefore premarital screening
is important since it allows would-be couples to assess their own general
health status, maintain good physical health for a 'happily ever after'
marriage and strengthens the marriage relationship.14,15,27,46
With advancements in medicine engineering opening up new
possibilities of medical screening - and with the fear of the spread of
diseases like STIs including HIV-AIDS - there is considerable pressure to
require prospective spouses to undergo pre-marital medical exams. Thus some
countries, like France, China, Syria, Tunisia, Egypt, Morocco, Saudi Arabia,
the United Arab Emirates (UAE), among others, have encouraged their citizens to
go for such pre-medical exams. Some have even made doing so a legal mandatory
requirement for marriage that allows not only informed, right and responsible
decision about marriage but also the control of targeted diseases and health
related problems in new couples.10,14,15
Furthermore, the marriage contract is a serious commitment
that is supposed to be permanent and stable. If it surfaces after marriage that
one of the spouses has a serious disease, this could lead to a premature
termination of the marriage (divorce) if the other party refuses to stay with
the person on account of the illness.14,15
Finally research has shown that there is higher level of
marital satisfaction and stability among couples who attended a satisfactory
premarital counseling and testing than those who did not.46
4.1.6. 2.3.3. HIV PCT PACKAGE 10
Like in all VCT service, counseling plays a significant role
in HIV premarital examinations. Therefore classic HIV PCT service package
ensures that:
a. Knowledge of status is
voluntary;
b. Pre-test counseling is offered
either through one or more sessions with a doctor or trained counselor, after
which the engaged individuals may choose to test on the same or different
day;
c. Informed consent is obtained from
the engaged person by a service provider; couple counseling for VCT is valuable
intervention when truly voluntary and when there is adequate informed consent
by both parties10.
d. Interrogation and physical examination of
client is performed by the physician in a serene atmosphere;
e. HIV test (and other required
laboratory tests) is ( are) performed using approved tests and testing
protocols;
f. Disclosure of test results and Post test
counseling: one or more sessions held for informing client of
his/her test results may take place on the same or different day after adequate
post test counseling. The physician/counselor must disclose the results to the
concerned person.6,47 The responsibility of the physician/counselor
is to warn would-be couples on eventual consequences of a positive HIV test
result he discovered and on possible preventive measures to limit the spread of
the infection. He may not disclose the result to the partner, unless the owner
of the result gives prior permission. In any case the physician/counselor
should not refuse to disclose the results and to deliver the prenuptial medical
certificate to the client.6,47
In certain part of the world, doctor can even recommend
against marriage and let the couple decide on the
recommendation.10,13
The essential thing is that if a fiancé(e) is found HIV
seropositive, he will be informed by a medical counselor on the dangers facing
the couple and the expected offspring so that (s)he makes responsible and
informed decision about marriage. The physician/counselor shall also inform
both parties to the intended marriage of the nature of the disease, the
possibilities of transmitting such infection to his or her marital partner or
to their children and the possible available preventive actions (e.g. protected
sex by condom, mutual faithfulness, PMTCT...) to be applied for life if they
still wish to marry. The couple, or each fiancé at least, then decides
freely and knowingly whether they go ahead with the marriage, regardless of the
results or break the marriage project. 48,49
g. Deliverance of prenuptial medical certificate (marriage
license) to the client after post test counseling, document that is required
for the publication and the celebration of marriage.3,5
HIV PCT without pre- and post-test counseling should not be
recommended.
2.4. PROCUREMENT OF MATERIALS FOR VCT
The important step in procurement of VCT materials is deciding
how much of each commodity to buy. Commodities needed for youth friendly VCT
services may include-- HIV test kits, -Automated analyzers, such as
enzyme-linked immunoassay (ELISA) readers, -Centrifuges, -Refrigerators,
TV/video equipment and health education videos, - Information leaflets, -
Contraceptives, - Drugs for palliative and supportive care, such as pain
management, - Antiretroviral (ARV) drugs for treatment and prevention of
mother-to-child transmission, - Drugs to prevent and/or treat Opportunists
Infections (OI), such as tuberculosis (TB) prophylaxis, - etc All these
should be provided in a VCT /PCT site10.
2.5. FACTORS INFLUENCING WILLINGNESS TO UNDERGO HIV
PCT
Studies have shown that willingness to have premarital HIV
counselling and testing is positively associated with increased age, urban
residence, and wish to keep one's own HIV testing result confidential. However,
knowledge of a person with HIV/AIDS, HIV testing location, and other sexually
transmitted infections/diseases, as well as belief that abstinence protects
against HIV are inversely related to desire to take an HIV
test.45
2.6. REASONS FOR UNDERGOING HIV VCT
The main reasons clients seek VCT include unprotected
sexual intercourse, wanting to get intimate, premarital,
believing that they are already infected, STI
infections, pre-university or employment.10
2.7. BARRIERS TO HIV VCT/PCT
Some barriers to HIV VCT/PCT have been recognized
worldwide10. These are:- Availability and acceptability of VCT
services, including legal issues ,- Waiting time ,- Costs and pressure by
health staff to notify partners, - Worries about confidentiality and fear that
results would be shared with parent(s) or partner(s) without their consent , -
Lack of perceived risk and lack of perceived benefits in knowing HIV status, -
Lack of information about VCT services/shortage of VCT centres. -Fear of being
labelled and stigmatized by their families, friends and communities
- Perceptions of the consequences of living with HIV, -
Inadequate responses from health care providers, including counsellors, to
effectively meet the HIV prevention, care and support needs of youth - etc
2.8. MARRIAGE BETWEEN HIV DISCORDANT OR HIV
SEROPOSITIVE
COUPLES
The third International Consultation on HIV/AIDS and Human
Rights recognized rights of PLWA, including marriage.70,71,72
However because of stigmatisation and discrimination, people tend to
exclude PLWA to their right to marry. Some groups (including evangelical church
groups) demand to cite test results as grounds to deny a marriage ceremony
(where results are discordant or positive). Test result certification is not
provided by most VCT sites because of the potential misuse or negative
consequences, including stigma, discrimination and false hopes of
«safety»10. Also, despite the proved `Assisted
Reproduction in HIV infected individuals` many people are reluctant to marriage
between discordant and HIV seropositive couples.73
Chapter Three
METHODOLOGY
3.1. STUDY DESIGN AND STUDY POPULATION
The study was a descriptive cross-sectional community based
study using both qualitative and quantitative tools. The study population was
all unmarried young adults of 15-30 years old living in the district. This
target group of unmarried young adults has been chosen because they are the premarital age population and
primary beneficiary and stakeholder of HIV PCT.
3.2. VARIABLES UNDER STUDY
The study variables were as follows (see Diagram 2 on page A
and annex 4 on page N):
A-Socio-demographic background variables: Age, sex, place of
residence, level of education, occupation, religion and ethnic group.
B- Premarital sex history, C-Level of Knowledge on STI,
HIV/AIDS, VCT and PCT
D-Perception towards HIV PCT, E-Perceived need of HIV PCT
services
F-Readiness to know and accept HIV PCT results
G-Suggestions that HIV PCT should be provided at affordable or
free cost
H-Perceived need of confidentiality and privacy regarding HIV
PCT exam and results
I-Willingness to undergo HIV Premarital Counseling Testing.
J- Suggestions of clients towards a very effective and
acceptable HIV PCT program
e.g Respondents who say HIV PCT should be compulsory or
optional
K-Point of view on marriage between HIV discordant couples and
HIV seropositive couples and possible decisions on marriage that unmarried
young adults are likely to make in regard to HIV positive test results.
Assumptions:
We assumed that there was some relationships between these
variables as it is described in Diagram 2. In fact we thought that the
likelihood for a young unmarried adult to perceive the need of HIV PCT services
was function of background personal specifications (age, sex, educational
level, religion, residence area, tribe), the premarital sex history, the
general knowledge on STI, HIV/AIDS, VCT/PCT and the general perceptions towards
HIV PCT.
We also assumed that the willingness of a respondent to
undergo HIV PCT was function of all the variables above plus the perceived need
of HIV PCT services, the readiness to know and accept HIV test results, the
suggestion that the provision of HIV PCT services should be at affordable or
free cost and the perceived need of confidentiality and privacy regarding HIV
PCT results. We also thought that application of key suggestions given by
respondents may stimulate their willingness and their attendance towards HIV
PCT, thus culminating to a very attractive, effective and successful HIV PCT
program.
From these two first assumptions we derived two logit models
which we attempted to verify in our data analysis.
Finally we assumed that once an unmarried young adult has the
willingness to undergo HIV PCT, (s)he might then take the HIV test and attend
counseling sessions. Counseling would then help him/her to know and accept
his/her HIV test results. Counseling sessions might also help him/her take
informed decision about marriage and develop a clear point of view on marriages
between HIV infected people.
Diagram 2: RELATIONSHIP BETWEEN VARIABLES: ASSUMPTIONS
OF LOGIT MODELS
-Knowing of a unmarried young adult HIV/AIDS sick
person
-Premarital sexual abstinence protects against HIV/AIDS while
premarital sex is a risk factor to HIV
-Children could be HIV infected from marriage union of their
parents
- Not all sexual unions and marriages are safe and good for
health of partners and their offspring.
- Good health status is a core criteria in the choice of a
fiancé(e)
- Recognition of PCT as the adequate and right measure to
assess the health status of one's fiancé(e)
-Have heard of HIV VCT
-Have heard of HIV PCT
-Knowing that HIV PCT is a core mean to limit the spread of
HIV/AIDS in new couples
-Knowing of any person/couple who underwent HIV PCT
-A healthy fiancé(e) could be unknown carrier of
HIV
-Knowing who the beneficiaries of HIV PCT are
-Knowing the major advantage of HIV PCT
C. Knowledge on HIV/PCT
F.
Readiness to know and accept HIV PCT results
E. PERCEIVED NEED OF HIV PCT
I.
WILLINGNESS TO UNDERGO HIV PCT
H.
Perceived need of confidentiality and privacy regarding HIV
PCT results
-Age -Sex -Educational Level
-Religion -Tribe
-Residence (Urban/Rural) etc
-Having had sex
-Age at first sex (sexarche)
-N0 of sexual partners etc
-Perceived risk of one self and one's fiancé (e) to
HIV/AIDS
-Perceived severity of HIV/AIDS
-Perceived threat of contracting HIV/AIDS in case one get
married to a infected HIV person when HIV PCT is not done.
-Perceived benefit of HIV PCT
-Perceived self control over HIV PCT
-Perception that most relatives (family members/peers) approve
HIV PCT
-Perception that HIV PCT should be institutionalized in the
country
-Perception whether HIV PCT should be compulsory or
optional.
- Perceived barriers to HIV PCT
- Preference to undergo HIV VCT for marital reasons or
not.
A. Background Variables
B. Premarital sex History
D. Perception towards HIV PCT
Logit Models:
E=á1+ßi(Ai)+
ßii((Bii)+ ßiii(Ciii))+
ßiv(Div)
I= á2+ß'i(Ai)+
ß'ii((Bii)+
ß'iii(Ciii))+
ß'iv(Div)+ ß'v(E)
+ ß'vi(F) +
ß'vii(G)+ ß'viii(H)
J. Key Suggestions of clients towards a very effective and
acceptable HIV PCT program/Policy
HIV PCT undergone
K. Decision towards marriage given the HIV PCT results and
point of view on marriage of HIV (+) fiancés
HIV test result of oneself and one's fiancé (e) is
known
C o u n s e
l I n g
G.HIV PCT at affordable or free cost
Source: The researcher
3.3. DATA COLLECTION TECHNIQUES AND TOOLS
4.1.7. 3.3.1. Data collection techniques
The study was performed into two phases and employed five main
data collection techniques, namely the Review of available records and
literature (Desk Research), the Focus group discussion (FGD), the In-depth
Interviews (IDI) and the survey.
The first phase of the study -through desk research, in depth
interviews and focus group discussion-was fully exploratory and qualitative in
order to generate primary information while the second-one was the survey which
generated quantitative data.
4.1.8. 3.3.2. Data Collection Tools
The tools used in the study were as follows: Problem analysis
diagram (Diagram 1), Assumption of relationship between variables (Diagram 2),
survey structured questionnaire (Annex 1), In-depth Interview guide (Annex 2a
& 2b), FGD guide (Annex 3), existing reports, Table of variables (Annex 4),
list of selected compounds, notebook, cameras, tape recorder, papers , pens and
computers.
The structured questionnaire was mostly made of closed-ended
questions offering either a choice among "yes", "no", or "I don't know" or a
choice among several options.
3.4. SAMPLING
4.1.9. 3.4.1. SAMPLE SIZE CALCULATION
We calculated the sample size using EPI_INFO version 3.3 based
on the following:
1. Population size of unmarried young adults in the age group
15-30 years old in the 3 sub-districts under study: 16.944 (data source: KDSS,
see Table 2 ).
2. Expected frequency on level of perceived need towards HIV
premarital examination and of willingness to undergo HIV PCT: 16%. This
expected frequency was drawn from the previous study on VCT establishment where
findings showed that 15.7% of respondents mentioned when one wants to get
married as the main raison for going for VCT 32.
3. Worst acceptable frequency on level of perceived need
towards HIV premarital examination and of willingness to undergo HIV PCT: 10%
(meaning an acceptable margin error of 6%)
4. Confidence level: 95%
5. Computed sample size: 142
Thus a sample size of 142 individuals was targeted. This was
rounded up to 150 unmarried young adult respondents. However
in prevision of eventual drop out from interviews or questionnaire
disqualification due to incompleteness or inconsistency, an extra 20 more
interviews was conducted so that the sample size is fully met.
4.1.10. 3.4.2. SAMPLING METHOD
Non-probability sampling was used. In order to obtain complete
and balanced insight in how knowledge and perceptions towards HIV premarital
examination were distributed in different cultures in males and females, in
rural and urban areas, in educated and illiterate ones, in different religious
and ethnic groups and in different professional categories, all these different
background groups were included in the sample as much as possible in order to
capture a holistic picture.
The main steps in sampling process included the following:
· Purposeful choice of 3 study sub-districts (Kintampo,
Jema Health and New Longoro) and proportionate attribution of quota sample
based on population density of each sub-district.
· Purposeful sampling of key-informants and participants
in IDIs and FGDs.
· Purposive selection of Twelve settlements (towns and
villages) from the 3 sub-districts ( 4 in Kintampo, 4 in Jema Health and 4
in New Longoro) based on population density, geographic location (urban /rural)
and mix of high HIV/AIDS risk (proximity to the highway and prevalence of
stop-over) so that the sample is as much heterogeneous as possible.
· Deduction of proportionate quota sample per
settlement.
· Random selection of 210 compounds out of 3973 (from the
whole total of 19167 in the 3 sub-districts) compounds identified with eligible
respondents from selected settlements, using the computer based data of
Kintampo Demographic Surveillance Survey (KDSS) used in KHRC with STATA command
«draw random sample». Note that the computer ballot system was done
by the KHRC agent, head of field workers in charge of KDSS.
· Selection of respondents: One respondent was selected
per targeted compound.
Any unmarried young adult between 15-30 years old found in any
selected compound was interviewed. In case two or more eligible respondents
were found in the same compound, priority was made on one volunteer who
consented to participate in the interview; otherwise a drawing lot was carried
out to choose only one of respondents who all consented to participate. In case
no respondent was found in a compound, the next selected compounds were
targeted until the full quota sample required was covered.
In order to purposefully equilibrate the sex distribution of
respondents or get a less skewed sex distribution, systematic random selection
of compounds was made from two sex (female and male) sub-sampling computer
based frames drawn from the KDSS which contains data on all the characteristic
of people per registered compound. Thus to each selected compound was assigned
automatically the sex of the respondent to be interviewed.
Table 2 describes the selected settlements and their assigned
quota samples. The district map below also describes the geographical situation
of the selected settlements.
|
Table 2: Sampling characteristics of selected towns and
villages per sub-district
|
|
Selected Towns and villages per
Sub-District
|
Town & Village Code
|
Pop. Density
|
Category of settlement
|
HIV Risk Level
|
Number
of RA
|
Population of 15 - 30 years
|
Sample Size*
|
Number
of
Cpd**
|
|
I. KINTAMPO SUB DISTRICT
|
|
1.Kintampo
Town
|
X
|
High
|
Urban
|
High
|
5
|
11066
|
70 (80)
|
100
|
|
2. Agyegye-
makunu
|
AG
|
Low
|
Rural
|
Low
|
1
|
178
|
1 (1)
|
2
|
|
3. Babator City
|
BB
|
High
|
Urban
|
High
|
2
|
1386
|
9 (10)
|
12
|
|
4. Punpuatifi
|
PF
|
Low
|
Rural
|
Low
|
-
|
109
|
1 (1)
|
2
|
|
TOTAL
|
8
|
12739
|
81 (92)
|
116
|
|
II. JEMA SUB DISTRICT
|
|
5. Jema Town
|
JM
|
High
|
Urban
|
High
|
2
|
1542
|
19 (22)
|
26
|
|
6. Nante
|
NN
|
High
|
Rural
|
High
|
1
|
791
|
11 (12)
|
14
|
|
7. Kokuma
|
KK
|
Low
|
Rural
|
Low
|
1
|
312
|
4 (5)
|
6
|
|
8. Ampoma
|
NP
|
Low
|
Rural
|
Low
|
1
|
517
|
7 (8)
|
9
|
|
TOTAL
|
5
|
3162
|
41 (46)
|
53
|
|
III. NEW LONGORO SUB DISTRICT
|
|
9. New Longoro
Town
|
LL
|
High
|
Urban
|
High
|
1
|
402
|
10 (12)
|
14
|
|
10. Asantekwa
|
AS
|
Low
|
Rural
|
Low
|
1
|
283
|
8 (9)
|
11
|
|
11. Busuama
|
BS
|
Low
|
Rural
|
Low
|
1
|
315
|
9 (10)
|
12
|
|
12. Sogliboi
|
SL
|
Low
|
Rural
|
Low
|
-
|
43
|
1 (1)
|
2
|
|
TOTAL
|
3
|
1043
|
28 (32)
|
39
|
|
|
|
|
|
|
OVERALL TOTAL
|
16
|
16944
|
150
(170)
|
210
|
|
Source : Kintampo Health Research Centre (KHRC) demographic
surveillance survey sampling frame and our Field survey, Kintampo (June
2005).
|
|
RA= Research assistants (Interviewers)
|
|
* The number in bracket corresponds to the total sample size
including extra sample units needed for replacement of eventual opt out or
questionnaire disqualification so that an overall sample units of 150 with
consistent and complete questionnaires is met.
|
|
** Number of Compounds selected per town/village in each
sub-District.
|
Figure 0: Map of Kintampo District showing Centroids of study
(villages/Towns) and roads network (Source: KHRC,
June 2005)
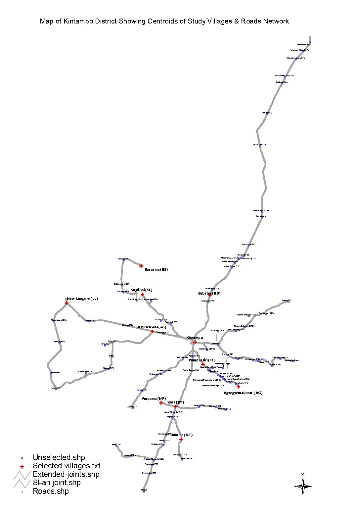
3.5. DATA COLLECTION
- In-depth interviews with 17 key informants and 8 Focus group
discussions of 6 members each (2 FGD for unmarried young adults and 6 for
parents) were conducted at appointed and agreed times between 13th
June and 15th July 2005 in Kintampo Town and Ampoma village.
- To minimize information bias, 20 research assistants who
speak both English and Twi were selected and trained on 14th June
(for the 3 assistants involved in qualitative study) and on 25th
June 2005 (for the 17 field workers involved in the survey) in order to enable
them do their work appropriately. These were made of 1 field supervisor, 16
interviewers to administer the structured questionnaire, 1 language translator
for translating the questionnaire, the IDI and FGD-guides and qualitative data
from English into «Twi» (a local dialect), 1 moderator for moderation
of FGDs, and 1 note-taker for note-taking and reporting. All the research
assistants were from KHRC staffs who were assigned to help us in part-term
while still doing their KHRC routine work.
- The pre final questionnaire was pre-tested on
25th June 2005 in Kintampo Sub-District among 20 respondents from
compounds not selected in the study. Six questions were reframed and adjusted
based on the results from feed-back of the pretesting session.
- The survey involved 16 experienced and well trained KHRC
field research assistants. It included at large 170 respondents (150 for study
purpose and 20 for eventual back-up in case of questionnaire disqualification
for incompleteness or inconsistency) and was carried out during 7-10 days from
28th June to 7th July 2005, with average rates of 17-24
questionnaires per day (that is 1-2 questionnaires per day per interviewer) and
30-40 minutes per questionnaire.
- Illustrative photographs on the course of the study were
taken among participants.
3.6. DATA PROCESSING AND ANALYSIS
4.1.11. 3.6.1.
QUALITATIVE DATA
Qualitative data from IDI and FGD were recorded and translated
into English and summarized in Matrix by the researcher. The transcribed
information was reviewed and the main issues summarized.
4.1.12. 3.6.2.
QUANTITATIVE DATA
3.6.2.1. Data quality control
For better quality of data we carefully checked the
completeness and the internal consistency of each questionnaire. Thus out of
the 170 administered questionnaires, twenty found incomplete and with
inconsistent data were simply canceled and replaced by complete ones.
3.6.2.2. Data presentation and statistical
analysis
For easier analysis, pre-coded data from survey questionnaires
were entered into FOXPRO view and then converted into EPIINFO 3.3, STATA and
EXCEL formats that we used in analysis.
Analyzed data was then presented as summarized results in
tables and graphs.
For analytical interpretation, we carried out calculation of
frequencies and relative frequencies. Statistical tests included X2
(chi square), P-values and Odd ratio with 95% confidence intervals. The
level of statistical significance was set at p<0.05.
Two Logit models were used to determine the factors that
affect the probability for a respondent to perceive the need of HIV PCT service
and the probability of willingness to perform premarital HIV counseling and
testing (from Diagram 2). As the data were mostly categorical and the response
binary (Yes/No answers), Logit models were found appropriate to be
used.58
3.6.2.3. Score allocation for level of knowledge and
perception towards HIV PCT
In order to evaluate level of knowledge and level of
perception towards HIV PCT with a more measurable scale, we assigned scores to
answers to specific defined questions. Thus all respondents were given each a
total score of level of knowledge and of level of perception towards HIV PCT
(see ANNEX 4 for details on score attribution per specified question). Then the
following tri-polar marking scale was drawn in order to assess the level of
knowledge and of perception of respondents towards HIV PCT:
|
Level of Knowledge on HIV PCT
|
Level of perception towards HIV PCT
|
|
Range score: 0-22 marks
|
Range score: 0-23 marks
|
|
Acceptable minimum/mean score: 11
|
Acceptable minimum/mean score: 11,5
|
|
Marking scale:
1.Poor knowledge: score < 11
2. Good knowledge: score = 11
a. Average good knowledge: score 11-16,5
b. Adequate good knowledge: score > 16,5
|
Marking scale:
1.Negative/lower/bad perception: score < 11,5
2. Positive/higher perception: score = 11,5
a. Average positive perception: score 11,5-17,5
b. Adequate positive perception: score > 17,5
|
3.7. SOME ETHICAL CONSIDERATIONS
The study topic was conceptualized with the District Director
of Ghana health service of Kintampo District. Nevertheless the study subject
was thereafter actually put in mind of the District Assembly, all local
Traditional, Religious and other opinion leaders in order to co-opt their ideas
to ensure their consent, ownership and permission on the study.
All key informants and interviewees received explanations that
the study would be beneficial to the District in the sense that findings would
really help Kintampo District Health Authorities to implement a very effective
VCT/HIV PCT service in the near future.
Community entry was done through DHMT members and KHRC field
workers.
Autonomy of all key informants, interviewees and even
interviewers was respected. Respect of confidentiality was assured regarding
all information given by participants. The questionnaire was anonymous for
confidentiality purposes.
The research team members were kindly soliciting free
self-acceptance (voluntary participation) and informed consent of all
participants involved after explaining them the relevance of the study and the
role expected from them.
Freedom of refusing or abstaining from answering some
questions or of even withdrawing from an ongoing interview or discussion was
guaranteed for people who consented to participate. Consent from participants
was also sought regarding recording their voices and or taking their pictures
and using them in the study report. Thus pictures in this work received
prior verbal permission of concerned participants to be published as live
testimonies.
For some sensitive and intimate questions, like having ever
had sex, interviewers used polite introductive word like
«Sebi» to kindly beg respondents to freely consent not only
to answer but to just give right answers although the question directly touched
their intimacy.
3.8. LIMITATION OF THE STUDY
Some limitations in this study should be noted.
1. The exercise was originally conceived to have full district
coverage but because of resource constraints the study was limited only in 3 of
the 8 sub-districts of Kintampo District.
This may have led to no representativeness for the whole
district.
2. Focusing the study only among unmarried young adults
between 15-30 years might have been source of bias about perceptions towards
HIV PCT since it may generate a partial and selective picture rather than a
holistic one. This is of true value since unmarried young adult aged more than
30 years may perceive HIV PCT differently. Also married people, based on their
experiences and testimonies on marriage, whether or not they got married after
undergoing a HIV PCT session, also have a lot of information and strong
perception towards HIV PCT and that should have been normally taken into
account to give a wider picture on the matter. This last limitation was
partially solved in involving parents and old couples in FGD and IDI.
3. In order to reduce interviewer bias, most questions were
close-ended. This might have created loss of some important information which
may-be open-ended questions could have captured.
Nevertheless despite all these limitations, we hope results,
conclusions and recommendations from this study stand true and will help
Kintampo District Health Authorities as reference to plan for health
policy/programmes or further researches related to VCT and premarital
examination implementation.
3.9. RETROINFORMATION AND DISSEMINATION OF THE
FINDINGS
As soon as the study results were released, retro information
was done successively to the DDHS, the DHMT, and the District HIV/AIDS Response
Initiative coordinator and to KHRC team. Copies of the final report were sent
to the DHMT and the KHRC.
Chapter Four
FINDINGS
4.1. SOCIO-DEMOGRAPHIC CHARACTERISTICS OF RESPONDENTS
INVOLVED IN
THE SURVEY
One hundred fifty (150) respondents were interviewed in the
survey, of who 81 (54%) were from Kintampo Sub-District, 41(27%) from Jema
Health Sub-District and 28 (19%) from New Longoro Sub-District. Majority (71%)
were from urbanized settlements.
In total 65 individuals of different socio-demographic
background, 29 (45%) females and 36 (55%) males were part of key informant
participants in the qualitative study, with ages ranging from 20 to 64 years
and a mean age of 30.6 years (SD 11.78). Seventeen of them (26%) ,made up of
the District HIV-AIDS response initiative coordinator, the District Public
Health Nurse in Charge of Family Health Clinic, the different religious
leaders, one traditional herbalist, one laboratory technician, one medical
doctor, 3 newly married couples (old couples), one prospective would-be couple,
one single influential young boy and one counselor, were key informants
contacted for In-Depth Interview (IDI) whereas the majority (74%), made up of
unmarried young adults and parents, took part in Focus Group Discussions.
4.1.13.
DISTRIBUTION OF RESPONDENTS BY AGE AND SEX
The 150 surveyed respondents were unmarried young adults aged
between 15 and 30 years with a mean age of 21.0 years (SD 4.48), the majority
of them (76%) being aged between 15-24 years (age distribution left skewed).
The sex distribution of respondents was slightly skewed with a little but
insignificant predominance of males (51%) [p-value=0.29]. Figure 1 below
describes these features.

4.1.2. EDUCATIONAL BACKGROUND OF
RESPONDENTS
The educational features of respondents in the survey (Figure
2) ranged from those with no formal education to post secondary school level,
majority of them (36%) being in Middle continuation and Junior Secondary
Schools (JSS), constituting a quasi-normal distribution. In both sexes the
trend showed an increased number from primary school level to Middle/JSS level
followed by a progressive sharp decrease of respondents in the subsequent
higher levels up to Post Secondary School, with no respondent at University
level at all. The trend also showed many surveyed males predominated over
females in Middle/JSS and Senior Secondary Schools (SSS) whereas surveyed
females were predominant in Primary and Post secondary schools (Figure 2). The
average number of years successfully completed at the highest level reached by
respondents was 3.
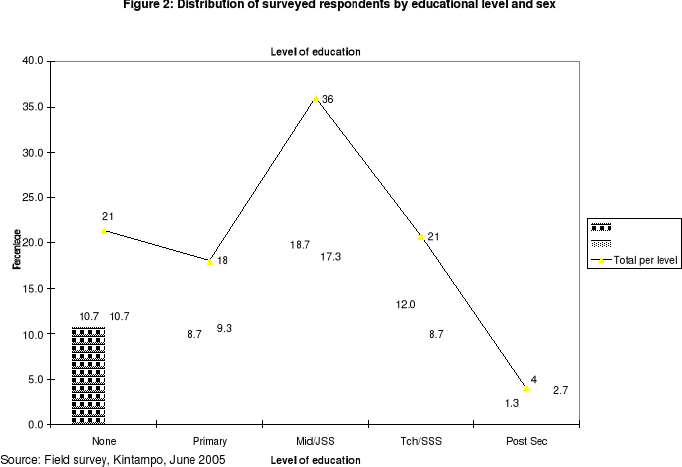
4.1.3. RELIGION, ETHNIC GROUP AND
OCCUPATION BACKGROUND
Majority of responds were mostly Christians (65%), followed by
Moslem (28%), the minority (7%) being without any defined religion.
Almost half part of respondents belonged to Akan (34%) and Mo
(27%) ethnic groups.
A higher proportion of respondents were students (36%),
followed by farmers (16%), with a minority of government or salaried workers
(3%).
All these features are summarized in Figure 3 below.
Figure 3: Distribution of Respondents by Religion, Ethnic
group and Occupation.


4.2. PREMARITAL SEX HISTORY AND HIV-AIDS RISK FACTORS
AMONG SURVEYED RESPONDENTS
Out of 150 respondents, 99(66%) have had premarital sex
already (78% of females and 55% of males), majority involved being females
(58%). Results in Table 3 show that female respondents were 2.97 times more
engaged in premarital sex than males (p-value =0.004116).
|
Table 3: Distribution of respondents according to
premarital sex history and sex.
|
|
Have had sex
|
Statistics (CI 95%, p<0.05)
|
|
Sex
|
Yes
|
No
|
Total
|
OR:2.97 (1.38<OR<6.46)
|
|
Female
|
57 (78%)
|
16 (22%)
|
73(100%)
|
RR: 1.43 (1.13<RR<1.82)
|
|
Male
|
42 (55%)
|
35 (45%)
|
77 (100 %)
|
X2 (Yates): 8.23
|
|
Total
|
99 (66%)
|
51 (34%)
|
150 (100%)
|
p-value: 0.004116
|
|
Source: Field survey, Kintampo, June 2005
|
Respondents in FGD mentioned the following as being the major
contributory factors to premarital sex in Kintampo District:
|
- The fact that Kintampo is highway stop over where over
night girls sell their goods to passengers,
- Curiosity, Peer pressure
- Type of songs and dances broadcast
- Lack of sex education in families,
- Bad dressings (mini skirts, tight clothes, half-naked
clothes): e.g.«Apuskelenke»
- Pornographic films, drug abuse, alcohol
- Unfaithfulness between married couples
|
- Poor parental care,
- Broken homes/marriages,
- Financial problem (poverty),
- Illiteracy and lack of education
- Joblessness, streetism, prostitution
- Modernism which breaks some protective traditional
social norms
- The human nature calling for satisfaction of sexual
physiological need,
- Single parents, - Traveling alone...
|
|
(Source: Compilation from IDIs and FGDs, Our Research
work, Kintampo, June 2005)
|
The age at first sex ranged from a minimum of 10 years up to
a maximum of 25 years and for the whole sample the mean age at first sex was
18 years (SD:2.98). However the mean age at first sex was 18.125 years (SD:2.6)
for females and 18.075 years (SD:3.34) for males, meaning both male and female
respondents engaged in premarital sex at about same age of 18 years . The
earliest age at first sex was 10 years in males and 12 years in females, the
latest age at first sex being 25 years in both sexes. Also the trend showed a
gradual increase of first sex rate as the age increases, the peak age of first
sex being 20 years in males and 18 years in females. Figure 4 describes these
features.

In addition, the number of sexual partners among those who
have had sex ranged from 1 to 15, with a mean of 2.7 (SD:2.38) partners per
respondents.
These findings reinforce trends from qualitative study where
participants attested to the fact that premarital sex was normal in Kintampo
society. This notion is captured in the responses below during IDIs and
FGDs.
|
«There is stage of age that when you reach, something
pushes you into it. And especially these days, the younger girls are very neat
and when you see them, they attract you and you just find yourself
psychologically attracted, so the next steps can follow....»
(FGD: A young boy during a mix boys-girls Christian FGD,
18 years old).
|
|
«In our times, children and young adults were supposed to
be home at 6:00 PM and slept not later than 8:00 PM. This helped us to be free
from premarital sex and its consequences such as STI/HIV-AIDS. But theses days,
if you go round to night in the streets, you find most of children and
adolescents, especially girls still wandering outside, pretending selling goods
while selling rather their bodies. They even commonly say: 'Sex for CFA',
meaning you have CFA or foreigner currency, you have me.»
(IDI: Rev Pastor, Pentecostal Church, Kintampo)
|
|
«Whatever the case, premarital sex cannot just be
eliminated; it is difficult to prevent it. Young boys and girls think it is a
spiritual disease. They said there is stages when you reach you feel like
having sex. And for that matter the best we could do is just to tell them they
should use condom. If you ask them to abstain, you are
lying.»
(FGD: A 54 - year-old traditionalist
father, parent FGD /Ampoma)
|
|
«The fact of Kintampo being in the Middle way from
North to South Ghana is bringing us troubles. Sex workers and young girls
because of stopover all over days and nights feel comfortable in their sex
business. They don't even use condom to protect themselves. All they want is
money. Because men say raw sex is the sweetest, they pay higher fees for it.
The fees are different depending on who the client is. A Ghanaian is asked to
pay 50,000 Cedis, whereas foreigners pay 150CFA per sexual greetings. So
premarital sex in Kintampo has become part of the natural life here. So
HIV/AIDS is part of our every day stuffs. If the situation is to be solved,
then may be the government should make a policy which prohibit all stopovers
here and all sorts of trade overnight. Girls and boys found in the street
overnight should be arrested by the police...»
(One young girl,24years old, KHRC field worker during a
female Moslem FGD in picture No 1)
|
|
|
«In my opinion, I think it is wise to test for
HIV/AIDS before one marries. This is because one may not know the past life of
the fellow fiancé(e).In this modern times, marriages are no longer done
holily due to the fact that most would-be couples might have engaged in
premarital sex that expose to all kind of risks. So since I am not sure
premarital sex in younger adults could be totally eradicated in this spoiled
town, I fully support the view for HIV premarital counseling and testing,
another alternative to fight HIV/AIDS.»
(IDI: A young Christian boy, 25 years old, in Picture No
2)
|
4.3. GENERAL AWARENESS AND KNOWLEDGE OF RESPONDENTS ON
HIV/AIDS,
VCT AND HIV PCT
|
Table 4: Trend of general awareness and knowledge on
HIV/AIDS, VCT and HIV PCT
[Chi-Square, Note: X2(Y)=Yates corrected
chi-square, p<0.05, CI:95%]
|
|
Indicators on awareness and knowledge on HIV/AIDS,
VCT and HIV PCT
|
Yes (%)
Male
(N=77)
|
Yes (%)
Female
(N=73)
|
Yes (%)
Total
(N=150)
|
p-value
X2*
OR
|
|
1.Knows or have known a young adult who suffers/suffered from
HIV AIDS
|
32(41.6)
|
31(42.5)
|
63(42.0)
|
OR=0.96
p=0.95
|
|
2. Know that unprotected pre-marital sex with casual/multiple
partners is a risky behaviour that could expose to STI-HIV/AIDS
|
74(96.1)
|
71(97.1)
|
145(96.7)
|
X2=1.95
p=0.375
|
|
3. Know that a child could be born HIV positive from sexual
union of his/her parents/mother
|
70(90.9)
|
66(90.4)
|
136(90.7)
|
X2=5.6
p=0.0604
|
|
4. Know that HIV/AIDS does not have any effective cure yet
|
71(92.2)
|
71(97.3)
|
142(94.7)
|
OR=0.33,
p=0.31
|
|
5. Know that not all sexual unions and marriages are safe and
good for health of both partners and offspring:
|
47(61.0)
|
45(61.6)
|
92(61.3)
|
X2=3.39
p=0.1833
|
|
5.1.Know that HIV/AIDS makes unsafe sexual unions
and marriages
|
33(42.9)
|
26(35.6)
|
59(39.3)
|
X2=1.15
p=0.7664
|
|
5.2. Know that others diseases a part from HIV/AIDS
makes
unsafe some sexual unions and marriages
|
7(9.1)
|
7(9.6)
|
14(9.3)
|
|
5.3. Know that both HIV/AIDS and others diseases make
unsafe sexual unions and marriage
|
9(11.7)
|
12(16.4)
|
21(14)
|
|
6. Recognize that they will consider health status as core
criteria when they choose their marriage partners
|
74(96.1)
|
68(93.2)
|
142(94.7)
|
OR=1.8
X2(Y)=0.19
|
|
7. Way to assess «Good Health Status» of marriage
partner before marriage: 7.1.By observing his/her appearance
|
3(3.9)
|
4(5.5)
|
7(4.7)
|
-
|
|
7.2.By asking close family
member
/friends
|
5(6.5)
|
5(6.8)
|
10(6.7)
|
|
7.3.Through premarital
medical
examination
|
66(85.7)
|
58(79.5)
|
124(82.7)
|
|
8. Have ever heard about HIV voluntary counseling and testing
(VCT)
|
53(68.8)
|
55(75.3)
|
108(72)
|
OR=0.7, p=0.48
|
|
9. Have ever heard about HIV premarital counseling and
testing
|
62(80.5)
|
65(89)
|
127(84.7)
|
OR=0.5, p=0.22
|
|
10. Sources of information about HIV PCT :
10.1.Radio/TV/Cinema/Video
|
61(83.5)
|
52(73.2)
|
113(78.5)
|
-
|
|
10.2. Churches or
mosques
|
22(30.1)
|
30(42.2)
|
52(36.1)
|
|
10.3.Friends/third
person
|
15(20.5)
|
32(45)
|
47(33)
|
|
10.4. Health workers
|
26(35.6)
|
20(28.2)
|
46(31.9)
|
|
10.5.Schools/University
|
23(31.5)
|
18(25.3)
|
42(29.2)
|
|
10.6.News papers or
books or posters
|
16(22)
|
11(15.5)
|
27(19.75)
|
|
10.7 .Parents
|
10(17)
|
10(14)
|
20(14)
|
|
10.8.Conference/youth
camp
|
5(6.8)
|
2(2.8)
|
7(4.9)
|
|
10.9. Internet
|
2(2.7)
|
3(4.2)
|
5(3.5)
|
|
10.10. Others sources
|
1(1.36)
|
1(1.4)
|
2(1,38)
|
|
11. Know that HIV PCT is one of the main measures to limit the
spread of HIV/AIDS in new couples
|
70(91)
|
68(93)
|
138(92)
|
X2=1.01
p=0.6
|
|
12. Know of someone or a couple who underwent HIV PCT before
marriage
|
26(34)
|
29(40)
|
55(37)
|
X2(Y)= .35
p=0.55, OR=0.7
|
|
13. Knowledge of who is required to undergo Premarital
Counseling and Testing (PCT): 13.1.The male partner
|
11(14.3)
|
2(2.7)
|
13(8.7)
|
-
|
|
13.2.The female partner
|
1(1.3)
|
8(11)
|
9(6)
|
|
13.3.Both partners
|
65(84.4)
|
63(86.3)
|
128(85.3)
|
|
14. Know major advantages of HIV PCT:
|
|
|
|
-
|
|
14.1.To know about their health and HIV status so
that
they decide responsibly about
marriage
|
67(87)
|
61(83.5)
|
128(85.3)
|
|
14.2.Stability and safety in marriage
|
36(47)
|
32(44)
|
68(45)
|
|
14.3.It strengthens marital relationship and
enhance
marriage satisfaction
|
23(30)
|
20(27.4)
|
43(29)
|
|
14.4.To ensure fertility in couples
|
17(22)
|
14(19)
|
21(14)
|
|
Source: Field survey, Kintampo, June 2005
|
In general, the main trend of awareness and knowledge of
respondents on HIV/AIDS, VCT and HIV PCT summarized in Table 4 are the
following:
Less than half of respondents of both sexes knew of any young
adult who suffer/suffered from or died of HIV/AIDS, male respondents knowing
less than females, but with no statistical significant difference between both
sexes.
|
«Yes, HIV/AIDS is common here. When you get
it you will not die early. My own 18 years old Junior Uncle had it. He would
grow thin and later grow big, grow thin and grow big again, and long round he
finally grew thin, became so sickly and died. He might have left the insect to
his girl friends, so those who will later marry them will come across deadly
spouses. I am afraid of this.»
(IDI: A 57-year-old Traditional herbalist/Ampoma,
father of 5 children, Picture No 3).
|
|
More than 96% of both males and females respondents knew
unprotected premarital sex with casual and multiple partners expose to
HIV/AIDS, no statistical significant difference between them.
Also more than 90% of both males and females knew that HIV
could be transmitted from mother to child through sexual union of parents,
again the trend shows no statistical significant difference between the two
categories.
|
«HIV/AIDS is a big curse. Children and generations
can all become infected and affected by it from their parents. It brings
problems to the family and the whole nation. So many widows and widowers, so
many orphans, so many deaths. No longer happiness in family at all. So if this
could be prevented by like HIV Premarital check-up for current younger people,
it is better.»
(A 32-year-old female parent: FGD of Moslem
mothers)
|
94.7% of respondents were aware that HIV/AIDS does not have
any cure yet (no statistical difference between both sexes). This finding is
obvious since in Kintampo society even some traditional healers are aware of
this fact. They are currently taking advantage of the inexistence of any
effective cure against HIV/AIDS to attract the community members to their
services, pretending they have traditional drug to cure HIV/AIDS (See
illustrative pictures below):
Pictures 4 and 5: Poster of an herbalist on the main road just
at Apaaso, Kintampo Police barrier
Source: Our Research Inquiry on
the field, Pictures No 4 and 5.
Majority (>60%) of both male and female respondents were
similarly aware that not all sexual unions and marriages are safe and good for
health of both partners, and their offspring ( no statistical significant
difference). However, surprisingly fewer (42.9% of males and 35.6% of females)
knew that HIV/AIDS makes unsafe sexual union and marriage.
|
«We all know not all sexual unions and marriages are
healthy for spouses and their children. Many diseases can bring problems and
instability in the family. So sometimes we consider all these before giving our
children to somebody for marriage»
(A 30-year-old young parent, FGD of Traditionalist
fathers/Ampoma)
|
A higher number of both males (96.1%) and females (93.2%) were
similarly aware that they will consider health status as core criteria when
they will choose their marriage partners.
In all FGD and IDI, all participants also strongly considered
health status is the major criteria in choosing spouses.
|
«Well. No body wants to die or to kill
him(her)self. Because when you see that your prospective spouse is having the
disease like HIV, obviously you go away from him/her to protect your self. This
is the least natural auto defense a normal human being could
do».
(A 26-year-old mother, FGD of Traditionalist
mothers)
|
|
«Do not take your self to where you will perish or
where you will endanger others. If you do, it is equivalent to committing
suicide or homicide. The prophet said you should not cheat and somebody should
not also cheat you...The prophet talked about `examine a woman very well before
taking her into marriage...Because it is from this examination you will be able
to tell whether you should go ahead or stop the marriage process'. It is a
matter of life or death. Anything you see that could shorten your life and even
the marriage is significant. Nothing is as dangerous as HIV/AIDS
today».
(IDI: The Imam, Kintampo Central Mosque, Picture No
6)
|
|
Although the neat majority of males (85.7%) and of females
(79.5%) recognized premarital medical examination as the right way to assess
«Good health status» of their marriage partners, a few part of them
thought they would assess it simply by observation of external appearance
(4.7%) or by asking close family members (6.7%). There was no significant
statistical difference between the trends in both sexes.
In all FGDs and IDIs all participants said premarital medical
examination was not included in the marriage procedures in Kintampo and showed
a great disagreement to this sort of managing marriage, saying PCT was very
important.
|
«No! In the older times it was good not to
conduct premarital examination, but these days it is not good to skip it. In
the past-time there was no premarital sex epidemic like today. There were no
doctors, no tests nor laws to encourage premarital examination. But still there
were rudimentary ways to study good health status of a person to marry. So
nowadays medical examination must be a law in our society and
churches.»
(A 45-year-old Christian father: FGD of Christian
parents, Picture No 7).
|
|
|
«At first we weren't aware of premarital examination
in our Islamic religion. But now we have realized that it should be done
before marriage since some diseases are hidden»
(A 22-year-old mother: FGD of Moslem mothers/Kintampo
central mosque, Picture No 8).
|
|
«I may trust my child and if someone comes to marry
her, I have to see it that premarital examination is done, before I accept the
marriage go ahead»
(A 46-year- old mother: FGD of Traditionalists
mothers/Ampoma).
|
Surprisingly, although HIV PCT is a specific type of VCT,
majority of respondents (84.7%) had heard more about HIV PCT than VCT itself
(72%). No significant statistical difference in males and females trends.
The top source of information on HIV PCT among respondents was
through Radio, TV, Cinema or Video (78.5%), the second source being churches
and mosques (36.1%), followed by friends or third person (33%). Worst still
parents were at the seventh position (14%).
In both sexes, HIV PCT was well known as one of the major
measures to limit the spread of HIV/AIDS in new couples. No statistical
difference between the trends in the 2 groups.
|
«Premarital examination is a major measure
that helps reduce the spread of the diseases in new couples. So the government
should make it a law and anyone who has HIV should be rejected and killed, so
that he/she does not spread it to others»
(A 45-year-old mother: FGD of Traditionalists
mothers/Ampoma)
|
Less than half (37%) of respondents knew of someone or couple
who underwent a HIV PCT before marriage.
Large majority of both males (84.4%) and females (86.3%)
recognized that both partners are required to undergo PCT.
Also majority of respondents in both sexes (85.3%) knew the
first main advantage of HIV PCT (To know about their health and HIV status so
that they decide responsibly about marriage), less than half of them knew the
2nd advantage (To ensure stability and safety in marriage) [45%] and
the 3rd one (It strengthens marital relationship and enhances
marriage satisfaction) [29%], with few of them (14%) considering HIV PCT
advantage is to ensure fertility in couples.
|
«Oh yes! Premarital counseling and testing on
HIV is useful. It helps you to know your status regarding HIV. It advises us on
how to behave afterwards. It also strengthens marriage relationship and
faithfulness in couples. It is like an exam. When you don't want to become
last and you find out that you don't have HIV, you wouldn't like to fornicate
again». (A 25-year-old mother: FGD of traditionalist
mothers/Ampoma)
|
4.1. SCORE OBTAINED ON AWARENESS AND KNOWLEDGE
OF
RESPONDENTS ON HIV PCT
Using a scale of measurement described in point 3.6.2.3 ,
Findings in Table 5 suggest that as a whole, all different groups of
respondents in different categories (age group, residence, sub-districts, sex,
occupation, religious group, ethnic group, educational level..) had
Good knowledge on HIV PCT since none of the categories ranked
below the cut-off mean score of 11 below which we would consider there is poor
knowledge. Majority of different groups described in Table 5 fell in Average
Good Knowledge, except 3 groups which fell into Adequate Good knowledge (AKAN,
SSS and Post-middle college respondents). The mean score of knowledge for the
whole sample was 15.72 [SD2.8], falling in average level. Most mean scores in
different categories studied in table 5 varied between 14.4 and 17.5 (over the
total score 22 ) and did not show big significant differences between them,
meaning the adequacy of knowledge on HIV PCT seems similar in all these
different groups. . Only one category had a mean score corresponding to the
cut-off point (Respondents of post-secondary school level with a mean score of
11).
Also when one considers the individual scores as it is shown
in Figure 5 below, large proportion of respondents (97 % beyond the cut-off
line from average score 11 and over) proved «Good Knowledge»
(GK) on HIV PCT, with 41.3% scoring «Adequate Good
Knowledge» versus 55.7% scoring «Average Good
Knowledge». On the other hand a minority of respondents proved
«Poor Knowledge» (3 % below average score 11). The
trend shows a right skewed distribution with a peak at score 15 (17.3%), then
the number of respondents gradually decreases as the score increases, with few
people scoring the maximum (1.3%).
|
Table 5: Level of knowledge on HIV PCT among
respondents
|
|
Background characteristic
|
Total score computed in the whole(n)
|
Range score obtained
|
Mean score obtained (u) [SD]
|
Conclusion on level of knowledge*
|
|
Age : 15-19
|
942 (n=61)
|
7-22
|
15.4[SD=2.87]
|
Average GK
|
|
21-24
|
843 (n=53)
|
10-22
|
15.9[SD=2.54]
|
Average GK
|
|
25-30
|
574 (n=36)
|
4-21
|
15.9[SD=3.94]
|
Average GK
|
|
|
|
|
|
|
Residence: Urban
|
1673(n=107)
|
4-22
|
15.6[SD=2.9]
|
Average GK
|
|
Rural
|
686 (n=43)
|
11-22
|
15.9[SD=2.8]
|
Average GK
|
|
|
|
|
|
|
Sub districts: K'po
|
1259(n=81)
|
4-22
|
15.5[SD=2.7]
|
Average GK
|
|
JH
|
672(n=41)
|
7-22
|
16.4[SD=3.3]
|
Average GK
|
|
NL
|
428(n=28)
|
11-19
|
15.3[SD=2.3]
|
Average GK
|
|
|
|
|
|
|
Sex M
|
1208(n=77)
|
4-22
|
15.68[SD=2.6]
|
Average GK
|
|
F
|
1151(n=73)
|
7-22
|
15.76[SD=3.1]
|
Average GK
|
|
|
|
|
|
|
Educ. level: None
|
489(n=32)
|
11-20
|
15.2[SD=2.26]
|
Average GK
|
|
Primary
|
393(n=27)
|
8-20
|
14.5[SD=2.75]
|
Average GK
|
|
Middle/JSS
|
844(n=54)
|
7-22
|
15.6[SD=2.83]
|
Average GK
|
|
Tech/SSS/sec sch
|
544(n=31)
|
14-22
|
17.5[SD=2.15]
|
Adequate GK
|
|
Post.mid college
|
69 (n=4)
|
15-20
|
17.2[SD=2.06]
|
Adequate GK
|
|
Post secondary S.
|
22 (n=2)
|
4-18
|
11[SD=9.89]
|
Average GK
|
|
Occupation: Farmer
|
365(n=24)
|
11-22
|
15.2[SD=2.8]
|
Average GK
|
|
Gov.Workers
|
58(n=4)
|
4-22
|
14.5[SD=7.59]
|
Average GK
|
|
Trader
|
334(n=20)
|
12-21
|
16.7[SD=2.6]
|
Adequate GK
|
|
Student
|
854(n=54)
|
10-21
|
15.8[SD=2.3]
|
Average GK
|
|
Others
|
748(n=48)
|
7-20
|
15.5[SD=2.94]
|
Average GK
|
|
Religion Christian
|
1558(n=98)
|
4-22
|
15.9[SD=2.9]
|
Average GK
|
|
Moslem
|
649 (n=42)
|
8-21
|
15.4[SD=2.57]
|
Average GK
|
|
None
|
151(n=10)
|
12-22
|
15.1[SD=2.96]
|
Average GK
|
|
Tribe: Akan
|
867(n=50)
|
4-22
|
17.3[SD=3.3]
|
Adequate GK
|
|
Mo
|
640(n=41)
|
11-19
|
15.6[SD=1.8]
|
Average GK
|
|
Others
|
852(n=59)
|
8-20
|
14.4[SD=2.8]
|
Average GK
|
|
Total sample
|
2359 n=150)
|
4-22
|
15.72 [SD2.8]
|
Average GK
|
|
*Note: Scale of measurement of level of knowledge on HIV PCT=
|
|
If u < 11: POOR knowledge (PK)
If u = 11: GOOD Knowledge (GK),
|
|
11-16.5: Average GK and >16.5:
Adequate GK.
|
|
Source: Field survey, Kintampo, June 2005.
|
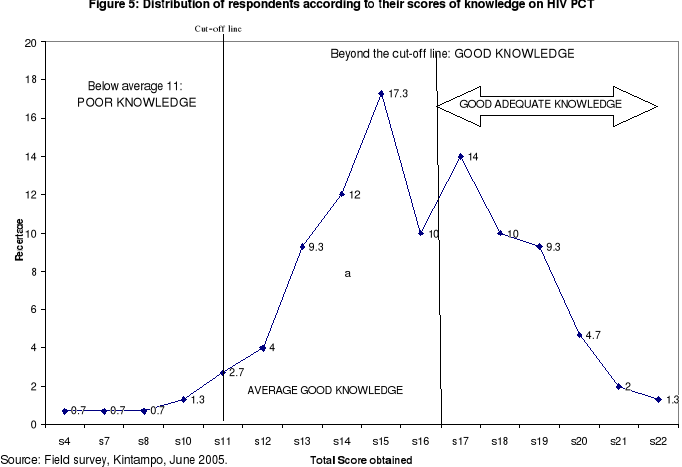
In figure 6, we see that respondents from rural parts knew
slightly more about HIV PCT than those coming from urban area, with the minimum
score of 11 and a mean score of 16.5 for rural respondents versus a minimum
score of 4 and a mean score of 13 among urban respondents. However the
difference in the trends of scores of knowledge between the two groups was not
statistically significant (p-value=0.25). The peak score was 15 among rural
respondents (20.9%) versus 2 peak scores of 15 (15.9%) and 17 (15.9%) among
urban respondents. Higher proportion of respondents who got maximum score of 22
were from rural parts (2.3%) as compared to those from urban ones (0.9%).
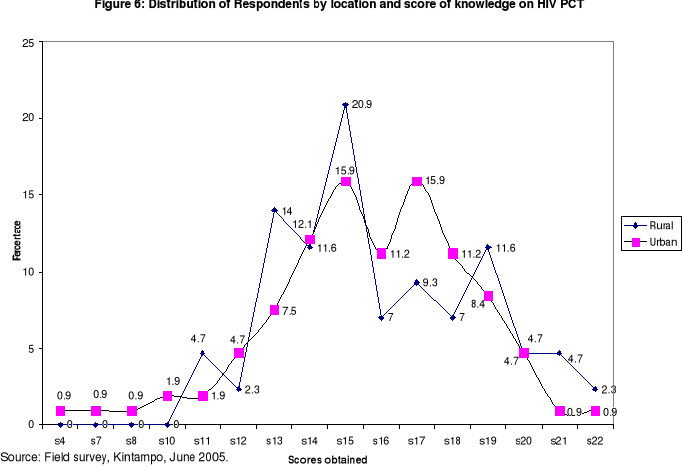
4.5. GENERAL PERCEPTION OF RESPONDENTS TOWARDS HIV
PCT
Findings in Table 6 below summarize the trend of how
respondents perceived HIV/AIDS and HIV PCT when the survey was carried out. The
following observations can be highlighted:
Large majority of Male (92.2%) as well as female (94.5%)
respondents perceived that although healthy they or their fiancé(e)s
could be unknown carrier of HIV AIDS. Females presented a slight higher risk
perception than males although there is no significant statistical difference
(p=0.81). This perception was expressed as well in FGDs carried out:
|
«Because of money, a woman forced her
daughter to marry a man who came from London. This man was apparently healthy.
But who knew he was having it? Just 2 years and six months later he started
showing the symptoms and later died. The poor lady is also dying».(A
27-year-old boy: FGD Christian young adults)
|
|
Table 6: Trend of general perception of respondents towards
HIV PCT
|
|
Indicators on perception towards HIV
PCT
|
Yes (%)
Male
(N=77)
|
Yes (%)
Female
(N=73)
|
Yes (%)
Total
(N=150)
|
p-value
X2*
OR
|
|
1.Perceive that one or one's partner [fiancé (e)]
though
apparently healthy can be an unknown carrier of
HIV/AIDS that could be detected during PCT
(Risk perception)
|
71
(92.2)
|
69
(94.5)
|
140
(93.3)
|
OR=0.7
p=0.81
|
|
2.Perceive that HIV-AIDS is a very dangerous/fatal disease
(Perceived severity of HIV/AIDS)
|
77
(100.0)
|
73
(100)
|
150
100.0
|
-
|
|
3.Perceive that there is a high risk of getting married
unknowingly to an HIV infected person and of becoming
HIV infected when two fiancés do not attend any
premarital medical examination on HIV test (Perceived
threat of contracting HIV in case one marries without
attending HIV PCT)
|
74
(96.1)
|
73
(100)
|
147
98.0
|
-
|
|
4.Believe that HIV Premarital Counseling and Testing
(PCT) is important (Perceived benefit of HIV PCT)
|
77
(100.0)
|
73
(100.0)
|
150
(100.0)
|
-
|
|
5.Believe they are self-confident and able to decide
themselves to undergo HIV PCT (Perceived self efficacy
towards HIV PCT)
|
76
(98.7)
|
71
(97.3)
|
147
(98.0)
|
-
|
|
6.Believe that their family will support them or encourage
them to perform HIV PCT before getting married
(perceived HIV PCT as a subjective -family norm a)
|
75
(97.4)
|
69
(94.5)
|
144
(96.0)
|
-
|
|
7. Believe that their family will support them or
encourage
them to perform HIV PCT before getting married
(perceived HIV PCT as a subjective-peer norm b)
|
71
(92.2)
|
60
(82.2)
|
131
(87.3)
|
OR=2.5
p=0.11
|
|
8. Perceive that HIV PCT should be institutionalized in the
district (Perceived HIV PCT as a social norm)
|
76
(98.7)
|
72
(98.6)
|
148
(98.7)
|
OR=1.0
p=0.5
|
|
8.1.Perceive that HIV PCT should be made
compulsory
|
48 (63)
|
42(58)
|
90(61)
|
OR=1.2
p=0.66
|
|
8.2.Perceive that HIV PCT should be made
optional
|
28(37)
|
30(42)
|
58(39)
|
|
9. Perceive there are some barriers to HIV PCT acceptance
and implementation in Kintampo (perceived barrier to
HIV PCT)
|
61
(79.2)
|
60
(82.2)
|
121
(80.7)
|
OR=0.8
p=0.79
|
|
10. Perceive there is the need of implementing HIV PCT
services in Kintampo district in the fight against
HIV/AIDS in new couples (Perceived need of HIV PCT
services)
|
76
(98.7)
|
73
(100.0)
|
149
(99.3)
|
-
|
|
11. Have the willingness to undergo HIV PCT with their
fiancé (e) before Marriage.
|
75
(97.4)
|
72
(98.6)
|
147
(98.0)
|
-
|
|
12. Perceive they are ready to know and accept their HIV
test result after HIV PCT
|
75
(97.4)
|
70
(95.9)
|
145
(96.7)
|
-
|
|
[Chi-Square, Note: X2(Y)=Yates corrected
chi-square, p<0.05, CI:95%]
|
|
Source: Field survey, Kintampo, 2005.
|
The totality of respondents (100%) in both sexes perceived the
severity of HIV/AIDS and subsequently also perceived perfectly the importance
of HIV PCT. Also most of them perceived the threat of contracting HIV/AIDS in
case they marry without performing the HIV test. This trend also emerged from
qualitative discussions:
|
«In this time of HIV/AIDS, there are no more
jokes in marriage matters. HIV/AIDS has totally limited the freedom and the
right of people to marry. Because of HIV/AIDS you have to carefully choose your
marriage partner. And the right way to do it is to perform HIV test before you
go ahead. Meeeeeee! (with strong gesture), I cannot marry a HIV partner. God
forbid!»
(A 22-year-old single girl: FGD Moslem
girls)
|
Large majority of respondents in both sexes (98%) believed
they were able personally to perform HIV PCT.
|
«It is the matter of my own life.
Irrespective of whatever views from people or family members , me I know I have
to perform HIV test before marriage, so that I guarantee a bright future in my
family»
(A 24-year-old girl: FGD Christian young
adult).
|
Large majority of respondents perceived that the family
members and peers could support and encourage them towards HIV PCT.
Large majority of respondents (98.7%) in the survey perceived
HIV PCT should be institutionalized in Kintampo District, with the majority
(61%) perceiving it should be compulsory versus the minority (39%) saying it
should be optional rather.
This is supported by findings from qualitative study where
almost majority of participants opted HIV PCT should be compulsory with a few
of them opting it should be optional.
Respondents of both sexes almost universally perceived the
need of implementing HIV PCT services in Kintampo District (99.3%) although
they also recognized there were some barriers to its implementation and
acceptance (80.7%).
|
«It has to be implemented. If so it will help
those who understand its importance. Barriers are for those who just don't make
an effort to understand its usefulness. So instead of leaving two people to
death, it's better to save one of them. Therefore this service is needed since
it will save so many lives».
( A 24-year-old girl: FGD Moslem
girls).
|
Finally Table 6 shows that almost all the respondents in both
sexes had the willingness to undergo HIV PCT before their marriage (98.0%) and
said they were ready to know and accept their HIV test results after PCT
(96.7%).
The general trend showed no significant difference of views in
males and females, meaning they similarly perceived HIV PCT.
4.6. SCORES OBTAINED ON PERCEPTIONS OF RESPONDENTS
TOWARDS HIV PCT
Using a scale of measurement described in point 3.6.2.3 (see
Methodology), Table 7 and Figure 7 show that the entire totality (100%) of
respondents in both sexes had «adequate positive
perception» towards HIV PCT irrespective of their
different socio-demographic backgrounds , the minimum score obtained being 18,
with a mean score of 21.81 (SD=1.16 ). The curve is right skewed with no great
difference between males (mean score= 21.7[SD=1.2]) and females (mean score=
21.8[SD=1.13]). 20-28% of respondents scored the maximum of 23 marks.

|
Table 7: Level of perception towards HIV PCT among
respondents
|
|
Background characteristic
|
Total score computed in the whole(n)
|
Range score obtained
|
Mean score obtained (u) [SD]
|
Conclusion on level of perception*
|
|
Age : 15-19
|
1333 (n=61)
|
19-23
|
21.8[SD=1.04]
|
AP
|
|
21-24
|
1160 (n=53)
|
18-23
|
21.8[SD=1.12]
|
AP
|
|
25-30
|
779 (n=36)
|
18-23
|
21.6[SD=1.4]
|
AP
|
|
Residence: Urban
|
2334(n=107)
|
18-23
|
21.8[SD=1.3]
|
AP
|
|
Rural
|
938 (n=43)
|
18-23
|
21.8[SD=1.07]
|
AP
|
|
Sub Districts: K'po
|
1751(n=81)
|
18-23
|
21.6[SD=1.09]
|
AP
|
|
JH
|
913(n=41)
|
19-23
|
22.2[SD=0.9]
|
AP
|
|
NL
|
608(n=28)
|
18-23
|
21.7[SD=1.4]
|
AP
|
|
Sex: M
|
1678(n=77)
|
18-23
|
21.7[SD=1.2]
|
AP
|
|
F
|
1594(n=73)
|
18-23
|
21.8[SD=1.13]
|
AP
|
|
Educational level:
None
|
720(n=32)
|
18-23
|
21.8 [SD=1.18]
|
AP
|
|
Primary
|
591(n=27)
|
19-23
|
21.8[SD=1.12]
|
AP
|
|
Middle/JSS
|
1151(n=54)
|
18-23
|
21.7[SD=1.3]
|
AP
|
|
Tech/SSS/sec sch
|
679(n=31)
|
19-23
|
21.9[SD=0.87]
|
AP
|
|
Post.mid college
|
89 (n=4)
|
21-23
|
22.5[SD=0.9]
|
AP
|
|
Post secondary S.
|
42 (n=2)
|
19-23
|
21[SD=2.8]
|
AP
|
|
Occupation: Farmer
|
524(n=24)
|
19-23
|
21.8[SD=1.27]
|
AP
|
|
Gov.Workers
|
86(n=4)
|
19-23
|
21.5[SD=1.7]
|
AP
|
|
Trader
|
432(n=20)
|
18-23
|
21.6[SD=1.3]
|
AP
|
|
Student
|
1175(n=54)
|
19-23
|
21.7[SD=1.1]
|
AP
|
|
Others
|
1055(n=48)
|
18-23
|
21.9[SD=1.08]
|
AP
|
|
Religion: Christian
|
2158(n=98)
|
18-23
|
21.7[SD=1.16]
|
AP
|
|
Moslem
|
893 (n=42)
|
18-23
|
21.7[SD=1.19]
|
AP
|
|
Others
|
221(n=10)
|
20-23
|
22.1[SD=1.19]
|
AP
|
|
Tribe: Akan
|
1096(n=50)
|
18-23
|
21.9[SD=1.04]
|
AP
|
|
Mo
|
908(n=41)
|
18-23
|
21.6[SD=1.3]
|
AP
|
|
Others
|
1268(n=59)
|
18-23
|
21.8[SD=1.16]
|
AP
|
|
Total sample
|
3272 n=150)
|
18-23
|
21.8[SD=1.16]
|
AP
|
|
*Note: Scale of measurement of level of perception on HIV
PCT=
If u < 11.5: Negative or bad perception
If u = 11.5: Positive (high, good)perception:
11.5-17.5: Average Positive perception and
>17.5=Adequate Positive perception (AP)
|
|
Source: Field Survey, Kintampo, June 2005.
|
4.7. RELATIONSHIP BETWEEN SCORE OF KNOWLEDGE AND SCORE
OF
PERCEPTION AMONG
RESPONDENTS.
As it can be implied in Table 8 below, there was a weak
positive linear relationship between the two variables which was statistically
significant (p-value 0.007). The score of perception slightly
increases as the score of knowledge increases. But even respondents with poor
score of knowledge also had higher score of perception.
|
Table 8: Linear Regression: Regress score of perception
=score of knowledge, CL =95%
|
|
Linear Regression: Regress Pscore=Kscore p-value
=95%
|
|
Variable
|
Coefficient
|
Std Error
|
F-test
|
P-Value
|
|
Score of knowledge
|
0.088
|
0.032
|
7.4156
|
0.007
|
|
CONSTANT
|
20.422
|
0.519
|
1545.6573
|
0
|
|
Correlation Coefficient: r^2=0.05
|
|
Source
|
df
|
Sum of Squares
|
Mean Square
|
F-statistic
|
|
Regression
|
1
|
9.675
|
9.675
|
7.416
|
|
Residuals
|
148
|
193.098
|
1.305
|
|
|
Total
|
149
|
202.773
|
|
|
|
Source: Field survey, Kintampo, June 2005.
|
From Table 8, we derived the model of the form: Y=
á + ßX, where Y is the score of perception and X the
score of knowledge towards HIV PCT.
The regression straight line fits to the following model:
Y=20.422+0.088X
Using this modal we could predict the score of perception of
any unmarried young adults based on his/her score of knowledge in answering to
the defined questions in the questionnaire. Thus for instance a respondent with
a score of knowledge of 10 would have a score of perception of 21.302.
4.8. FACTORS INFLUENCING PERCEPTION OF THE NEED OF HIV
PCT
SERVICES
|
Table 9. Factors (predictors) influencing Perceived
need of HIV PCT service (p1) among unmarried young adults in
Kintampo District
|
|
Variables
|
Coefficient
|
SE
|
Z-test*
|
p-value
>Z
|
Odds ratio
(95%CI Odds ratio)
|
|
Intercept (constant á1 )
|
-35.38
|
21.29
|
-1.6
|
0.096
|
-
|
|
Socio-Demographic Background:
(X1) Age
|
0.2983
|
0.3082
|
0.967
|
0.333
|
1.3 (0.7, 2.5)
|
|
(X2)Sex (Female)
|
2.975
|
2.131
|
1.39
|
0.16
|
19.5 (0.3, 1278)
|
|
(X3)Place of residence (Urban)
|
-1.622
|
2.366
|
-0.68
|
0.492
|
0.19 (0.002, 20.4)
|
|
(X4) Religious group (Christian)
|
1.717
|
2.516
|
0.68
|
0.49
|
5.57 (0.04, 773)
|
|
(X5)Ethnic group (Akan & Mo)
|
1.0331
|
2.5015
|
0.413
|
0.679
|
2.8 (0.02, 378.4)
|
|
(X6) Level of education (Post Primary)
|
1.418
|
2.446
|
0.57
|
0.56
|
4.13 (0.03, 500)
|
|
(X7) Profession (Student/Pupil)
|
1.4105
|
2.995
|
0.470
|
0.637
|
4.097(0.01, 1452.1)
|
|
(X8) Premarital sex history : Have had
premarital sex (Yes)
|
-2.727
|
2.768
|
-0.98
|
0.324
|
0.06 (0.0003, 14.8)
|
|
(X9) SCORE (LEVEL) OF KNOWLEDGE
ON HIV/ PCT**
|
-0.017
|
0.375
|
-0.04
|
0.96
|
0.98 (0.47, 2.1)
|
|
(X10) SCORE (LEVEL) OF PERCEPTION
TOWARDS HIV/PCT**
|
1.4974
|
0.8998
|
1.664
|
0.096
|
4.47 (0.8, 26.1)
|
|
*Z-test, p-value<0.05 , ** See ANNEX 5 to view variables
used in scoring scales
|
|
Logit Model: Ln[p1/ (1-
p1)]=-35.38+0.2983 X1+ 2.975X2-1.622
X3 + 1.717X4 +1.0331X5
+ 1.418X6 +1.4105X7
-2.727X8 - 0.017X9
+1.4974X10
|
|
Source: Field survey, Kintampo, June 2005.
|
Although there is no significant association between dependant
variable and explanatory variables under study, Table 9 above demonstrates the
following:
1. Perception of the need of HIV PCT was inversely
(negatively) associated with Urban residence, with the fact of having had
premarital sex and with score (level) of knowledge.
2. Perception of the need of HIV PCT service was positively
associated with increased level of perception towards HIV PCT, age, being
female, Christian, being of Akan and Mo ethnic group, being of post-primary
educational level and being student.
4.9. FACTORS INFLUENCING WILLINGNESS TO UNDERGO HIV
PCT
Table 10 below shows that there was only one reliable positive
predictor of willingness to undergo HIV PCT. This predictor was the readiness
of a respondent to know and accept his/her HIV result. In fact willingness to
undergo HIV PCT was strongly associated with readiness of a respondent to know
and accept his/her HIV result (p<0.001), with Odds ration
far exceeding the constant (1 x constant E12= 162754.79).
|
Table 10. Factors (predictors) influencing willingness
to undergo HIV PCT service (p2) among unmarried young adults in
Kintampo District
|
|
Variables
|
Coefficient
|
SE
|
Z-test*
|
p-value
>Z
|
Odds ratio
(95%CI Odds ratio)
|
|
Intercept (constant á2 )
|
-39.715
|
15.934
|
-2.5
|
0.0127
|
*
|
|
Socio-Demographic Background:
(X'1) Age
|
-0.0296
|
0.1839
|
-0.2
|
0.8722
|
0.9 (0.7,1.4)
|
|
(X'2)Sex (Female)
|
1.2901
|
1.252
|
1.03
|
0.3028
|
3.6 (0.3,42.3)
|
|
(X'3)Place of residence (Urban)
|
1.1279
|
1.3789
|
0.8
|
0.4134
|
3.1(0.2, 46.1)
|
|
(X'4) Religious group (Christian)
|
1.2919
|
1.5037
|
0.86
|
0.3903
|
3.6 (0.2, 69.3)
|
|
(X'5) Ethnic group (Akan & Mo)
|
0.9243
|
1.4945
|
0.62
|
0.5363
|
2.5 (0.1, 47.1)
|
|
(X'6) Level of education
(Post Primary)
|
-1.2049
|
1.434
|
-0.84
|
0.4008
|
0.3 (0.01, 5.0)
|
|
(X'7) Profession (Student)
|
-0.3604
|
1.7713
|
-0.2
|
0.8387
|
0.7 (0.02,22.4)
|
|
(X'8) Premarital sex history : Have had
premarital sex (Yes)
|
-1.5237
|
1.6286
|
-0.9
|
0.3495
|
0.2 (0.01,5.3)
|
|
(X'9) SCORE (LEVEL) OF KNOWLEDGE ON HIV/
PCT**
|
0.1913
|
0.2191
|
0.9
|
0.3826
|
1.2 (0.8, 1.9)
|
|
(X'10) SCORE (LEVEL) OF PERCEPTION TOWARDS
HIV/PCT**
|
0.7263
|
0.5674
|
1.3
|
0.2006
|
2.1(0.7, 6.3)
|
|
(X'11) Perceived need of HIV PCT
service (Yes)
|
-3.1371
|
7.3989
|
-0.4
|
0.6716
|
0.04 (0.0, 86196)
|
|
(X'12) Perceived need of confidentiality and
privacy in HIV/PCT service.
|
0.9644
|
7.5131
|
0.13
|
0.8979
|
2.6(0,6516187)
|
|
(X'13) Readiness to know and accept
HIV PCT Results (Yes)
|
28.3658
|
3.605
|
7.9
|
<0.001
|
>162755
(14423,>162755)
|
|
(X'14) Suggestion that HIV PCT service should be
provided free of charge (yes)
|
-0.8604
|
4.2528
|
-0.2
|
0.8397
|
0.4(0.0001,1763.26)
|
|
*Z-test, p-value<0.05, ** See ANNEX 5 to view variables
used in scoring scales.
|
|
Logit Model: Ln[p2/(1-
p2)]= -39.715-0.0296X'1+
1.2901X'2-1.1279X'3 + 1.2919X'4
+0.9243X'5 -1.2049X'6
-0.3604X'7 -1.5237X'8 +
0.1913X'9 +0.7263X'10-3.1371X'11
+0.9644X'12 +28.3658X'13
-0.8604X14
|
|
Source: Field survey, Kintampo, June 2005.
|
Other no significant associations are as follows:
1. Willingness to undergo HIV PCT was negatively associated
with age, post-primary educational level, being student, having ever had
premarital sex, perceiving the need of HIV PCT services and suggestion that HIV
PCT should be provided free of charge.
2. Willingness to undergo HIV PCT was slightly positively
associated with Akan & Mo Ethnic groups, urban residence, Christian
religion, female sex, score (level) of knowledge, and score (level) of
perception towards HIV PCT and suggestion of confidentiality in PCT
services.
4.10. DEDUCTION OF PROBABILITY FOR RESPONDENTS TO
PERCEIVE THE NEED OF HIV PCT SERVICE AND TO INTEND UNDERGOING HIV
PCT
|
Table 11: Distribution of respondents according to
their probability of perceiving the need of HIV PCT service and of willingness
to undergo HIV PCT
|
|
Probability for willingness to undergo HIV PCT
|
|
|
0-0.5
|
>0.75
|
TOTAL
|
|
Probability for perceiving the need of HIV PCT service
|
0-0.5
|
1(0.67%)
|
5(3.33%)
|
6(4.00%)
|
|
0.6-0.75
|
2(1.33%)
|
10 (6.67%)
|
12 (8.00%)
|
|
> 0.75
|
3 (2.00%)
|
129 (86.00%)
|
132 (88.00%)
|
|
TOTAL
|
6(4.00%)
|
144(96.00%)
|
150 (100.00%)
|
|
Source: Field survey, Kintampo, June 2005.
|
Using the two logit models described in Tables 9 and 10, we
deduced the probability for each respondent to perceive the need of HIV PCT
service and the probability of willingness to undergo HIV PCT. Table 11 above
shows that 86% of respondents had a higher probability
(>0.75%) of perceiving the need of HIV PCT service (Mean probability:
0.923786) and of willingness to undergo HIV PCT (mean probability:
0.946193992).
4.11. PREFERENCE TO UNDERGO HIV VCT FOR MARITAL REASON
OR NOT
|
Table 12. Distribution of respondents by sex and HIV
testing choices
|
|
PREFERENCE
|
|
Sex
|
HIV PCT
(%)
|
VCT outside
Marriage context (%)
|
TOTAL
|
|
Female Female Female
|
58 (80)
|
15 (20)
|
73 (100.0)
|
|
Male
|
57 (74)
|
20 (26.0)
|
77 (100.0)
|
|
TOTAL
|
61 (77)
|
35 (23)
|
150 (100.0)
|
|
X2(Yates)=0.35, p-value 0.55, CL 95%, OR=1.36
|
|
Source: Field survey, Kintampo, June 2005.
|
Table 12 illustrates that majority of respondents
(77%) preferred undergoing HIV PCT while minority of them
(23%) preferred voluntary HIV testing outside marriage context. Table 12 does
not show any significant difference of preference choices given the sex of
respondents (p-value 0.55), the Odd ratio of preference of HIV PCT in females
being 1.36 times the odd in males.
4.12. BARRIERS TO HIV PCT ACCEPTANCE AND
IMPLEMENTATION
IN KINTAMPO
DISTRICT
Respondents were asked about what they think were the barriers
to HIV PCT acceptance and implementation in Kintampo District. A long list of
barriers was generated as shown in Table 13 below.
|
Table 13: Respondents' perception of barriers to HIV PCT
acceptance and implementation
|
|
No
|
Perceived Barriers to HIV PCT
|
Yes
(%)
|
No
(%)
|
NK
(%)
|
|
1
|
Inexistence of regulatory procedures and Law/Policy on PCT in
Ghana
|
90
(60.00)
|
59
(39.30)
|
1 (0.7)
|
|
2
|
Mandatory imposition of PCT that infringes the Human Right of
individuals
|
86
(57.3)
|
63
(42.00)
|
1
(0.7)
|
|
3
|
High cost (price) of premarital examinations
|
110
(73.3)
|
40
(26.7)
|
-
|
|
4
|
The location of the centre/hospital at long distances
|
94 (62.7)
|
56
(37.3)
|
-
|
|
5
|
The attitude of the service provider
|
116 (77.3)
|
34 (22.7)
|
-
|
|
6
|
Premarital sex and fear to know one's HIV status
|
110 (73.3)
|
40
(26.7)
|
-
|
|
No
|
Perceived Barriers to HIV PCT
(Continued)
|
Yes
(%)
|
No
(%)
|
NK
(%)
|
|
7
|
Fear of stigma and discrimination in marriage (denial of
marriage for HIV+)
|
116 (77.3)
|
33 (22.0)
|
1 (0.7)
|
|
8
|
Ignorance of the importance of PCT (illiteracy...)
|
111 (74.0)
|
39
(26.0)
|
-
|
|
9
|
Reluctance of fiancés
|
98 (65.3)
|
50 (33.3)
|
2 (1.3)
|
|
10
|
Preference of young people to get married without PCT
|
88 (58.7)
|
61 (40.7)
|
1 (0.7)
|
|
11
|
Opposition of some churches
|
71 (47.7)
|
78 (52.3)
|
-
|
|
12
|
Opposition of some parents
|
72 (48.0)
|
77 (51.3)
|
1 (0.7)
|
|
13
|
Polygyny (Polygynous/polygamous marriages)
& Islamic religion
|
78 (52%)
|
72 (48.0)
|
-
|
|
14
|
Marriage by convenience (outside churches & civil
registrar officer our court or without customary ritual)
|
94 (62.7)
|
55 (36.7)
|
1
(0.7)
|
|
15
|
Forced marriage (e.g. traditional early marriage)
|
93 (62.4)
|
56 (37.6)
|
-
|
|
16
|
Unregistered marriage
|
81 (54.0)
|
60 (46.0)
|
-
|
|
17
|
Inadequate VCT/PCT facilities
|
109 (72.7)
|
41 (27.3)
|
-
|
|
18
|
Lack or inadequate trained personnel & counselors
|
107 (71.3)
|
43 (28.7)
|
-
|
|
19
|
Fiancés are in a hurry to get married very quickly for
any reason
|
91 (60.7)
|
58 (38.7)
|
1 (0.7)
|
|
20
|
Lack of confidentiality and privacy among health care
providers in PCT services.
|
109 (72.7)
|
41 (27.3)
|
-
|
|
21
|
Medical premarital certificate provided to fiancé(e) by
doctors without performing any medical check-ups (fraud)
|
97 (64.7)
|
53 (35.3)
|
-
|
|
22
|
Re-marriage ( for divorced or widowed)
|
84 (56.0)
|
66(44.0)
|
-
|
|
23
|
Inability for girls to negotiate for HIV PCT when boys don't
like it
|
100 (67.1)
|
49 (32.9)
|
-
|
|
24
|
Little solution for those who test HIV (+) ( no effective
drugs to treat AIDS)
|
106 (70.7)
|
44 (29.3)
|
-
|
|
25
|
Blind love among young people
|
85 (56.7)
|
64 (42.7)
|
1 (0.7)
|
|
26
|
Others (not providing gifts to couples, ...)
|
26 (17.4)
|
111 (74.5)
|
12 (8.1)
|
|
NK=Not known (Don't know)
Source: Field survey, Kintampo, June 2005.
|
For easier interpretation perceived barriers described in
Table 13 could be grouped under 4 categories:
1. Major absolute barriers: the proportion of respondents who
said yes is =70%.
These are barriers number 3, 5, 6, 7, 8, 17, 18, 20 and 24.
2. Moderate barriers: the proportion of respondents who said
yes is between 50-69%.
These are barriers number 1, 2, 4, 9, 10, 13, 14, 15, 16, 19,
21, 22, 23 and 25.
3. Minor barriers: the proportion of respondents who said yes
is between 30-49 %. These are barriers number 11and 12
4. Negligible barriers: the proportion of respondents who said
yes is < 30%.
Barriers grouped under «others» in index number 26
fit to this category.
Some of these barriers were also recognized in qualitative
study as it can be related in the following quotes.
|
«Since there is no official law on premarital
examinations here in Ghana which would enable people to test before marriage,
many people marry without testing and thus become victims of many diseases such
as HIV/AIDS which, yet, could have been prevented.»
(IDI: District AIDS Initiative
coordinator/DA/GES/Kintampo, Picture No 9).
|
|
|
«We know that premarital counseling and testing is
part of reproductive health. But we haven't started a special service on it
yet. But things are in the pipe so that a VCT and premarital counseling service
would be implemented in the District»
(IDI :Public Health Nurse and Responsible of Family Health
Clinic/Kintampo)
|
|
«Many young adults have had premarital sex and
because of that they fear to go for the HIV PCT»
(A 4- year-old mother: FGD of Traditionalist
mothers/AMPOMA)
|
|
«Some girls have stayed long without getting men to
marry and when a man promises to marry such girl, she may want the marriage to
happen in no time because she thinks the man may see an other woman and change
the decision, or the test result may compromise the marriage. So in her plan
marriage without any ado with no ceremonial medical examinations is just the
best to satisfy her over due dreams. I am among this group. Just understand
this. Isn't it?»(A 23-year-old girl: FGD Moslem Girls)
|
|
«Broadcasting of the HIV test results in hospitals
and in the public is a major obstacle to HIV PCT. If you want it to work, bring
us counselors who are not known locally or may be people can go and test far in
other new places from their home towns. I don't talk about stigma and
discrimination which are also there.»
(A 39-year-old man: FGD Moslem fathers).
|
Since during FGD of Moslem girls participants also recognized
their religion as a barrier to HIV PCT implementation we found better to
stratify frequencies of this barrier over religion background.
Table 14 below shows that 43.9 % of Moslem
respondents also mentioned Islam as a barrier to HIV PCT. Though statistically
insignificant, there is some level of association between religion and
perception of Islam as a barrier to HIV PCT (p-value = 0.08), meaning Moslem
and non Moslem respondents perceive in the same way that Islam is a barrier to
HIV PCT.
|
Table 14: Distribution of respondents by religion and
perception of
Islam as a barrier to HIV PCT
implementation
|
|
Perceive Islam as a barrier to HIV PCT
|
|
|
Religion
|
Yes (%)
|
No (%)
|
TOTAL (%)
|
|
Catholic
|
15 (41.7)
|
21 (58.3)
|
36 (100.0)
|
|
Protestant
|
23 (63.9)
|
13 (36.1)
|
36 (100.0)
|
|
Pentecostal
|
19 (70.4)
|
8 (29.6)
|
27 (100.0)
|
|
Muslim
|
18 (43.9)
|
23 (56.1)
|
41 (100.0)
|
|
No Religion
|
5 (50.0)
|
5 (50.0)
|
10 (100.0)
|
|
TOTAL
|
80 (53.3)
|
70 (46.7)
|
150 (100.0)
|
|
X2: 8.2, p-value:0.08, CL 95%
|
|
Source: Field survey, Kintampo, June 2005.
|
4.13. KEY ISSUES FROM RESPONDENTS TOWARDS HIV PCT
HEALTH
PRACTICE IN KINTAMPO
DISTRICT
4.3.2. 4.13.1. VIEWS ON FREQUENCY OF HIV
TEST BEFORE MARRIAGE
AMONG WOULD-BE
COUPLES
Figure 8 below shows that a third of respondents in both sexes
suggested the HIV test should be done at least twice before marriage, with 3-6
months interval between two tests. Almost one fifth of respondents in both
sexes suggested HIV test should be done just once 2-3 months before marriage.
Another fifth suggested it should be done at least once, without specifying the
maximum number of tests. Few respondents also thought the frequency of HIV
tests should vary depending on the length of the engagement/marriage period.
We have to also note that almost one fifth of respondents did
not know (NK) any answer at all, possibly because of lack of knowledge.

The same trend of answers was also shown in qualitative
study.
|
«HIV Test should be done 3 times before
marriage, with 3 months interval between two tests, given the window
period»(IDI: Counselor & Matron /Kintampo District
Hospital)
|
|
«It is better they undergo a minimum of 3 tests, the
first one is preliminary, the second is the control test and then the third one
is a confirmation test, with 3 months interval between 2 tests. I haven't
received a couple who did more than one test, but we advise them about the
necessity of doing 3 tests before marriage.»
(IDI: Lab Technician/ Kintampo District Hospital, Picture
No 10)
|
|
|
«It should be More than once because supposing you
get it now, if you test now it may be negative while it may convert to
positivity 3 months later due to the window period. That is even why we start
our counseling sessions earlier at least 3 months prior to marriage so that
couples who are willing to do HIV testing can do it at least twice before
getting married»
(IDI: Rev Pastor Methodist Church/Kintampo)
|
4.13.2. VIEWS OF RESPONDENTS ON WHO SHOULD SEND
WOULD-BE
COUPLES AT THE HOSPITAL FOR
HIV PCT
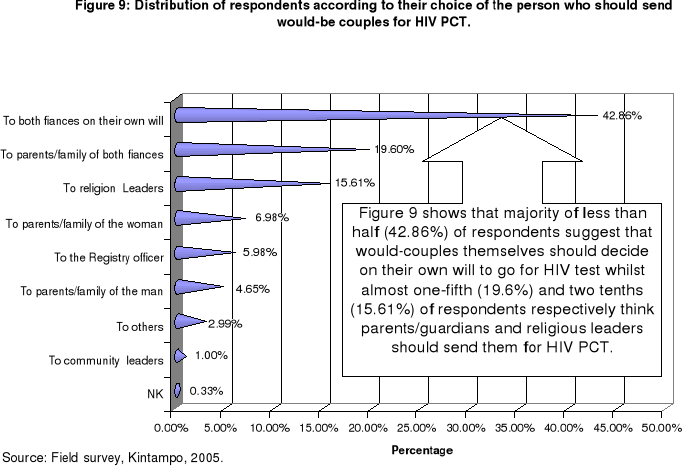
4.3.3. 4.13.3. VIEWS OF RESPONDENTS ON
WHO THE HIV TEST RESULT SHOULD
BE COMMUNICATED TO
AFTER A PCT SESSION
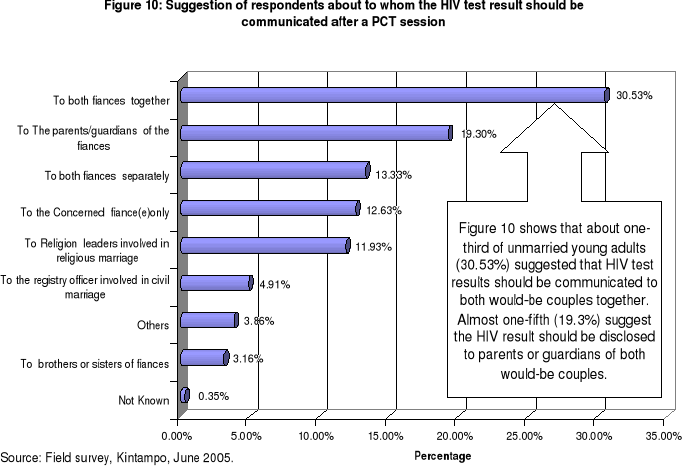
4.13.4. WAYS TO PROMOTE HIV PCT IN K'PO
DISTRICT
From Table 15 below the totality of respondents (100%)
recommended that other required premarital tests should be added to HIV test in
order to reduce stigma associated to HIV/AIDS, especially when HIV test is done
solely.
|
Table 15: Suggestions from respondents on ways to
promote HIV PCT in Kintampo District
|
|
N0
|
Ways and means suggested by respondents
|
Yes
(%)
|
No
(%)
|
NK
(%)
|
|
1
|
There should be a specific law (decree-law) on premarital
examinations in Ghana
|
135
(90.6)
|
14
(9.4)
|
-
|
|
2
|
PCT should be clearly mentioned in the health reproductive
policies of Ghana
|
145
(96.7)
|
5
(3.3)
|
-
|
|
3
|
Mass sensitization campaigns about PCT through durbars,
Radio/TV, news papers, churches/mosques, NGO, asso- ciations, clubs, schools
& university, Hotels, hospitals etc
|
149
(99.3)
|
1
(0.7)
|
-
|
|
4
|
Open discussions on Youth sexual education about HIV-AIDS and
PCT in youth durbars such as sports...
|
149
(99.3)
|
1
(0.7)
|
-
|
|
5
|
PCT should be taught in the health education &
reproduction matters in school
|
146
(97.3)
|
4
(2.7)
|
-
|
|
6
|
Churches and mosques should teach PCT to young couple before
marriage
|
149
(99.3)
|
1
(0.7)
|
-
|
|
7
|
Strictly prohibit all marriage (be it civil, religious or
traditional) before PCT, through a decree law
|
118
(79.2)
|
31
(20.8)
|
-
|
|
8
|
Strictly recommend a prenuptial medical certificate from the
doctor for each fiancé before celebration of marriage
|
140
(93.3)
|
9
(6.0)
|
1
(0.7)
|
|
9
|
Providing care and support services for people living with
HIV/AIDS
|
144
(96.0)
|
6
(4.0)
|
-
|
|
10
|
Reducing stigma and discrimination against people living with
HIV/AIDS
|
136
(90.7)
|
14
(9.3)
|
-
|
|
11
|
Creating youth HIV associations/clubs like Virgin club etc
|
139
(92.7)
|
11
(7.3)
|
-
|
|
12
|
Add other premarital required tests to reduce stigma
associated to HIV
|
150
(100)
|
-
|
-
|
|
13
|
Encouragement by providing free treatment for any other
diseases detected among those would-be couples who come for HIV PCT.
|
145
(97.3)
|
4
(2.7)
|
-
|
|
14
|
Others (PCT before pride price is paid, quoting that couple
did PCT during marriage ceremony, PCT film/posters....)
|
49
(32.9)
|
90
(60.4)
|
10
(6.7)
|
|
Source: Field survey, Kintampo, June 2005.
|
These findings correspond to opinions of participants in FGD
and IDI.
|
«Even when premarital examinations are
carried out, the emphasis is only on HIV/AIDS and one forgets about many other
diseases requiring genetic counseling, and family planning is not part of it.
There should be a policy that defines the package of required premarital tests.
The policy should insist that no marriages should take place unless couples
undertake an examination, and it should also include counseling on family
planning. Such policy will definitely promote HIV PCT in Kintampo and in the
whole nation.» (IDI: Public Health Nurse & In charge of Family Health
Clinic /Kintampo).
|
4.13.5. WAYS TO CREATE EASIER ACCESSIBILITY TO HIV
PCT
IN KINTAMPO
DISTRICT

Findings in Figure 11 shows that majority of respondents
(59.88%) suggested that HIV PCT services should be free or set at affordable
cost or paid by the government or any charity NGO in order to make HIV PCT
services accessible to young people. One fifth of respondents also suggested
that the number of health facilities providing HIV PCT services should be
increased, one tenth saying VCT/PCT centres should be put within the community
not at long distances.
These suggestions also meet the opinion of participants in FGD
and IDI.
|
«Past experience has shown many people would
voluntarily undergo HIV test if it is free. In fact in 2004, Ghana Social
Marketing Foundation came in Kintampo to recruit 100 people for free VCT. It
was a 7-day-casual VCT session based at Motor Union/G.P.R.T.U-Kintampo. Within
7 days they were able to get about 96 persons of whom 6 tested HIV positive.
Therefore I believe young people will patronize HIV premarital testing if it is
made free».
IDI: District HIV/AIDS response Initiative
coordinator/DA-GES/Kintampo.
|
Some of the participants even linked the accessibility to HIV
PCT to the District Mutual Health Insurance Scheme (DMHIS):
|
«Some one may want to do HIV PCT but doesn't
get money for it. So everybody should register for DMHIS to have easier access
to HIV PCT. HIV PCT should be announced to the public as part of services to be
covered by the DMHIS».
(IDI: Rev. Pastor,Ampoma Village)
|
4.13.6. WAYS TO MAKE HIV PCT MORE EFFECTIVE,
ACCEPTABLE AND
ATTRACTIVE FOR YOUNG PEOPLE IN
KINTAMPO DISTRICT
Table 16 below regroups all measures that respondents
suggested for the HIV PCT to be more acceptable and attractive to them. Some of
these measures were suggested by the large majority of respondents (e.g.
Guarantee complete confidentiality and privacy ) etc. The suggestions implied
certain interventions to be put in place so that people are attracted by the
service (see Discussion, point 4.7.6 and Figure 15).
|
Table 16 : Suggestions for the HIV PCT practice to be more
effective, acceptable and attractive to unmarried young people in Kintampo
district
|
|
N°
|
Ways to make HIV PCT more effective
|
Yes (%)
|
No
(%)
|
NK
(%)
|
|
1
|
Provide for unbiased, clear and non-judgmental advices to
would-be couples
|
139
(92.7)
|
10
(6.7)
|
1
(0.7)
|
|
2
|
Guarantee complete confidentiality and privacy
|
149
(99.9)
|
1
(0.7)
|
-
|
|
3
|
Secure permission of patients before passing on information to
anybody (parents, pastors/bishop, Imam and other care providers..)
|
142
(94.7)
|
8
(5.3)
|
-
|
|
4
|
Provide permanent caring and support services
|
147
(98.0)
|
3
(2.00)
|
-
|
|
5
|
Examiner/counselor of the same sex as the client
|
127
(84.7)
|
22
(14.7)
|
1
(0.7)
|
|
6
|
To be counseled by knowledgeable, well trained, kind, wise and
good communicator examiner/counselors
|
145
(96.7)
|
5
(3.3)
|
-
|
|
7
|
To be counseled by counselors not known in the area and change
continuously the old counselors by new ones after a certain period.
|
135
(90)
|
14
(9.3)
|
1
(0.7)
|
|
8
|
Follow up of fiancés / newly married is done after HIV
PCT
|
132
(88.6)
|
15
(10.1)
|
2
(1.3)
|
|
N°
|
Ways to make HIV PCT more effective
(Continued)
|
Yes (%)
|
No
(%)
|
NK
(%)
|
|
9
|
Provide for the presentation of test results as soon as
possible, to reduce the anxiety of waiting to long (same day result)
|
141
(94.0)
|
7
(4.7)
|
2
(1.3)
|
|
10
|
Affordable cost or free HIV PCT examinations
|
147
(98)
|
3
(2.0)
|
-
|
|
11
|
To be counseled by young adults counselors
|
99
(66.0)
|
51
(34.0)
|
-
|
|
12
|
More than one counseling session is provided to the
fiancés
|
126
(84.0)
|
23
(15.3)
|
1
(0.7)
|
|
13
|
When there will be a treatment or effective cure for
HIV/AIDS
|
140
(94.0)
|
9
(6.0)
|
-
|
|
14
|
Provide entertainment in VCT/PCT centres
|
136
(90.7)
|
14
(9.3)
|
-
|
|
15
|
Others (give marriage gifts to would-be couples who come for
HIV PCT, quote it in marriage ceremony...)
|
42
(28.0)
|
108
(72.0)
|
-
|
|
Source: Field survey, Kintampo, June 2005.
|
4.13.7. HEALTH FACILITIES WHERE HIV PCT CENTRE SHOULD
BE ESTABLISHED IN KINTAMPO
DISTRICT
|
Table 17: Health facilities where respondents suggest
HIV PCT services to be established
|
|
|
Health Facilities
|
|
Sub-District
|
K'po District Hospital (%)
|
Jema Health centre
(%)
|
Anyima Health centre
(%)
|
New Longoro H.Centre
(%)
|
Busuama Health centre
(%)
|
In any one of fac.in the Dist. (%)
|
In all the H.
Facilities
(%)
|
TOTAL
|
|
Kintampo
|
76 (93.8)
|
0 (0)
|
1(1.2)
|
0 (0)
|
0 (0)
|
1 (1.2)
|
3 (3.7)
|
81 (100)
|
|
Jema
|
10 (24.4)
|
31 (75.6)
|
0 (0)
|
0 (0)
|
0 (0)
|
0 (0)
|
0 (0)
|
41 (100)
|
|
New Longoro
|
22 (78.6)
|
0 (0)
|
0 (0)
|
2 (7.1)
|
1(3.6)
|
0 (0)
|
3 (10.7)
|
28 (100)
|
|
TOTAL
|
108 (72)
|
31 (20.7)
|
1 (0.7)
|
2 (1.3)
|
1 (0.7)
|
1 (0.7)
|
6 (4)
|
150 (100)
|
|
Source: Field Survey, Kintampo, June 2005.
|
Table 17 shows that majority (72%) of respondents suggested
HIV PCT services should be established in Kintampo District Hospital (KDH).
Also it is noted that majority of respondents from Jema Sub-district (75.6%)
chose Jema health centre for the HIV/PCT service to be implemented. Majority of
respondents from New Longoro Sub-District quoted KDH rather than their health
centre as the site for the HIV PCT centre.
4.14. POSSIBLE DECISIONS THAT WOULD-BE COUPLES ARE
MORE LIKELY
TO MAKE GIVEN DIFFERENT SCENARIOS OF HIV
TEST RESULTS.
Respondents were asked to give their likely decisions on
marriage given assumptions of possible HIV tests results in different
scenarios.
Figure 12 below shows that majority of respondents (94.7%)
would definitely decide to break the marriage relationship and choose another
healthy partner in case their fiancé(e)s test HIV positive after a PCT
session. The break up of marriage relationship would also be decided by the
majority of respondents (90.0%) who themselves test HIV positive while their
would-be partners are HIV negative.
|
|
Source: Field survey, Kintampo, June 2005
|
|
Decision 1: Marry but abandon childbearing (permanent
contraception) + protected sex
(condom) throughout the life
Decision 2: Marry but abandon childbearing (permanent
contraception), adopt children +
protected sex (condom) throughout the
life
Decision 3: Marry but limit childbearing with PMTCT of HIV
throughout the life for all
Pregnancies and breastfeeding.
Decision 4: Break up of engagement/marriage relationship and
search/choice of an other
healthy fiancé(e)
Decision 5: None of them, I will still marry her/him , have
unprotected sex and bear
children irrespective of all advices,
because I love her/him and marriage is
for the best and the worst.
Others : Others undefined decision.
NEG vs. POS: The respondent is negative whereas the
fiancé(e) tests HIV positive.
POS vs. NEG: The respondent tests positive whereas his/her
fiancé(e) is HIV negative
POS vs. POS: Both fiancé(s) test HIV Positive.
|
However in the third scenarios of both fiancé(s) being
HIV positive, opinions diverged greatly: one third (34.7%) chose decision 1,
followed by one fourth choosing decision 5 (23.3%), and one fifth (16%)
choosing decision 3. This trend meets views of participants in both IDI and
FGD.
4.15. POINTS OF VIEW OF RESPONDENTS ABOUT MARRIAGE
BETWEEN
DISCORDANTS COUPLES AND HIV INFECTED
COUPLES
Figure 13 below shows that majority of
respondent (64%) opted that marriage between discordant couples should not be
permitted versus a fifth (19.3%) saying such marriage should be permitted only
under certain protective precautionary measures such as permanent condom use,
limitation of childbearing, PMTCT etc.Their views greatly diverged about
marriage between both infected partners, majority of less than half (44.7%)
saying it should be permitted under certain protective measures and another
considerable proportion (41.3%) saying such marriage could be permitted
provided would-be couples and or their parents/families agree with it.
In either case it should be noted that only few respondents
(0-2.7%) put consideration on the agreement by the religion bodies for such
marriage to be conducted.
|
|
Source: Field survey, Kintampo, June 2005
|
|
Pv1: Such marriage should be permitted only under certain
protective precautions given to the couple by the doctors.
Pv2: Such marriage should not be permitted.
Pv3: No matter if the two fiancé(s) agree to marry
Pv4: No matter if the religious leaders agree with the
marriage.
Pv5: No matter if the parents/families of both
fiancé(s) agree with the marriage. NK: Don't Know.
|
The entire trend here above meets the opinions observed among
participants in FGDs and IDI.
|
«Would-be couples who are both HIV positive
should marry so that they wouldn't transmit it outside to others. But in
couples where only one tests positive, marriage should be canceled because it
is impossible for them to use condom throughout their life if they
marry».(A 38-year-old mother: FGD of Moslem mothers)
|
|
« No marriage when one tests HIV positive.
But for infected couples, they can console themselves to still marry, hoping
may be one day doctors will find vaccine or a drug for them to get treated
while still living and enjoy the little they could enjoy. After all they are
human being with the equal right of enjoyment».
(A 39-year-old men: FGD of Moslem
Father).
|
|
«.... Uuummmh, well!. In marriage matter
normally the last decision belongs to the couples. When although the fact that
one of them is HIV sero positive, the other partner still say he/she will still
marry him/her, that marriage could be celebrated. It is not my responsibility
to deny the right of people to marriage.....But I would really hesitate to
marry them...Pastor laughing...., knowing I am contributing to let AIDS protect
them soon in their grave." «IDI: Rev Pastor Methodist
church/Kintampo»
|
|
«Both discordant couples and infected ones
should not marry. It is not a matter of just blessing their union. What about
their future? Who will take care of their orphans and widows/widowers?
Counselors could counsel them to get rid of marriage so that they live longer.
I am sorry, It is not stigmatization; just understand the situation which will
change only when the vaccine or drug of HIV will be
found.»
(A 23- year-old boy and KHRC field worker: FGD
unmarried boys/girls of mix religious background).
|
|
«Normally both discordant couples and
infected couples shouldn't be allowed to marry, given the fact that they would
not be able to cope with all the precautions required. Such marriages favor
birth of infected children, most of who would become orphans or also transmit
it to others. We have to stop people with blind love to destroy new generations
with innocently HIV infected children.»(IDI: Counselor/KDH, Picture No
11)
|
|
Chapter Five
DISCUSSIONS
Since demographic characteristics of respondents show a very
heterogeneous and representative picture of the main social groups living in
the District, we believe findings in this study are quite representative of the
district. We can therefore surely discuss them.
5.1. PREMARITAL SEX HISTORY AND HIV-AIDS RISK FACTORS
AMONG
SURVEYED
RESPONDENTS
Results from Table 3 showed that 66% of respondents have had
premarital sex, with the mean age at first sex of 18 years (18.125 for females
and 18.075 for males). Female were significantly 2.97 times more engaged in
premarital sex than males (p=0.004116). These findings show a
higher level of premarital sex as compared to those found in the 2003 GDHS
where it was found that by age 18, almost half of women (48%) and one-fourth of
men (25%) have had sexual intercourse53. Findings from this study
showing that men slightly engage early in sexual intercourse are in
contradiction with the same 2003 GDHS where it was seen that it was rather
women who early engage in sex (median age at 18.2 years) than men (median age
at 20.2 years)53. The vulnerability of women to premarital sex may
be likely due to gender differences which are culturally favored. These
cultural deviations which include coercive sex, rape, defilement etc, promote
the transmission of HIV/AIDS and endanger the lives of women through
involvement in unprotected sex with multiples partners59.
Our findings are similar to those found in China where most
newly weds in China have had sex before they marry.59
Given the fact that premarital sex was also mentioned as a
core barrier to HIV PCT from participants in IDI and FGDs, since those who have
had sex tend to fear to go for test because they fear they might have been HIV
infected, we think reduction of premarital sex among young unmarried adults
would help to promote HIV PCT in the area. A certain number of measures, such
as sex education, school-based educational programs, adolescent counseling,
creation of virgin clubs, parents implication in sex education, reduction of
poverty and illiteracy, interdiction of projections of pornographic
film...among others, could help, as it has proved success
Worldwide9,39,59,60,61.
5.2. KNOWLEDGE AND PERCEPTION OF RESPONDENTS TOWARDS
HIV PCT
Findings in Tables 4 ,5, 6 and 7 and in Figures 5,6 and 7
support that 97% of respondents had good knowledge with 100% scoring positive
perception towards HIV PCT, with little variation of knowledge and perception
among both men and women. This is an encouraging picture on which District
Health Authorities can rely to quickly implement a HIV PCT service in order to
respond to their need. Since score of knowledge showed lower scores among 3% of
respondents, education on HIV PCT should still be scaled-up continuously so
that all unmarried young adults and growing adolescents in the District all
acquire adequate knowledge on HIV PCT.
5.2.1. INDICATORS ON AWARENESS AND KNOWLEDGE ON HIV
PCT
Although majority of respondents scored higher marks showing
adequate knowledge on HIV PCT and confirming near universal awareness on
HIV/AIDS revealed in the 2003 GDHS 29,53, lack of knowledge emerged
from each of the indicators in Table 4 in both sexes. In fact none of the
indicators performed 100% of respondents giving right answers. For example it
is noticeable that 10.3% did not know that children could be born HIV infected
from their mothers, figure which is quite similar to data from the 2003
GDHS53. Worse still, 38.7 % did not know that not all sexual unions
and marriages are safe and good for health of both partners and offspring. And
as a divergence, although showing big lack of knowledge in knowing diseases
making unsafe sexual unions and marriages, almost 95% of respondents recognized
they would consider health status as a core criteria when they will choose
their marriage partners. All these show there is a deplorable big gap since
such basic knowledge is actually the one which would help them perceive well
the importance of HIV PCT.
Beside that, 82.7% said they would assess health status of
their marriage partner through premarital examinations. This specific
observation of high level of knowledge concerning the necessity of assessing
good health status of their marriage partners and the ways to assess it,
explains very well the near universal positive perception they showed towards
HIV PCT (Table 6, 7 and figure 7).
It should be noted that majority of respondents (58%) showed
big lack of knowledge about knowing a young adult who suffers or suffered from
or died of HIV/AIDS, trend which is similar to figures from the 2003
GDHS53. Also majority (63%) did not know anyone or any couple who
underwent HIV PCT before marriage. The first observation does not imply young
adults are not having HIV/AIDS or dying from it, when we know that in Ghana
more than 90% of AIDS cases are found among adults aged 15-49%, the peak ages
being 25-34 for females and 30-39 for males.29 This fact rather
shows that education and awareness creation on HIV/AIDS is still lacking in
some social groups. In fact many are those dying of HIV/AIDS and yet people
around them don't just know it is AIDS or they think it is just something else.
Promotion of peer education, including persons living with AIDS is crucial to
break up this kind of gap of knowledge on HIV/AIDS ravages.
For the second observation we agree it is possible a
respondent has not known yet someone or a couple who underwent HIV PCT before
marriage. This may be true since HIV PCT is not yet formally implemented in
Kintampo District. The service is still at an embryonic stage where only few
would-be couples go and test. And even then because the HIV PCT is surrounded
by a strict rule of secrecy, it may be even possible a person or couple the
respondent knows did the test before marriage, but that he/she could not just
inform others for confidentiality purposes. But since we know it is by
observing other person doing good things that respondent could also consider
that behavior as being good and finally adopt it him/herself62, we
think at this stage not performing HIV PCT would remain a barrier to promote
the HIV PCT behavior. Also people should not confuse confidentiality on HIV
test results with confidentiality on practicing or attending HIV PCT. The first
can be kept confidential while the second information can be made available to
relatives and to peers. There is still much to do to first implement officially
the HIV PCT centres where would-be couples can go for test and let people
around know that the HIV PCT health practice (behavior) is being undertaken by
others.
Surprisingly, although HIV PCT is a specific type of VCT,
majority of respondents (84.7%) had heard more about HIV PCT than VCT itself
(72%). This shows how education and awareness creation is still low or
inconsistent on VCT and that even when respondents get the information they
only get it partially, inadequately and incompletely. This could be confirmed
by their sources of information about VCT and HIV PCT. Although majority of
respondents heard about HIV PCT through audiovisual media channels (Radio, TV,
Cinema or Video...) [78.5%], churches/Mosques [36.1%] and friends/third person
[33%], it is surprisingly deplorable that only 31.9% heard about it through
health workers who yet should have been the very top source of information if
we only want the right information on HIV PCT to reach young people. Only few
respondents (14%) heard about HIV PCT from their parents, meaning young adults
rely on outside sources as their parents are more likely not to inform and
educate them about HIV PCT and other sexual matters. Also likely it is possible
these young adults get more information on HIV PCT compared with parents. This
opposes and questions the workability of one of the strategies for the
implementation of BCC and IEC programmes of addressing HIV/AIDS in Ghana, where
parents are supposed to be educated to be positive role models for their
children and also to play an active role in educating them about sexuality and
other reproductive health related matters9,61. Mass media seemed to
be playing its role in the implementation of BCC and support towards an
effective HIV PCT awareness, behavioral change, care and coping strategies as
it is recommended in the National HIV/AIDS and STI Policy61. However
the involvement of schools in informing young people about HIV PCT seemed still
very low (29.2%).
It is worthy to note that the inexistence of effective drug to
cure HIV/AIDS was known by majority of respondents (94.7%). This is a good
point since from this we hope they could then deduce that the only available
effective way to fight HIV/AIDS is its prevention which is considered central
to the National effort to reduce the spread of HIV/AIDS in Ghana.61
As a result, knowing HIV/AIDS does not have any effective drug to kill
the HIV would definitely help them understand the importance of HIV premarital
counseling and testing, one of usual preventive measures in the national
framework to fight HIV/AIDS.
With reference to pictures 4 and 5 showing the routine reality
that traditional herbalists in Kintampo District are having people living with
AIDS (PLWAs) who come to them for treatment, it is important to attract your
attention that such false claims of cure for HIV/AIDS negatively affects BCC in
Kintampo. During one FGD one woman said the following quote:
|
«By now, Traditional herbalists are wrongly claiming
that they have effective drug to cure and eradicate HIV/AIDS. One neighbor sex
worker told us she would no longer use condoms in order to earn much money
(...meaning she would rather have raw sex which she taxes high...) since, she
said, she is now convinced there is traditional effective cure for
HIV/AIDS....And if we go far, this may also affect adversely patronization of
VCT and HIV premarital testing when it will start functioning».
(A 28- year- old woman: FGD of Moslem mothers).
|
It is true such claims of cure for HIV/AIDS may affect
negatively compliance and patronization of preventive services such as HIV PCT
in Kintampo. Therefore we suggest that the DHMT assist and orient those
traditional herbalists as it is recommended in the National HIV/AIDS
policy.61
5.2.2. LEVEL OF KNOWLEDGE ON HIV PCT
Using the tri-polar scoring scale described earlier on, we
found out that majority (97%) of respondents proved Good knowledge, with 41.3%
scoring «Adequate Good Knowledge» versus
55.7% scoring «Average Good Knowledge»,
versus a minority (3%) proving Poor knowledge on HIV
PCT. These results clarify one of the factors (poor public
knowledge on HIV PCT) that we mentioned in our conceptual frame work (see
Introduction) and wanted to verify in this study. The findings are sufficiently
encouraging in the sense that, with this higher level of knowledge revealed
contrarily to what we thought initially, they suggest there is a hopeful
starting point from which the District can take off in implementing such
service.
However it should be noted that when analyzing level of
knowledge in different professional groups (Table 5), only traders scored
adequate good knowledge while students and others scored average good
knowledge. This is a surprise since we would normally expect students to know
more than traders and other professional groups. But all the same, wherever
you are or whatever you do, you may get or may not get access to the right
information needed. Just to say that awareness creation on HIV/AIDS prevention
should be scaled-up at all levels to ensure equitable accessibility of people
to information.61
Also although the level of knowledge showed average good
knowledge in all religious groups, Christian respondents scored the highest
mean score ( 15.9[SD=2.9]) than Moslem and respondents with no religion. This
confirms the observation we got in the field through IDI and FGD where it was
shown that Christian religious institutions have started doing some educational
activities on HIV PCT among their churchgoers and even some had started sending
would-be couples for HIV PCT at the KDH, whereas it was not yet the case in
Islam communities. Although not significant, this disparity of level of
knowledge among respondents of different religious groups demonstrates that not
all religion bodies have responded to the government advocacy for an effective
national response to the problem of HIV/AIDS61.
It should also be noted that respondents of Akan ethnic group
were more knowledgeable (adequate good knowledge) than their counterparts from
other ethnic groups who scored average good knowledge. We think this may
suggest that the Akan respondents have high access to HIV PCT information than
others, without being sure from which kind of sources of information. A further
study is needed to deeply research into this to determine the why of this
discrepancy.
In figure 6, we also surprisingly noted that respondents from
rural parts actually knew slightly more about HIV PCT than those coming from
urban area although there was no significant difference. This discrepancy is
difficult to explain although we may just relate it to differences in
accessibility to or in response of attendance to opportunities of information
between the 2 groups. This unexpected finding also tells how seriously people
who live in rural areas take in IEC/BCC messages compared to those in urban
areas.
The higher level of knowledge on HIV PCT among respondents
from Kintampo District may prove somehow how active and effective has been the
comprehensive BCC strategy addressing HIV/AIDS in Ghana and in Kintampo
District to provide information guided by individual needs and
perceptions.30,31,61.
5.2.3. INDICATORS OF PERCEPTION OF RESPONDENTS
TOWARDS HIV
PCT
Indicators of perception of respondents towards HIV PCT showed
encouraging results ranking from 80.7% to 100% (Table 6).
In fact results showed high risk perception to HIV (93.3%)
[far higher than figures reporting low risk perception in Ghana29],
higher perceived severity of HIV/AIDS (100%), higher perceived threat of
contracting HIV in case one marries without attending HIV PCT (98%), higher
perceived benefit of HIV PCT (100%), high perceived self efficacy towards HIV
PCT action (98%), high perception of HIV PCT as a subjective-family norm
(96%), high perception of HIV PCT as a subjective-peer norm (96%), high
perception of HIV PCT as a social norm (98.7%), high perceived barriers to
HIV PCT practice (80.7%) and high perceived need of HIV PCT services (99.3%)
among respondents. These are all conducive factors which may have led most
respondents to be more attracted by HIV PCT practice, looking both at the high
rate of willingness (98%) they manifested to undergo HIV PCT and at the high
readiness rate (96.7%) to know and accept their HIV test results after a PCT
session, contrary to what we initially presumed in the conceptual framework. In
fact it is believed that people will take action to prevent, to screen for, or
to control ill-health conditions 1) if they regard themselves as susceptible
to the condition, 2) if they believe it would have potentially serious
consequences on their health/life, 3) if they believe that a course of action
available to them would be beneficial in reducing either susceptibility to or
the severity of the condition, 4) if they are convinced that most people
(family members, peers..) approve of the action (behavior), and 5) if they
believe that anticipated barriers to (or costs of) taking the action are
outweighed by its benefits62. Therefore the district authorities
should orient the BCC strategies in specifically addressing those indicators so
that HIV PCT is widely promoted in Kintampo district. Thus for behavior change
communication strategies to succeed in fighting HIV/AIDS in new couples in the
district, unmarried young adults must feel threatened by their current
behavioral patterns (perceived susceptibility and severity) and believe that
change of a specific kind of behavior (getting married after attending any PCT)
will result in a valuated outcome (of protecting him/her and his offspring
against HIV risk infection in attending HIV premarital screening) at acceptable
cost. They also must feel themselves competent (self-efficacious) to overcome
perceived barriers to adopt HIV PCT practice (behavior).
Should HIV PCT be made compulsory or optional in
Kintampo District?
As you may have seen it in Table 5, majority of respondents
(61%), recommended HIV PCT should be compulsory as opposed to minority (39%),
saying it should rather be optional. Views of participants in qualitative study
were even much divergent, constituting itself a discussion flow in view of the
following quotes, just to mention a few.
|
«If we truly want to save lives, I think HIV PCT should
be made compulsory, so that transmission of HIV will be reduced. Optional
testing will still favor HIV spread in new couples since not all would-be
couples will opt to go for it.»(IDI: District HIV/AIDS Response Initiative
Coordinator /DA /GES/Kintampo, Picture No 12).
|
|
|
«No! In church matters, we don't make things
compulsory, so HIV PCT should be made optional. The would-be couples have to
decide what they want to do regarding their own life and health. We haven't
reached the level where we ask for a medical certificate that indicates that
you are HIV/AIDS free before celebrating your marriage. Our advice is that we
talk to the would-be couples and each person him/her self has to accept the
advice. If he/she decides to do the HIV test, fine. If not, well, we let them
know that they will have to suffer the consequences.»(IDI: Rev.Pastor
Methodist church/Kintampo)
|
|
«In church we leave to people their freedom to self
acceptance and decision like God does for us. So HIV testing is not compulsory
in our church before marriage. We only counsel would-be couples to do it. The
last decision to test is for them»
(IDI: President of St Joseph Catholic church,
/Kintampo, Picture No 13)
|
|
|
«Since most of young adults may not comply
voluntarily, HIV PCT should be made compulsory. I believe in my Mosque as
people like marriage it can still work very well like that»
(IDI: Imam/Central Mosque/Kintampo, Picture No 14)
|
|
«I think, the simplest better way is to make it
compulsory. We were doing it in our church and it worked. But sometimes ago we
received a letter from an NGO saying we should not continue to do it like that.
But it has become a social normal behavior among my churchgoers. If I were to
make a law, frankly it should be made compulsory»
(IDI: Rev Pastor, Pentecost's church/Kintampo)
|
|
«Yes. It should be compulsory in order to reduce the
spread of HIV in new couples and families. This will bring happiness in the
country»
(IDI: Traditional Herbalist/Ampoma )
|
|
«I am just not comfortable for HIV PCT to be
compulsory. It should be optional rather. Eeeh!, I can't really explain why.
Just make it optional. It is a stressful deal.»
(IDI: Private Medical Doctor/Kintampo)
|
|
«HIV PCT should be made compulsory. Because the rate
at which HIV/AIDS is going high and higher in this place is terrible. Very soon
within decades each family in Kintampo will have a HIV infected person or a HIV
orphans/widows. So since couples don't come voluntarily, just scarce cases, it
has to be compulsory.
(IDI: Matron Counselor/KDH, Picture No 15)
|
|
|
«Neither compulsory nor optional. Both are not good.
If you make it compulsory, fine, but people will feel infringed in their right.
If you make it optional, also fine. But some people will not do the test and
the disease will still spread and decimate people. We should rather educate and
encourage people so that HIV PCT becomes an individual, ,familial , social and
routine norm of life so that we do It just spontaneously like we eat or put our
dresses»
(IDI: Laboratory Technician/KDH)
|
|
«It should be compulsory. Parents should make sure
that PCT is done before they give their children for marriage»
(A 34- year- old mother: FGD Traditionalist
mothers/Ampoma)
|
|
«It should be compulsory because nobody likes the
illness»
(A 45-year- old father: FGD Moslem fathers)
|
|
«Yes! It has to be compulsory. In our church it is
organized by the marriage committee»
(A 64- year- old father: FGD Christian parents).
|
|
«It should be made compulsory. If not many people
will not test. If you can accept to marry an HIV infected partner, fine, then
it can be optional. But if you know you could regret it later, the best
solution is to make it compulsory, what else? »
(A 23-year- old single girl: FGD Moslem girls, Picture No
16)
|
|
|
«It should be compulsory. But even so, people will
still don't go for test, unless the government sets a strong conducive law on
premarital tests, which will first force people to do It before realizing later
it has become part of personal and social spontaneity.»
(A 24-year- old single boy: FGD young adults, Picture No
17).
|
Can we still discuss this issue after this discussion flow? If
you look at it critically, what is obvious is that although views diverged,
majority if not all respondents and participants are saying it should be
compulsory. But what would the policy maker choose? If you are still free of
HIV/AIDS, what is the option which secures you the best? If you are a PLWA,
which option fits the best? And if you are PLWA children innocent victims from
mother-to-child transmission of HIV, what would have been the option to protect
you? And if you are a lawyer or a medical doctor or a religion leader, what is
the best solution? If you are demographer planning for a future bright
generation what is the best solution? We could still lengthen the list of
similar questions, just to show that the view of each person depends on his/her
own interest. The legislator should put all views together in order to make a
holistic representative and acceptable policy that protect each individual and
the community.
This issue on compulsoriness of HIV PCT always creates polemic
among people. This is the case even among WHO/UNAIDS staffs 63. But
from public health point of view, disease screening is one of the most basic
tools of modern public health and preventive medicine.64
Although screening programs are commonly thought of as either
voluntary (optional) or mandatory, there is in fact a continuum of approaches
that can be taken. Faden and colleagues (1991) characterize five types of
screening programs under which HIV PCT could fall: (1) completely mandatory,
(2) conditionally mandatory, (3) routine without notification, (4) routine with
notification, and (5) non-directive patient choice.64
In a completely mandatory program, a government
agency requires citizens to undergo a screening test and sanctions those who do
not comply. So for instance in our case study, individuals who would marry
without performing the test or pastors, bishops or Imam who would celebrate a
marriage when a couple did not perform any test would be sanctioned.
64
In a conditionally mandatory program, either
government or a private institution makes access to a designated service or
opportunity contingent upon participation in the screening
program64. For instance, medical authorities-legislators-lawyers and
religion leaders could require would-be couples to undergo HIV PCT as a
condition of receiving prenuptial certificate that would allow them to marry.
And this is actually what we meant in asking the question whether HIV PCT
should be compulsory or not and we believe majority of respondents who opted
for the compulsoriness understood this.
In a non-directive patient choice program (voluntary
testing) individuals are provided information about the test, and the choice
about whether to be tested is left to them. Patients actively must choose to be
tested, and if they do not opt to be tested, the default is that no testing
will occur. This type of program is the model typically employed in the context
of genetic counseling where it is labeled "non-directive counseling." This also
is the model used by HIV anonymous test sites, including HIV
PCT64.
As the epidemic continues to affect people living in poverty
and people who have historically been disenfranchised, there is an increased
risk that testing can and will be used to discriminate against people infected
with, or even thought to be infected with, HIV and will further isolate people
with AIDS64. Some of quotes got from some participants in FGDs went
even far beyond all type of acceptable discrimination. Just reread this
horrible quote:
|
«Premarital examination is a major measure that helps
reduce the spread of the diseases in new couples. So the government should make
it a law and anyone who has HIV should be rejected and killed, so that he/she
does not spread it to others»!!????? (A 45- year- old mother: FGD of
Traditionalist mothers/Ampoma)
|
If respondents understood compulsory HIV PCT like this, then
it could not work. Thus, policy decisions must incorporate strong protections
for those who are already suffering from discrimination64.
It is true VCT and HIV PCT have helped to control HIV/AIDS and
to target treatment for infected persons in a number of countries, such as
Uganda10. This illustrates the tangible public health benefits of
such screening efforts and explains why some countries have made HIV PCT
mandatory rather than optional10,42. Thus, if HIV PCT programs are
poorly conceived, organized, or implemented, they may lead to interventions of
questionable merit and enhance the vulnerability of groups and
individuals64.
There is the need of still studying further as to whether
compulsory HIV PCT would work or not in the Kintampo District context. Despite
the view of majority of respondents suggesting HIV PCT should be compulsory,
District Health authorities should study the feasibility of this approach,
knowing that optional (voluntary) approach has also failed in some VCT centres
still not or feebly patronized in the country36. Either it starts
under the Voluntary (Optional) or mandatory approach, district authorities
should put in place long term education and sensitization campaign to make sure
HIV PCT later becomes a spontaneous «routine
screening» with the full and straight commitment and
understanding of communities and the target groups.
District authorities should also be aware that it has been
found that when shifting from a type of approach to another, patronization of
HIV PCT is always affected in the way that the number of clients patronizing
premarital service tends to decrease when the examination become optional than
when it was compulsory and to increase when PCT examination is free. The same
study has shown a low rate of voluntary compliance to premarital examination
because of fear of the results.13 They should also examine the
cost-effectiveness of a HIV mandatory premarital screening program based on
current studies 65.
If the approach of compulsory HIV PCT is chosen in Kintampo
District, a cost-effectiveness study should also be planned in order to compare
the cost with the effectiveness of such program. Also if optional HIV PCT
program is to be implemented in accordance with the current National HIV/AIDS
and STI Policy61, then Kintampo district authorities should realize
they are putting in place a system against the views of the majority of the
target group interviewed in this study.
Finally, experience of Uganda with a higher HIV prevalence
rate showed that lack of non-committal in HIV PCT leaves room for being
optional. And this led some religious groups and parents to make testing for
HIV before marriage mandatory, although the Uganda policy supports it should be
rather optional66.
5.2.4. RELATIONSHIP BETWEEN LEVEL OF KNOWLEDGE AND
LEVEL
OF PERCEPTION OF RESPONDENTS TOWARDS
HIV PCT
Findings from Table 7 and Figures 5 and 7 showed that the
entire totality (100%) of respondents in both sexes had «adequate positive
perception» towards HIV PCT irrespective of their
different socio-demographic background. This clarifies with disagreement one of
the factors (bad perception towards HIV PCT) in our initial problem analysis
diagram. Despite Table 8 showed there was a significant weak positive linear
relationship between level of knowledge and perception towards HIV PCT (p-value
0.007), meaning the score of perception slightly increases as the score of
knowledge increases, it was observed however that even respondents with poor
score of knowledge also had higher score of perception. This means
little or average knowledge on HIV PCT is enough to still create a very strong
positive perception towards HIV PCT among unmarried young adults.
This is a proof that little or average knowledge could still result in
generating positive perception towards a given behavior62.The
similarities in score of perception among respondents of low and high score of
knowledge underpins the fact that if we want to raise perception of people
towards HIV PCT practice, we only need to simply create awareness on few
important issues on don'ts and not necessarily bringing
sophisticated scientific matters to them. Therefore the development of BCC and
IEC materials and messages aimed at promoting HIV PCT should be based on
participatory methods and research evidence-based data, leading to the
production of appropriate messages and materials for different target groups
according to their need of knowledge to fill appropriate identified
gaps61.
As a comparison, our results showing adequate positive
perception of unmarried young adults towards HIV PCT are quite similar to
findings in Egypt where ESHRA and Colleagues found that most respondents from
Menofia Governorate, except unmarried males, had a favorable perception towards
HIV PCT50.
5.3. FACTORS INFLUENCING PERCEPTION OF THE NEED OF HIV
PCT
SERVICE AMONG
RESPONDENTS
Perception of the need of HIV PCT service was inversely
(negatively) associated with Urban residence, to the fact of having had
premarital sex and score of knowledge (Table 9).
In fact respondents from urban area were 5 times less likely
to perceive the need of the PCT service than respondents from rural
settlements. This is contrary to what have been reported in a similar study
among Malawians45.This may be due to the fact that young people from
Urban areas may take all things for granted to the point of thinking all their
health need will be automatically satisfied in life irrespective of their own
expression.
Also respondents who have ever had sex were 16 times less
likely to perceive the need of the service than still virgin respondents. This
may be explained by the fact that for those who know they have engaged in risky
premarital sex, fear to know their HIV serologic status may be higher and
worrisome to the extent of leading them not even to perceive the need of such
service10. It even joins the view of some participants in one of the
FGDS.
|
«Because young people have had sex before their
marriage, they fear to go for HIV PCT because of fear of HIV test result,
thinking such service is rather suitable for those still virgin»
(A 43-year- old man: FGD of traditionalist
fathers/Ampoma).
|
Therefore promotion of sexual abstinence and of virginity
through appropriate sex education and establishment of virgin clubs could help
ensure that target groups express and understand the need of such services as
it has been proved in Uganda and Zambia10. Also education and
comprehensive counseling of those who happen to have had premarital sex should
be carried out in order to dissipate the fear those respondents feel.
It was also found that increased score of knowledge on HIV/PCT
was associated with decreased likelihood of the respondent to express the need
of such service. So the higher the score of knowledge (the more knowledgeable a
respondent), the lower the likelihood to perceive the need of HIV PCT service.
This is contrary to our expectations but somehow compares with results from
Malawi where it was found that respondents who had knowledge of sexually
transmitted diseases (STDs), knowledge of HIV testing place were less likely to
desire testing prior to marriage.45 We can't truly explain why it
happens this way but we could say that it is possible that more knowledgeable
people may take their health for granted because of their pride. Also it could
be because it has been shown that although young people have a high level of
knowledge about HIV/AIDS, the internalization or conceptualization of their own
potential risk is very low10. Also according to our findings, it
seems that knowledge would lead to fear of HIV-testing or a sense of
non-vulnerability, such that the need for HIV testing may not be appreciated by
the knowledgeable respondent.
On the other hand, perception of the need of HIV PCT service
was positively associated with older age, females, Christian religion, Akan and
Mo ethnic groups, post-primary educational level, Students and level of
perception towards HIV PCT.
Increased age seemed to increase gradually the likelihood for
the respondents to perceive the need of HIV PCT. This may be due to the fact
that as children grow up they start thinking of the formation of their own
family through marriage. Therefore while seeking for and gathering information
needed on marriage they may hear about and understand the need of such
service.
Females were 19.5 times more likely to perceive the need of
such service than males. This may be justified by the fact that females even
proved slightly higher mean scores of knowledge (15.76 versus 15.68) and of
perception (21.8 versus 21.7) than males. It may also be explained by the fact
that generally females are more flexible and easy to be convinced than males
who are mostly naturally less flexible. Our findings are in some disagreement
with findings from «The Adolescent Counseling and Recreation Centre
(AcRC)» in Kenya and « the Center Dushishoze» , a youth center
in Butare /Rwanda, where it was rather found that more males were expressing
VCT need than female clients10.
Christian respondents were 5.57 times more likely to perceive
the need of HIV/PCT service than non Christian ones. This stands true because
as said earlier on, most Christian religions have started educating and
sensitizing their young adults towards HIV PCT.
Respondents belonging to Akan and Mo Ethnic groups were 2.8
times more likely to perceive the need of HIV/PCT service than respondents from
other Ethnic groups. This could be explained by the fact that Akan and Mo
showed higher scores of knowledge than respondents from other ethnic
backgrounds.
Respondents of post-primary educational level were 4.13 times
more likely to perceive the need of HIV/PCT service than respondents of lower
educational level. This contradicts the above findings showing that score of
knowledge was negatively associated with perceived need of the service. But it
confirms that somehow increased level of knowledge should be translated into
behavior change so as to differentiate those still not adopting a positive
behavior because of their ignorance. It also affirms that educational
attainment may affect the individual's perceptions and thus indirectly
influence health related behavior.64 This explanation may also
explain the fact that students were 4.097 times more likely to perceive the
need of HIV/PCT service than respondents of other professional categories.
Finally increased level of perception towards HIV/PCT
increases by 4.47 times the likelihood for a respondent to perceive the need of
the service than a respondent with lower score of perception. So the higher the
score of perception the higher the likelihood to perceive the need of HIV PCT
service. This stands far true since it is the individual's perceptions towards
an illness or an available treatment or behavior which will lead the individual
valuing the benefit of the action so that he/she can adopt the behavior to
protect him/her to the disease he/she perceived as very
dangerous64.
5.4. FACTORS INFLUENCING WILLINGNESS TO UNDERGO HIV
PCT
Table 10 showed that we could strongly predict the willingness
of a respondent to undergo HIV PCT from his/her readiness to know and accept
his/her HIV result (p<0.001). Therefore the more the
respondent says he /she will be ready to know and accept his/her HIV test
result, the higher the likelihood of the willingness to attend HIV PCT. This
meets findings found in Thailand in a cluster randomized trial used to assess
the effect of an active group intervention in promoting utilization of
voluntary HIV testing and counseling67. In fact since it is
reported that most people fear to know their HIV serologic status10,
it is definitely obvious that an individual who has coped with this fear will
more likely intend to do the test now as he/she feels ready to know and accept
his/her HIV serologic status. Therefore if the service is to be implemented in
Kintampo, many sessions of sensitization and anticipated pre-counseling among
the target groups would be recommended in order to dissipate the anxiety and
the fear clients manifest on the eventual HIV test results.
About other associations, not significant, it was noted that
increased age were associated with low likelihood to intend undergoing HIV PCT.
This finding is in agreement with findings in a study done in 1970 in
Yonsei-Korea among Protestant Ministers on `Knowledge and attitude and practice
about marriage...' where age was found to be the most important factor
influencing the attitude of respondents towards PCT, the younger respondents
showing more positive attitude than the older one. 51 However our
result is inconsistent with explanations given above where increased age seemed
associated with positive perception of HIV PCT service. Our finding is also
inconsistent with findings from a study done in Malawi in 2004 which rather
showed a significant, although weak, association between increasing age and
supporting HIV-testing prior to marriage45. It is possible that
older respondents, who were probably already engaged in many unprotected sexual
intercourses with multiples partners, could not support premarital HIV testing
because of fear of the HIV test results. It is also possible the older groups,
although more appreciative of the reality of HIV/AIDS and their support, think
the test is rather for those still younger. Testimony from one old couple we
interviewed seemed to support this feature.
|
IDI couple whose religious marriage was celebrated on
9th July 2005 in ST.JOSEPH'S CATHOLIC CHURCH KINTAMPO:
«No we did not perform any test at all. We got
married 31 years ago. We did our traditional marriage in August 1974. Those
days there was not something like testing before marriage. Even now
because today is just the religious blessing of our old marriage, it was
useless for us to test for HIV. However nowadays we perfectly
agree that young adults who want to marry should conform to their time and
undergo HIV premarital testing in order to plan better for the future and
secure for good health for themselves, their spouses and
offspring».
|
Students and respondents of post-primary level all seemed less
likely to intend undergoing HIV PCT than their counterparts of other
professional categories. This is in some variance with our previous discussions
concerning the positive association of the two parameters with the positive
perception of the need of HIV PCT services.
Also respondents engaged in premarital sex were less likely to
intend doing a HIV PCT than those still virgin. This confirms the above
findings and stands true by the same explanations that those who have engaged
in risky unprotected sex do not intend to perform the test because of fear of
the HIV test result10. This is because most people think sexual
intercourse is the only major route of transmission of the disease.
One would-be couple with premarital sex history who just
benefited from premarital counseling sessions organized by their pastor in
their local church in Kintampo consented to testify their experience through
this work in order to teach it to others that HIV PCT is still feasible and
helpful despite past sexual bad behaviors.
|
«We are preparing to marry within one month time. We
haven't performed HIV test yet. But after receiving beneficial counseling from
our Pastor, and given the fact that we both mutually recognized and confessed
to each other having been differently involved in premarital sex before we met
for our marriage project, we found better to do HIV premarital testing. The
reason is that we know this disease is contracted through many sources
especially sexual intercourses and others that we are prone to. So there is the
need for us to test, thing that we hope to realize by 2 weeks, so that we check
whether or not we are free of this disease in order to start our marriage life
with certainty and self confidence.»
(IDI: A 25-year-old prospective husband with
his 24-year-old fiancée, Pentecostal
Church/Kintampo, Picture No 18).
|
|
This live testimony strongly proves how counseling sessions
should be promoted and carried out in Kintampo district in order to dissipate
the fear of those unmarried young people who would fear to attend HIV PCT
because of their premarital sex history.
It is not understandable that respondents who yet perceived
the need for the HIV PCT services were now surprisingly less likely to intend
doing the test than those who do not perceive its need at all. This is
completely contradictory to our expectation and partially demonstrates how when
dealing with HIV testing it is difficult to predict a respondent would
concretize his/her own view in doing the HIV test because of so many
parameters, especially the fear of the results10. Reason why long
term pre-counseling sessions could help convince such respondents to finally
intend doing the HIV test.
Individuals who perceived HIV PCT should be provided free of
charge or at affordable cost were less likely to intend doing the test than
others. This can easily be understood insofar as most people not willing to
attend a heath service usually pretend they do not have money to do so even
when they have it. On the other hand individuals who truly felt they were poor
might have hesitated to manifest the willingness to undergo HIV PCT until later
on, once the service will be implemented at free charge, they would may be now
intend to do the test once they are sure it is free.
Individuals living in the urban areas were 3.1 times more
likely than rural dwellers to accept voluntary HIV counseling and testing prior
to marriage. This is similar to results found in Malawi45 but enters
in contradiction with previous observations showing young people from rural
parts perceived more than those from urban areas the need of the implementation
of HIV PCT service. Although we cannot determine the reasons for this
difference on the basis of the current study, this inequality has far-reaching
public health implications because over 80% of unmarried young adults live in
rural areas in the district. Further studies are needed to explore this
discrepancy.
Akan and Mo respondents were 2.5 times more likely to intend
undergoing HIV PCT than respondents from other Ethnic groups. As said earlier
on, this may be due to the fact that they also proved high level of knowledge
on HIV PCT than others. If we consider the fact that Akan and Mo are the most
populous Ethnic groups in the 3 sub-Districts involved in this study and in the
whole district, we could assume at this stage that there is hope that such
service, if implemented, would be patronized much by Akan and Mo respondents,
whether this is true or not.
Christians were 3.6 times more likely to intend undergoing HIV
PCT than respondents of others religion groups. This stands true using the same
explanations mentioned earlier on.
Female respondents were 3.6 times more likely to intend
undergoing HIV PCT than males. This joins findings from Uganda but contradicts
some findings from Kenya and Rwanda.10
Increased score (level) of knowledge and of perception were
positively associated with willingness to undergo HIV PCT. This meets our
expectations because we believe knowledge empowers people to act positively.
However our finding contradicts findings from Malawi.45 In fact as
people perish by ignorance, it is a good thing that knowledge, once acquired,
could help people to adopt positive behaviour than before they got that
knowledge.64 This could also be translated into positive perception
so that those with positive perception show much interest in intending
undergoing HIV PCT than those with negative or low perception of it.
Finally, respondents expressing the high need of
confidentiality were 2.6 times more likely to intend doing the testing than
those who do not. This finding espouses results from a similar study among
Malawians, where Humphreys Misiri and Adamson S. Muula found that those who
preferred maintenance of confidentiality if one is HIV positive were more
likely to accept HIV testing prior to marriage45. This feature
corresponds to the views of most participants in IDI and FGDs who recognized
lack of confidentiality as a major barrier and suggested consequently
maintenance and guarantee of confidentiality as a core way to promote the
service and make it acceptable and attractive for people (see up-coming point
5.7.4).
It should be noted through Table 11 that about 86% of
respondents had paired higher probability (>0.75) of perceiving the need of
HIV PCT service in Kintampo and of willingness to undergo HIV PCT. Assuming
this picture stands true for the whole target population in Kintampo District,
we could be self-confident based on this study that once the service is
implemented, majority (at least 86%) of young people would definitely patronize
it. On the other hand this suggests that not implementing or not promoting HIV
PCT would definitely result in low patronization of the VCT service as
initially presumed in our conceptual framework. This could serve as a motivator
for district authorities to plan for such service as soon as possible.
5.5. PREFERENCE TO UNDERGO HIV VCT FOR MARITAL REASON
OR NOT
Findings in Table 12 suggest that 77% of
unmarried young adults exclusively preferred HIV PCT whereas only minority
(23%) of them preferred HIV Voluntary testing in no marital purposes. Although
the difference between the two trends is not statistically significant, the
findings suggest that most unmarried young adults are less likely to
voluntarily go for HIV testing unless it is for marital reasons, females being
1.36 times more likely than males to prefer undergoing HIV PCT. This supports
findings from the Adolescent Counseling and Recreation Centre (AcRC) in Kenya
where most unmarried young adults who come for the HIV test come for certain
reasons especially premarital purpose10. Therefore as implied in
findings in the previous study on `Formative research for the establishment of
VCT service in Kintampo District'32, the picture in this present
study support that for VCT service to be well patronized, HIV PCT must be
promoted as well so that unmarried young adults could come for it when they are
about to enter into marriage.
5.6. BARRIERS TO HIV PCT ACCEPTANCE AND
IMPLEMENTATION
IN KINTAMPO
DISTRICT
Respondents had to give their view on a long list of 25
barriers drawn from IDI and FGDs.
For easier interpretation perceived barriers described in
Table 13 were grouped under 4 categories, given the frequencies derived from
respondents:
a) Major absolute barriers (Yes = 70%):
These are respectively -High cost (price) of premarital
examinations , -The attitude of the service provider, -Premarital sex and fear
to know their HIV status, -Fear of stigma and discrimination in marriage
(denial of marriage for HIV+), -Ignorance of the importance of PCT, -Inadequate
VCT/PCT facilities, -Lack or inadequate trained personnel & counselors,
-Lack of confidentiality and privacy among health care providers in PCT
services and Little solution for those who test HIV (+) ( no effective drugs to
treat AIDS).
b) Moderate barriers (Yes 50-69%):
These are -Inexistence of regulatory procedures and Law/Policy
on PCT in Ghana, -Mandatory imposition of PCT that infringes the Human Right of
individuals, -The location of the centre/hospital at long distances,
-Reluctance of fiancés, -Preference of young people to get married
without PCT, Polygyny (Polygynous/polygamous marriages) & Islamic
religion, -Marriage by convenience (outside churches & civil registrar
officer or court or without customary ritual) , -Forced marriage (e.g.
traditional early marriage), -unregistered marriage, -Fiancés are in a
hurry to get married very quickly for any reason and -Medical premarital
certificate provided to fiancé(e) by doctors without performing any
medical check-ups (fraud), - Re-marriage (for divorced or widowed), Inability
for girls to negotiate HIV PCT when their prospective husbands don't like it
and Blind love among young people.
c) Minor barriers (Yes 30-49%):
These
barriers regroup - Opposition of some churches and - Opposition of some
parents.
d) Negligible barriers (Yes < 30%).
Barriers grouped under `others» (not providing gifts to
couples) in index number 26 fit to this category.
Most of the major and moderate barriers above have been
identified worldwide in VCT implementation and practice.10,64 Some
of these barriers (fear of lack of confidentiality and privacy, fear of stigma
and discrimination, ignorance) were also identified in the 2004 previous
study32, and therefore merit special interventions for VCT promotion
in Kintampo District.
We discuss some of these barriers here below.
Certain barriers like «Inexistence of specific law on
premarital examinations in Ghana» emerged from official key informants who
wished there should be a specific law describing the scope, the procedures of
the exam. And respondents also gave their approbation on this as a barrier.
This confirmed one of the factors (inexistence of conducive law/policy) in our
initial conceptual framework. But at this stage where some churches have
already started organizing PCT among young people despite the inexistence of
any specific law on PCT, we assume it is not as such a big barrier. However
although this barrier fell among the category of moderate barrier, we still
strongly recommend there should be a specific law/policy on premarital
examinations in Ghana in order to make it clear regarding its scope and
procedures, like it is the case in many other Countries in accordance to
recommendation from WHO11 and from many other authors10.
Mandatory imposition of HIV PCT fell under moderate barriers.
This is simply because from Table 6, majority of respondents (61%) opted that
HIV PCT should be compulsory although it is recognized that mandatory
imposition infringes human right of individuals and therefore push them not to
attend the service10. In fact observations in two states of the USA
(Louisiana and Illinois) where premarital testing was made compulsory showed a
large proportion of premarital couples got married elsewhere in surrounding
states63. This may have happened like that if the governmental
bodies in these two states imposed the compulsoriness of the HIV PCT to people
without consulting them in a base-line study. In our case, if the view of
majority was to be respected in Kintampo based on the current study, we don't
assume that reluctant unmarried young adults would run away and go to marry
elsewhere in Ghana. And even if it happens it will just be a minority. And
since no law can satisfy completely everybody, the service would still function
normally.
Polygyny (polygamous marriages) and Islamic religion fell in
moderate barriers against HIV PCT. We think it is true since qualitative study
also proved similar trend where Moslem girls disapproved polygyny in Islam
during a FGD and recognized it would be a barrier to HIV PCT. This corresponds
partially to findings from a study of the Kaguru people of Tanzania
68
What is paradoxical and interesting in our study is that a
large part of Moslem respondents (43.9%) also recognized their Religion as a
barrier to HIV PCT (Table 14). They were just frank to tell the truth. This led
us to seek an additional IDI from the Imam and one Moslem elder:
|
«People saying Moslem community or Islam is a
big barrier to implementation of HIV premarital examinations in Kintampo are
totally wrong. If some Moslems are also having this conviction, it means they
haven't understood Islam yet. In the history the prophet recommended
examination of prospective spouses before marriage, not textually quoting HIV
test, but implying check-up of their health status. So Islam is not a
barrier.....
|
|
.... It is even rather a protective institution which
contributes very much in reducing HIV spread. Since women are many than men,
men marrying more than one wife help reduce the number of prostitutes who would
be spreading the disease in looking for casual husbands. So we even call
Christians to join Islam in promoting polygamous marriage which, I believe,
will further definitely reduce HIV/AIDS spread and prevalence in the country.
We will soon start sending our young people for HIV premarital test too, things
are in the pipeline. Then, be convinced that Islam is not a barrier to this
beneficial service».(IDI: Imam,Central Mosque/Kintampo, Picture No
22)
|
|
«On the subject of premarital examinations, there is
an Hadith that the Prophet told a man that he should first check carefully the
woman he intends to marry. This could be interpreted in the present days by
having a premarital examination to make sure that there is no danger of all
kind of diseases such as sexually transmitted infections, HIV/AIDS and genetic
consequences for offspring. Therefore there should be extensive campaigns in
the media, churches and Mosques to encourage would-be couples to undertake
these examinations. We are planning to start it in our Mosque. So Islam is not
a barrier at all.»
(IDI: A 46-year-old man, fervent Moslem
believer/Kintampo central Mosque)
|
Without commenting much on the explanation we got from the
Imam, what we can add is that it is true plygyny (polygamous marriage) could be
a barrier, but just a moderate one. This is because through the FGD of Moslem
Girls, it was revealed that most Moslem men do not perform any prior medical
procedure when they choose to marry other wives. However we believe the
integration of HIV PCT in Muslim community would change the current reality so
that people do no longer claim Islam as a barrier to HIV PCT as it has been
proved in many other Islamic Countries where premarital exam is legal and
commonly done14,52. Further studies would be needed in the future to
follow-up this issue if possible.
Finally we recommend in priority that major and moderate
barriers to HIV PCT revealed in this study should be addressed properly in
order to guarantee a smooth take off of VCT and HIV PCT service in the
District.
5.7. KEY ISSUES FROM RESPONDENTS TOWARDS HIV PCT
HEALTH PRACTICE
IN
KINTAMPO DISTRICT
5.7.1. VIEWS ON FREQUENCY OF HIV TEST BEFORE MARRIAGE
AMONG WOULD-BE COUPLES
The points of view of respondents were divergent about the
required number of HIV tests before people marry (Figure 8). It is however
encouraging that a third of them recognized it should be done more than twice,
a fifth saying it should be more than once, and another fifth supporting it
should be just once. All these findings support different levels of knowledge
among respondents regarding HIV laboratory test.
In many countries with legislation on HIV PCT, the HIV test is
required at least once before marriage. But in certain countries like China
12 and certain areas in Democratic Republic of Congo (ECC/CBCA
Church North-Kivu Province), due to the need of testing before the
officialization of engagement, also because of possible lengthy engagement
during which change could occur in serological status of one or both
fiancés, HIV PCT is done at least twice. The first one is undergone
before the onset of official engagement (before payment of pride price) and the
second happens just a few days before the official celebration of the
marriage12.
In this study only 2.6% of respondents opted for the test
being done twice, one before bride price is paid and the second prior to
official celebration of the marriage. This shows that respondents disagreed
with this last option which yet is being used else where.
However it may be, due to the window period, it is normal that
the HIV PCT should be done at least twice, with 3 months interval between the
two tests18.
5.7.2. VIEWS OF RESPONDENTS ON WHO SHOULD SEND
WOULD-BE
COUPLES AT THE HOSPITAL FOR
HIV PCT
From Figure 9, we saw that majority of respondents (42.86%)
suggested that the fiancés themselves should decide and go for test
without any body sending them. This is the best way of doing thing as far as
marriage concerns two people. But this could work well only if couples discuss
in pre-test counseling the implications of discordant/positive results of HIV
test10.
But if we look at the social aspect of marriage, involving
both families, the religious bodies or lawyers, it is possible some times that
a third person (religious leader, counselor...) comes in to play a role of
facilitator. This does not destroy the fact that the test remains first of all
voluntary.
The big issue is on how to manage the positive HIV test
results and to whom to communicate it. Knowing many couples would not be able
to cope with the positive HIV test result alone and decide on marriage project
without the intervention of a third person such as counselors or religious
leaders came in between, we suppose in our opinion that, even if a couple
decides voluntarily to undergo the test, a third neutral body, whether
religious or not, medical or not, counselor or not, is still needed to
facilitate and follow-up their commitment to HIV testing, and help them cope
with the anxiety and the consequences of an eventual HIV test result
vis-à-vis the decision on marriage.
In most of African countries, including Ghana, Religion
Institutions are officially integrated as stakeholders, activists and main
partners in the fight against HIV/AIDS10,61. Thus although only
15.61% of respondents said Religion leaders could send would-be couples for HIV
PCT, this role which is unavoidable should not be neglected since Religion
Institutions are involved in many counseling programs, including HIV PCT. In
our case study Religion institutions are even currently the only reliable and
available structures providing premarital counseling sessions in Kintampo
district. Therefore a religion body who sends would-be couples to undergo HIV
PCT after counseling session is still acting towards the advocacy for an
effective national response to the problem of HIV/AIDS as highlighted in the
National HIV/AIDS policy.61 The district health authorities should
play a coordinating role to train and orient religion institutions in the
directives towards a voluntary consent of would-be couples on HIV PCT.
5.7.3. VIEWS OF RESPONDENTS ON TO WHO THE HIV TEST
RESULT SHOULD
COMMUNICATED TO AFTER A PCT
SESSION
In Figure 10, about one-third of respondents suggested HIV
test results should be communicated to both would-be couples together; others
suggested it should also be communicated to parents or guardians, to religion
leaders etc. This big issue is about how to maintain confidentiality.
Confidentiality and privacy is crucial in VCT and HIV PCT matters10.
But when it comes the necessity of disclosing the test results to the
fiancé(e) so that they both discuss and decide on marriage issue and if
it happens that the marriage relationship breaks up, confidentiality may no
longer be respected.45 And that is where the problem resides. It is
not bad for religion bodies or any other third person to be involved. But the
whole issue is that they should know the HIV test result belongs to the person
and the couples. And the National HIV/AIDS policy is very clear on the issue of
disclosure of HIV/AIDS test results with insistence that health care providers
shall not disclosure any confidential information from the client to any person
without the express consent of the client.61
5.7.4. WAYS TO PROMOTE HIV PCT IN K'PO DISTRICT
For easy classification we wanted to see which measures
should be put in place in decreasing order of priority, depending on what
beneficiaries of the service suggested in Table 15. Thus we created the
following classification scale:
1. First line measure: when 100% of respondents suggest it.
2. Second line measure: when 90-99 % of respondents suggest
it.
3. Third line measure: when 80-89 % of respondents suggest it.
4. Fourth line measure: when 70-79 % of respondents suggest
it.
5. Fifth line measure: when 50-69 % of respondents suggest
it.
6. Sixth line measure: when 30-49 % of respondents suggest
it.
7. Last line measure (negligible): when less than 30 % of
respondents suggest it.
Using the above scale based on the «Yes» frequency
distribution for each measure suggested by respondents, we could deduce from
Table 15 that 15 interventions in 5 gradual steps (Figure 14) are actually
needed in Kintampo district in order to promote HIV PCT.
Depending on the resources available, the district health
authorities should address the suggested measures one by one and step by step
to make sure HIV PCT is established smoothly.
Because 100% of respondents insisted that other tests should
be added to HIV/AIDS in order to reduce stigma associated to HIV/AIDS, this is
a crucial action which should be done in priority as the very first line
intervention. In fact literature supports that premarital examinations should
be global and not selective so that it integrates all required tests such as
Hepatitis B, Sickle cell test, Rhesus factor, just to mention a
few.5,14,15,18 Integration of other tests in premarital screening
has shown success in many parts of the World.10
Others measures such as mass sensitization campaigns, open
discussions on youth sexual education, provision of care and support, reducing
stigma and discrimination associated to HIV have also proved success in VCT
practice wordwide.10
Figure 14 below describes the 15 interventions to be put in place
in 5 steps in order to promote HIV PCT in Kintampo District.
|
|
Figure 14. Steps and actions needed in order to
promote
|
|
|
|
% CI of Yes Answers
|
|
|
|
HIV PCT in the K'po District, based on
suggestions
|
|
|
|
Lower Limit
|
Upper Limit
|
|
|
|
of beneficiary respondents.
|
|
Last line action
|
Step 7
|
-
|
0
|
29%
|
|
|
|
|
|
|
|
15
|
6th line actions
|
Step 6
|
Others (PCT done before pride price is paid, quoting that
couple did PCT during marriage ceremony, PCT films /posters...)
|
30
|
49%
|
|
|
|
|
|
|
|
5th line action
|
Step 5
|
-
|
50
|
69%
|
|
|
|
|
|
14
|
4th line actions
|
Step 4
|
Strictly prohibit all marriage (be it civil, religious or
traditional) before PCT is done, through a decree law
|
70
|
79%
|
|
|
|
|
13
|
3rd line actions
|
Step 3
|
-
|
80
|
89%
|
|
12
|
2nd line actions
|
Step2
|
Setting a specific law (decree-law) on premarital examinations
in Ghana
|
90
|
99%
|
|
11
|
Reducing stigma and discrimination against people living with
HIV/AIDS
|
|
10
|
Creating youth HIV associations/clubs like Virgin club etc
|
|
9
|
Recommending a prenuptial medical certificate from the doctor
for each fiancé before celebration of marriage
|
|
8
|
Providing care and support services for people living with
HIV/AIDS
|
|
7
|
Mention PCT in the health reproductive policies
|
|
6
|
Teach PCT in the health education & reproduction matters
in school
|
|
5
|
Encouragement by providing free treatment for any other
diseases detected among those would-be couples who come for HIV PCT
|
|
|
4
|
Churches and mosques teach PCT to young couple before
marriage
|
|
|
3
|
Open discussions on Youth sexual education about HIV-AIDS and
PCT in youth durbars such as sports...
|
|
|
2
|
Mass sensitization campaigns about PCT through durbars,
Radio/TV, news papers, churches/mosques, NGO, associations, clubs, schools
& university, Hotels, hospitals etc
|
|
1
|
1stline action
|
Step1
|
Add other premarital required tests to reduce stigma
associated to HIV
|
100%
|
|
|
Source: Field Survey, Kintampo, June 2005.
|
|
|
|
|
|
|
5.7.5. WAYS TO CREATE EASIER ACCESSIBILITY TO HIV PCT IN
THE DISTRICT
Majority of respondents (almost 60%) suggested HIV PCT
services should be free or set at affordable cost or paid by the Government or
by any charity NGO in order to make HIV PCT services accessible to
beneficiaries (Figure 11). Another part of respondents expressed that the
number of VCT/PCT centres should be increased and established not at long
distances from communities. This is understandable because majority of
respondents recognized high cost of HIV PCT as a major barrier (Table13). In
fact it has been observed in VCT practice that because of fear of HIV results,
fear of stigma and discrimination associated to HIV/AIDS and little solution to
cure HIV/AIDS, most people are reluctant to do the test, worse still to pay for
their money for HIV testing10,64. Also when we consider the fact
that HIV/AIDS is prevalent in developing countries in poor communities, the
affordability of HIV VCT and HIV PCT becomes questionable. That is why UNAIDS
has recognized scaling up of free VCT centres as the suitable strategies to
fight HIV/AIDS in developing countries8,10,37. Thus in Ghana VCT is
recognized nationwide as part of the strategies for National response to combat
HIV/AIDS. Specifically it is stipulated in HIV/AIDS policy that Government
Agencies and Institutions will ensure increased collaboration in sourcing
resources and technical assistance necessary for the implementation of
programmes and interventions throughout the country35,61. Therefore
establishment of VCT centre providing free HIV tests to people and to would-be
couples would be very helpful in fighting HIV/AIDS in the general population
and new couples in particular in Kintampo district. The only problem associated
to free cost of HIV PCT is that sustainability is very low after financing
institutions withdraw from sponsoring the VCT program10. Thus at the
starting point, the HIV PCT service could be free, but it should be wise to
later put in place some measures to ensure that the program is sustainable and
owned by the community.
5.7.6. WAYS TO MAKE HIV PCT MORE EFFECTIVE, ACCEPTABLE
AND
ATTRACTIVE FOR YOUNG PEOPLE IN K'PO
DISTRICT
In order to deduce interventions to be put in place in
decreasing order of priority, depending on what beneficiaries of the service
suggested for the HIV PCT service to be more acceptable and attractive, we used
similar classification scale mentioned above (point 5.7.4).
Data from Table 16 imply 15 interventions in 4 gradual steps
that are summarized in Figure 15 below.
Obviously, given the proportion of respondents suggesting
confidentiality should be guaranteed, the very first crucial step in launching
the HIV PCT service in Kintampo should actually be maintenance of
confidentiality. The patronization of the service would definitely depend upon
the confidence respondents have in health care providers, regarding how they
are treated with secrecy. This has been proved in VCT practice
worldwide.10
Once confidentiality is worked on, the district authorities
should then tackle other suggested points one by one, and step by step, or even
holistically, to put in place corresponding measures. Thus for instance the
second step would consist of providing care and support services for those
found HIV infected and appointment of well trained personnel, especially
counselors. These are also very crucial in running a very effective and
attractive VCT services as it has been proved in Zambia, Uganda, Kenya and
Chili, just to mention few countries10. In fact the ultimate goal to
do HIV test is to let people who are detected HIV infected have access to a
comprehensive and continuum care and support. These include provision of
antiretroviral drugs, drugs for treatment of opportunistic infections,
psychological and social support10. If clients are being cared for
in a such comprehensive way, then people will appreciate and patronize the VCT
service. Conversely, when clients are not well cared for, the VCT service will
be contested.
The other measures in the subsequent steps could also be
progressively addressed (Figure 15).
|
|
Figure 15. Steps and actions needed to make HIV PCT
practice
|
|
|
|
% CI Yes Answers
|
|
|
|
more acceptable and attractive for young adults,
based on suggestions of beneficiary respondents in K'po
district.
|
|
|
|
Lower Limit
|
Upper Limit
|
|
|
|
|
|
|
|
15
|
Seventh line actions
|
Step 5
|
Others (give marriage gifts to couples, quote that
couple did PCT in marriage ceremony...)
|
0
|
49%
|
|
|
|
|
|
|
|
Sixth line action
|
Step 4
|
-
|
50
|
59 %
|
|
|
|
|
|
14
|
Firth line actions
|
Step 3
|
Appoint young adults counselors
|
60
|
79 %
|
|
|
|
|
13
|
Fourth line actions
|
Step 2
|
Organize more than one counseling session is provided to the
fiancés
|
80
|
89%
|
|
|
|
12
|
Put in place examiner/counselor of the same sex as the
client
|
|
|
|
|
11
|
Conduct follow up of fiancés / newly married after HIV
PCT
|
|
10
|
First line action
|
Step1
|
Put in place counselors not known in the area and or change
continuously the old counselors by new ones after a certain period.
|
90
|
100%
|
|
9
|
Provide entertainment in VCT/PCT centres
|
|
8
|
Provide for unbiased, clear and non-judgmental advices to
would-be couples
|
|
7
|
Provide treatment or effective cure for HIV/AIDS
|
|
6
|
Provide for the presentation of test results as soon as
possible, to reduce the anxiety of waiting to long (same day result
|
|
5
|
Secure permission of patients before passing on information to
anybody (parents, pastors/bishop, Imam and other care providers..)
|
|
4
|
Appoint knowledgeable, well trained, kind, wise and good
communicator examiner/counselors
|
|
3
|
Provide permanent caring and support services
|
|
2
|
Provide HIV PCT at affordable cost or free of charge.
|
|
1
|
Guarantee complete confidentiality and privacy
|
|
Source: Field survey, Kintampo, June 2005.
|
|
|
|
|
|
|
5.7.7. HEALTH FACILITIES WHERE HIV PCT CENTRE SHOULD
BE ESTABLISHED IN KINTAMPO
DISTRICT
As shown in Table 17, 72% of respondents suggested HIV PCT
services should be established in Kintampo District Hospital (KDH), while 75.6%
of respondents from Jema Health (who represented 27% of the whole sample)
expressed that the service should be established in Jema Health Centre. These
findings suggest that respondents knew that KDH fulfills well the required
criteria to run such service given the trained personnel in place (doctors, lab
technicians, Matron-counselor...) and the laboratory equipment available. Those
from Jema just expressed that they wanted the service to be close to them, to
avoid lorry fare as it came up also in FGD where people expressed that HIV PCT
centres should be placed in communities for easier accessibility.
In either case, some thing more must be done now in this
pre-VCT implementation period. If the service is to be implemented in KDH, the
infrastructures for VCT should be prepared now so as to secure privacy and
confidentiality of respondents. The same if the service is to be implemented
else where like in Jema Health centre. In fact the national policy seeks for
the provision of VCT facilities and procurement of VCT commodities such as
laboratory equipment and supplies including reagents for diagnosis and
voluntary testing for HIV61. Since facilities for VCT are currently
limited in the Region and completely inexistent in Kintampo District, special
advocacy efforts should be devoted now to obtaining the support of health
planners at all levels, in both Governmental and Non-Governmental sectors to
allocate resources in their budgets to either rehabilitate existing
laboratories in KDH or build a separate VCT unit , provide VCT materials and
supporting training of qualified personnel towards the implementation of
VCT/HIV PCT service in Kintampo District. Also the implementation of the
VCT/HIV PCT may start at KDH where majority of respondents actually expressed
it to be established, before progressively expanding it later in other places
like in Jema in order to bring the service closer to target groups, depending
on resources available.
5.8. POSSIBLE DECISIONS ON MARRIAGE THAT WOULD-BE
COUPLES ARE MORE LIKELY TO MAKE GIVEN DIFFERENT SCENARIOS OF HIV TEST RESULTS
AND POINT OF VIEW OF RESPONDENTS ON MARRIAGE BETWEEN HIV DISCORDANT WOULD-BE
COUPLESANDHIV
SEROPOSITIVE WOULD-BE COUPLES.
In general, decision on break up of marriage relationship was
strongly prevalent in case of discordant HIV results whereas decisions greatly
diverged when it is about both fiancés testing HIV positive (Figure 12).
This confirms that premarital screening is a major determinant in marriage
choices.69
Our findings support what prevail in Nigeria where calls for
rights of PLWA to marry, although quite significant, still pose problems. In
fact in an article published in April 9th 2003, a journalist wrote
against marriage of PLWA, we quote «However, you will need to
understand that several groups are seriously worried about the spread of
HIV/AIDS in the country. It could be appropriate if we encourage the marriage
of PLWHA to PLWHA, not on the basis of discrimination but to prevent the
further spread of the virus. I therefore think that we all need to observe the
human right not to spread HIV to others if we are infected. Campaigning against
pre-marriage HIV testing is as good as campaigning against the provision of
drugs to PLWHAs.»70
Our findings definitely show there is high popular demand for
HIV PCT among would-be couples, so that young people and their families can
take information on HIV carrier status into account at an earlier stage in the
choice of marriage partner. They also show how denial of marriage right to
PLWA will be a problem which will still enhance stigmatization and
discrimination associated to HIV/AIDS in Kintampo District. Although we
recognize that it is difficult for a person still HIV negative to accept to
marry an HIV infected one, we also recognize that PLWA also have the same right
to marriage as it is recommended by UNAIDS guidelines on the rights of
individuals concerning HIV/AIDS71,72.
What is obvious is that people haven't also understood
availability of PMTCT methods to prevent transmission of the virus from the
mother to the baby. This may explain how few of respondents chose decision to
marry and adopt PMTCT methods in case of discordant couples or HIV infected
couples.
Yet studies have shown that PMTCT (using antiretrovirals &
Cesarean Section, avoiding breastfeeding) and protected sexual intercourse
(permanent condom use) are very effective in limiting further HIV
transmission73, fact that our respondents do not understand well. So
decision on marriage in discordant or HIV infected couples could consist of
marrying and adopting PMTCT or abandoning/limiting childbearing, adoption of
children with permanent condom use, or more sophisticated methods like
artificial insemination73. But our respondents seemed reluctant to
those measures. In FGDs and IDI majority of participants had the conviction
that in actual circumstances it is totally impossible for discordant or HIV
positive couples to permanently perform PMTCT and use condom. And they
suggested that marriage between discordant couples should be rather purely
prohibited (Figure 13). But they seemed agreeing with marriage between both HIV
infected partners, joining the above mentioned view from a Nigerian
Journalist70.
Therefore large campaign of education and sensitization of
young people on Assisted Reproduction in HIV infected people and on
availability of effective preventive measures (PMTCT, permanent condom use)
should also be carried out so that people understand that marriage between
discordant couples or HIV infected couples is still workable.
Chapter Six
CONCLUSION AND RECOMMENDATIONS
We have now come to the end of the study. The main objective
of the study was to generate useful information on current level of knowledge
and perceptions of unmarried young adults towards HIV PCT in order to predict
their acceptance and behaviors towards utilization of such services and to
deduce appropriate program/policy for intervention in the relevant area. The
qualitative and quantitative methods adopted in the study contributed to
respond to our research questions, to verify our conceptual framework and to
achieve the main and specific objectives of the study.
Findings drawn from 150 surveyed unmarried young adults in the
3 sub-districts targeted for the study proved sufficiently the attainment of
our study objectives.
The study findings show that 97% of respondents have good
knowledge and 100% of them have adequate positive perception towards HIV PCT.
Majority of unmarried young adults express the need of HIV PCT service (99.3%)
and show positive acceptance and willingness (98%) towards utilization of such
service in Kintampo District. There is positive linear relationship between
score of knowledge and of perception on HIV PCT with positive perception even
among people with poor knowledge. Thus little or average knowledge on HIV
PCT is enough to still create a very strong positive perception towards HIV PCT
among unmarried young adults.
Willingness to undergo HIV PCT is strongly positively
associated with readiness of a respondent to know and accept his/her HIV result
and negatively associated with age, post-primary education, being a student and
premarital sex. Akan and Mo ethnic groups showed greater preference for HIV
PCT.
Majority of the targeted group show greater preference towards
HIV VCT for marital reason.
Respondents recognize there are some barriers to HIV PCT and
suggest several activities in order to deal with those barriers and make HIV
PCT more effective.
Majority of respondents show disapproval of marriage between
HIV discordant and HIV seropositive couples and presume that they would break
marriage relationship in case of HIV positive results during HIV PCT
session.
Not all populations of unmarried young groups in Kintampo
have an equal likelihood of perceiving the need of HIV PCT service and of
accepting HIV PCT. Therefore Public health intervention (BCC/IEC) in the
district on HIV PCT implementation and promotion should be tailored
specifically for each target group. A policy document is needed to specify the
scope and procedures of premarital examinations in light of the findings in
this study.
Based on the study findings, for the VCT /HIV PCT service to
be successfully implemented, we recommend the following:
A. At the National/Regional level:
1.Since the lack of specific law was stressed as one of
barriers to HIV PCT in Ghana, a specific law and policy document on premarital
examination should be elaborated in light of the findings in order to make
easier the implementation of HIV PCT services.
2. Since the study showed a low rate of awareness acquired on
HIV PCT through mass media and religious bodies, the use of Mass Media and
Religious Institutions in awareness creation on HIV PCT should be enhanced and
coordinated on a regular basis.
3. Given the fact the study showed a very high premarital sex
rate among unmarried adults (66%), considering that participants in IDI and
FGDs also mentioned premarital sex as a core barrier to HIV PCT promotion in
the area, since those who have had sex were less likely to go for test because
they fear they might have been HIV infected, we recommend that:
a) A certain number of measures, such as sex education,
adolescent counseling, creation of virgin clubs, parent's implication in sex
education, reduction of poverty and of illiteracy.., should be put in place
nationwide in order to prevent and reduce the high rate of premarital sex among
young adults.
b) Because pornographic films were recognized as factors
pushing young adults to engage in premarital sex in Kintampo, all cinema
centres where projections of pornographic films take place should be closed in
Ghana in general and in Brong Ahafo Region in particular.
4. Considering the fact that education and awareness creation
on HIV/AIDS is still lacking among some unmarried young adults, promotion of
peer education, including persons/unmarried young adults living with AIDS
should be carried out in order to break up gaps of knowledge on HIV/AIDS and
HIV PCT revealed through this study.
5. Concerning the question whether HIV PCT should be
compulsory or optional, we recommend that the national and regional health
authorities and legislators should put all views together in order to make a
holistic representative and acceptable policy that protect each individual and
the community. Long term education and sensitization campaign and programs are
crucial to make sure HIV PCT later becomes a spontaneous «routine
screening» with the full and straight commitment and
understanding of communities and the target groups.
6. Given similarities in adequate positive perception towards
HIV PCT among respondents of low and high level of knowledge on HIV PCT, we
recommend that the development of BCC and IEC materials and messages aiming at
promoting HIV PCT should be based on participatory methods and research
evidence-based data, leading to segmentation of the audience and to the
production of appropriate messages and materials for different target groups
according to their need of knowledge to appropriately fill specific identified
gaps.
7. Considering the crucial need of confidentiality in VCT and
HIV PCT service mentioned by respondents, we recommend that national health
authorities and the national AIDS control program should ensure that the
personnel (counselors, lab technicians...) are adequately well trained to
maintain confidentiality so that people patronize the service without fear of
lack of confidentiality.
8. Considering the finding that majority of unmarried young
adults (77%) exclusively prefer HIV PCT than Voluntary
testing, we recommend that for VCT service to be patronized very well, HIV PCT
must be implemented and promoted as well so that unmarried young adults could
come for it when they are about to enter into marriage.
B. At the District level:
1. Since it was found that only 31.9% of respondents heard
about HIV PCT through health workers, we recommend that the District should
incorporate HIV PCT among the top IEC/BCC messages in the fight against
HIV/AIDS and multiply IEC/BCC sessions on HIV PCT by Health Workers using
in-service health education of patients or through local mass media (FM
stations, TV, newspapers...).
2. Because the study showed the involvement of schools in
informing young people about HIV PCT seems still very low (29.2%), we recommend
that special programs on HIV PCT should be introduced and intensified in
schools in Kintampo District.
3. Given the high perception of HIV PCT as a social norm
(98.7%), the high perceived need of HIV PCT services (99.3%), the high rate of
willingness (98%) to undergo HIV PCT and the high rate of readiness (96.7%)
of respondents to know and accept their HIV test results after a PCT session,
considering that data from KDH show a timid starting of the service in an
embryonic stage where by now few would-be couples are coming irregularly for
HIV PCT, also knowing that 86% of respondents had a higher probability
(>0.75) of perceiving the need of HIV PCT service in Kintampo and of
willingness to undergo HIV PCT, we recommend that a VCT/HIV PCT service should
be officially implemented in Kintampo District in due course in order to
respond to the need expressed by the beneficiaries of such service still
lacking in the area. Resources should be allocated to the preparation of
infrastructures, equipment, laboratory reagents and for training activities
prior to the launching of such service.
4. Considering the major role of Religious bodies in promoting
HIV PCT, given the fact that majority of would-be couples who came for HIV PCT
so far were counseled by their Churches, we recommend that the District health
authorities should coordinate and train counselors from religious institutions
since their involvement is crucial in managing marriages.
5. Given the fact that results showed we could strongly
predict the willingness of a respondent to undergo HIV PCT from his/her
readiness to know and accept his/her HIV Result, we recommend that if the
service is to be implemented in Kintampo, many sessions of sensitization and
anticipated pre-counseling among the target groups should be continuously
carried out in order to dissipate, through specific and appropriate BCC
messages, the anxiety and the fear clients manifest to know their HIV test
results.
6. In view of many barriers to HIV PCT acceptance and
implementation invoked by respondents in this study, we recommend in priority
that district authorities should address major and moderate barriers one by
one, step by step, or even holistically, in order to guarantee smooth
implementation and take-off of VCT and HIV PCT service in the area.
7 Due to the need of promoting HIV PCT among unmarried young
adults, we suggest that District authorities address properly, in order of
priority, all measures mentioned by respondents and summarized in Figure 14 in
order to promote HIV PCT in Kintampo District. The District should imperatively
collaborate with local religious bodies in order to achieve that.
8. Because majority of respondents (almost 60%) suggested HIV
PCT services should be free or set at affordable cost or paid by the Government
or by any charity NGO, we suggest that district authorities should examine the
possibilities of implementing a free VCT/HIV PCT service through donor
intervention in order to make HIV PCT services accessible to beneficiaries.
9. In order to make HIV PCT more effective,
acceptable and attractive for young people in Kintampo district , district
authorities should apply, in priority order, measures that respondents
suggested and summarized in Figure 15 for VCT/HIV PCT service to be successful
once implemented. Here again we suggest the district health authorities should
imperatively collaborate with local religious bodies in order to achieve
that.
10. Since majority of respondents suggested HIV PCT services
should be established in Kintampo District Hospital (KDH) whilst majority of
respondents from Jema Sub-district rather chose Jema Health centre, we
recommend that the service should be established first in KDH in the
implantation phase. However district authorities should later on assess the
possibility of extending the service in Jema Health centre or even elsewhere in
order to bring the service closer to beneficiaries.
11. Since our inquiry revealed a big lack of official
statistics of marriages in Kintampo District Court although marriages occur
regularly in local religious Institutions, we recommend that local
administrative, judiciary, religion leaders and health authorities examine the
problem in order to reactivate marriage registration in the area.
12. Finally given all information generated in this study, we
recommend that district health authorities make some of the findings useful in
policy-making towards a successful VCT and HIV PCT service in Kintampo
District.
C. At the community level:
1. Since majority of respondents suggested HIV PCT should be
considered as one of current social norms, all community leaders should make
HIV PCT as part of marriage norms.
2. Due to the window period, we recommend that the HIV PCT
should be done at least twice in all communities, with 3 months interval
between the two tests, as a large part of our respondents also suggested it.
Given the lack of knowledge some respondents showed on required frequency of
HIV PCT before marriage, we suggest that the District should target this issue
in awareness creation campaigns. During their counseling sessions, Religious
bodies should orient would-be couples on the required number of tests before
marriage.
3. Knowing many couples would not be able to cope with the
positive HIV test result alone and decide on marriage project without the
intervention of a third person, we recommend that, even if a couple decides
voluntarily to undergo the test, a third neutral body within the community,
whether religious or not, medical or not, counselor or not, should facilitate
and follow-up their commitment to HIV testing, and help them cope with the
anxiety and the consequences of an eventual HIV test result vis-à-vis
the decision on marriage.
4. Since our findings show how denial of marriage right to
PLWA will be a problem which will still enhance stigmatization and
discrimination associated to HIV/AIDS in Kintampo district due to lower
understanding of -use of Assisted Reproduction in HIV infected
Individuals/couples, -use of available protective measures (PMTCT, permanent
condom use) and -adoption of children, large campaign of education and
sensitization of young people and the community on these measures should
intensively be carried out by the district health team, religion bodies and
others NGO involved so that people understand that marriage between discordant
couples or HIV infected couples is possible and workable.
D. At the household level:
1. Since the study showed a very high premarital sex rate
among respondents, parents should educate their young children on sexual
matters, specifically on how to abstain from sex before getting married.
2. Given that it was shown is the study that not all parents
educate their children on HIV PCT, parents should educate their adolescents and
young adults so that they may undergo HIV PCT as a routine examination before
getting married.
E. At individual level:
1. Given the approved importance of HIV PCT, each unmarried
young adult should consider the practice of HIV PCT as an integral part of
marriage preparation and process.
F. To Researchers:
1. Since it was found that Akan respondents were more
knowledgeable on HIV PCT than respondents of the Mo ethnic group, we recommend
that a further study should be carried out in order to deeply research into
this to determine the why of this knowledge discrepancy between these two
ethnic groups.
2. Several other studies should be planned based on the gaps
the current study did not explore.
Contact address:
drjpkmakelele_m_amos@yahoo.frREFERENCES
1 Sally Wehmeier, Oxford Advanced Learner`s
Dictionary of Current English, 6th edition, La Tipographica Varese
Italia/Oxford University press, Oxford-England, 2000:1422 p
2 BERNARD & PIERRE, G., Dictionnaire
médical pour les régions tropicales, Kangu-Mayumbe BERPS,
Congo-Kinshasa1984.
3 DOMART, A. & BOURNEUF, J., Nouveau Larousse
médical, Paris, Larousse, 1992.
4 Ettie A.Rout, safe marriage: A return to sanity,
London, Wood & Sons Ltd, 1922, pp 78, available at
http://www.ibiblio.org, accessed on
March 26th 2005.
5 FERRIER, P.-E., Précis de
pédiatrie, Paris, Doin, 1984.
6 MERGER, R., LEVY, J., MELCHIOR, J., Précis
d'obstétrique, Paris, Masson, 1995: 597 pages
7 Christopher J.L Murray & Alan D. Logez,
Health dimensions of sex and reproduction, The global burden of sexually
transmitted diseases, HIV, perinatal disorders and congenital anomalies,
WHO/Harvard University, Geneva/Boston, 1998, p 552
8 Africa Region, The World Bank, Intensifying
Action against HIV/AIDS in Africa: Responding to a Development Crisis, 1999,
available at
www.worldbank.org
/aidsstratWrldbank.pdf, accessed on 14th January 2005.
9 National reproductive health service policy and
standards, Ghana National RH Service and Standards, 2nd Edition, Accra,
December 2003, 103 pages.
10 Deborah Boswell and Rachel Baggaley, VCT and
young people, A summary overview, June 2002.
11 J.M.Paxman,R.J.Zuckerman, Laws and Policies
affecting Adolescent Health, WHO, Geneva, 1987, 300 pages.
12 Francis Markus ,BBC News, Chinese brides may
keep virginity secrets, Many Chinese women are locked in tradition, Wednesday
31 July 2002,
www.bbc.co.uk in January 2005.
13 Premarital Medical Test May Be Optional,
November 2002, available at
www.china.org.cn, accessed on
17th January 2005.
14 Mandatory Premarital examinations, available at
www.islamtomorrow.com,
accessed on November 27th, 2004
15 Premarital screening, available at
www.bphealthcare.com, accessed
on 16th February 2005.
16 Interdiction marriage pour raison
médicale: Indice de fertilité, qualité du mari, available
at
www.0plus0.com, accessed on February
15th, 2005.
17 Sylvie L.Cohen & Michele Burger, PARTNERING:
A New Approach to Sexual and Reproductive Health, UNPFA, New York, December
2000, 181
18 Premarital screening, available at
www.bphealthcare.com ,
accessed on February 10th, 2005
19 Rajesh Aggarwall and other specialists medical
writers,The Bantam Medical Dictionary,3rd edition,Market House Books
Ltd., New York/USA, April 2000:534
20 LANSAC, J., BERGER, MAGNIN, G.,
Obstétrique pour le praticien, 3e édition, Paris,
Masson, 1997.
21 RONALD, L. KLEINMAN, M. B., Manuel de
planification familiale à l'usage des médecins, London, IPFF,
1981.
22 ROTSART DE HERTAING, I. et J. COURTEJOIE,
Maternité et santé, Kinshasa, BERPS, 1988.
23 M.A. Albar, Counselling about genetic diseases:
An Islamic perspective, Volume 5, Issue 6, 1999, page 1129-1133, available at
www.emro.whc.com, accessed on
25th November 2004
24 Abdel-Meguid N, Zaki MS, Hammad SA, Premarital
genetic investigations: effect of genetic counseling,
Department of Human Genetics, National Research Centre, Cairo, Egypt,
available at www.ncbi.nlm.gov, accessed on January 23rd, 2005.
25 FOUNTAIN, D. et J. COURTEJOIE, Infirmier,
comment bâtir la santé?, Kangu-Mayumbe, BERPS, 1982.
26 Indiana University Health Center, Laboratory
Frequently Asked Questions, available at
www.indiana.edu/health,
accessed on February 11th , 2005.
27 The Premarital and Pre pregnancy Health Check-Up
Program, available at
www.samitij.co.th, accessed on
February 10th 2005
28 District profile, Kintampo District Health
Directorate, January 2005
29 National AIDS/STI Control Programme(NACP)/Ghana
Health Service, HIV/AIDS in Ghana: Current situation, Projections, Impacts,
Interventions, 4th edition, Accra, September 2004
30 Kintampo District Health Directorate, 2003-2004
annual reports.
31 Dr Mohammed Bin I., Performance Review Report
2004,Regional Health Directorate, Brong Ahafo Region, March 2005, 92 pages.
32 Elizabeth Okoth, Dissertation, Formative
research for establishment of VCT in Kintampo, School Public Health, University
of Ghana, Accra August 2004.
33 Adolescent Reproductive Health policy,Government
of Ghana, National Population Council, October 2000, pages 34.
34 National Population Policy, Government of Ghana,
National Population Council, The Advent Press, Accra/Ghana, Revised Edition,
1994, pages 56.
35 Strategic framework for HIV/AIDS in Ghana
2001-2005, April 2000.
36 National AIDS Control Program Bulletin, Quartely
Technical Bulletin on HIV/AIDS in Ghana-NACP/GHS, Vol.1 No, 2 December 2003.
37 UNAIDS/WHO, AIDS epidemic update, December 2004,
available at
www.unaids.org, accessed on January
20th 2005.
38 National AIDS Control Program Bulletin, HIV
sentinel survey, 2004 report, March 2005,Accra.
39 E.Douglas Scutchefield, C.William Keck,
Principles of public health practice,Delmar, USA,1997, pp 377.
40 World Vision Ethiopia, Youth VCT Linkage and
Referral project, available at
www.etharc.org/ethiopiavct,
accessed on 9th January 2005.
41 UNDP, Fight against HIV/AIDS,
Socio-Cultural study on HIV/AIDS prevention in Liberia, 2001, 80 p, available
at
www.mirror.undp.org/liberia/aidshiv,
accessed on Febrary 20th, 2005.
42 VCT UNAIDS Technical update.English original,
May 2000. UNAIDS Geneva WC 503.6 (
www.unaids.org)
43 National AIDS Control Program (NACP) Bulletin,
vol 2, N0 1 July 2004, Accra
44 UNPFA, Voluntary Counselling and Testing (VCT)
for HIV Prevention, 2003, available at www.unpfa.org/hiv/prevention, accessed
on 9th January 2005.
45 Humphreys Misiri, Adamson S.Muula, Attitudes
towards premarital testing on HIV among Malawians, CMJ, 2004, available at
www.cmj.hr/2004/4501/17undMISIRI.pdf,
accessed on February 20th, 2005.
46 Schumm WR, Resnick G, Silliman B, Bell DB,
Premarital counseling and marital satisfaction among civilian wives of military
service members,School of Family Studies and Human Services,
Kansas State University, Manhattan 66506-1403, USA, available at
www.ncbi.nlm.gov, accessed on
January 23rd, 2005.
47 Canadian Legal Information Institute, Premarital
Health Examination Act, available at
http://www.canlii.org/pe/laws/sta/p-18/20041117/whole.html,
accessed on February 11th 2005.
48 Marriage Laws in Indiana state/USA, available at
www.usmarriagelaws.com
/state/license , accessed on February 10th 2005.
49 Obtaining Premarital Medical certificate,
Massachusset, General Laws, Chapter 207, available at
www.ci.smerville.ma.us/premaritalform.pdf
, accessed on 12th February 2005.
50 Eshra D.K., Dorgham L.S, El-Sherbini A.F,
Knowledge and attitudes towards premarital counseling and examination,
available at
www.ncbi,nlm.nih.gov accessed
on November 24th, 2004.
51 Joo Sook Kim, Seung Yu and Il-Soon Kim,
Protestant Ministers`knowledge, attitude and practice about family planning,
sex education and marriage, Yonsei Medical journal, Yonsei University, KOREA,
1970, 13
52 Jordan National Population Commission/The
futures Policy project, Analysis of policy and legal barriers to improved
reproductive health services in Jordan, May 2000, 51p.
53 Ghana Demographic and Health Survey, 2003.
54 MYST, M. , J. PIERRIENS, I. LEBUGHE, et al.,
SIDA : Guide pratique destiné au corps médical, Kinshasa,
B.C.C. / Projet SIDA, 1990.
55 J.Khanna,P..F.A. Van Look, P.D.Griffin,
Reproductive health: a key to a brighter future, special programme of
research,development and research training in Human Reproduction, WHO ,Geneva,
1992, 167
56 Professor John S.Nabila, Dr Clara Fayorsey and
Dr Matilda Pappoe,«Youth and reproductive health in Africa, Assessment of
Adolescent reproductive health needs in Ghana»,UNFPA-USAID-CEDPA-JHU/PCS,
Media-Design Legon-Ghana, February 1997, 130 pages
57 Sharifah Tahir and Dr Nanta Auamkul, THAILAND
Moving towards comprehensive reproductive Health services, ICOMP, September
1998, Malaysia, p 36
58 Marcello Pagano, Kimberlee Gauvreau, Principles
of Biostatistics, 2nd ed.,New York.
59 BBC News / Asia-Pacific/Premarital sex
«Usual in China», October 2003, available at
www.bbc.co.uk, accessed on
15th March 2005.
60 Adetoundo O.Lucas and Herbert M.Gilles, Short
Textbook of Public Health, Medicine for the Tropic, Chennai/India,
4th Edition, 2003, 389 pages.
61 National HIV/AIDS and STI Policy, Ghana AIDS
Commission, August 2004.
62 Glanz, Karan et al, Behaviour and Education.
Theory and Practice, Josey, Bass Publishers, 1990.
63 Dr. Frerichs ,Personal screening for HIV in
developing countries, June 12th 1994.
64 Michael A. Stoto, Donna A. Almario, and Marie
C., Public Health Screening Programs, Reducing the Odds Preventing Perinatal
Transmission of HIV in the United States, McCormick, Editors, USA, available at
www.hivdent.org, accessed on 12
April 2005.
65
P. D. Cleary et
al,
Compulsory premarital
screening for the human immunodeficiency virus. Technical and public health
considerations, available at
www.jama-assn.org, accessed on
15th June 2005.
66 Uganda HIV Policy,
www.aidsuganda.org, 12 April
2005.
67 Chuleeporn Jiraphongsa et al, Acceptance of HIV
Testing and Counseling Among Unmarried Young Adults in Northern Thailand,
available at
www.extenza-eps.com, accessed
on 20th February 2005.
68 Sexual and Reproductive self-determination,
Voluntarism and Marriage, available at
www.unfpa.org, accessed on
24th January 2005.
69 Premarital screening and choice of marriage
partner, available at
www.emro.who.int /publications,
accessed on 5 June 2005.
70 Raphael Oko, Can PLWA marry under Nigerian law?,
available at
http://www.nigeria-aids.org,
accessed on 7th July 2005.
71 Albania: Disability and the Right to Marry,
Amnesty International- November 2004, available at
www.pili.org, accessed on
8th June 2005
72 Human Rights and Public Health: An Overview,
available at
http://www.aidslaw.ca,
accessed on 7th July 2005.
73 Recommended Ethical Principles Regarding the Use of
Assisted Reproduction in HIV Infected Individuals, available at
http://www.27802211.com ice/program
/program8. htm#appe1 , accessed on June 15th 2005
ANNEX 1. QUESTIONNAIRE FOR THE SURVEY
|
|
CODEcode
|
|
KNOWLEDGE AND PERCEPTIONS TOWARDS PREMARITAL
COUNSELLING AND TESTING (PCT) ON HIV INFECTION AMONG UNMARRIED YOUNG ADULTS IN
KINTAMPO DISTRICT
|
FORM NO
|
FORMNO
|
ADMINISTER THIS QUESTIONNAIRE TO UNMARRIED ADULTS
BETWEEN 15-30 YEARS
1. BACKGROUND and ID:
CODEC(*)ode
|
Sub District
|
|
CODESD
|
|
Village/Code
|
|
|
CODEVILL
|
|
Compound Number
|
|
|
|
|
|
|
|
CODECO
|
|
Respondent ID:
|
|
|
|
CODERES
|
|
KDSS PERMANENT ID
|
|
|
|
|
|
|
|
|
|
|
|
CODKDSS
|
|
Date of visit:
..................................................
|
|
|
|
|
|
|
DATEVISIT
|
|
Staff code:
......................................................................................
|
|
|
CODESTAF
|
2. SOCIO-DEMOGRAPHIC BACKGROUND OF RESPONDENT
|
1 Sex
|
1. Male
|
2. Female
|
BSEX
|
2 a .Highest educational level reached
|
1. None
|
2. Primary school
|
3. Middle/continuation school/JSS
|
BEDULEV
|
|
4.Technical/commercial/SSS
secondary school
|
5. Post-middle college - teacher training, secretarial
|
6. Post secondary - nursing, teacher, polytechnic, etc.
|
|
|
7. University
|
8. Not known
|
///////////////////////////////////////
|
|
|
b. Number of years successfully completed at the highest level
reached [88 = NK]
|
|
|
BEDUYRS
|
3.What is your religion?
|
1.Catholic
|
2. Protestant
|
3. Pentecostal
|
4. Muslim
|
5. Traditional African
|
6. No religion
|
7. Other:
|
BRELIGN
|
4.What ethnic group do you belong to?
|
11. Akan: Bono, Ashanti, Fanti
|
12. . Mo
|
13. Gonja, Dagomba,
|
14. Konkomba, Basare
|
BETHNIC
|
|
15.Frafra, , Grushie,
|
16.Mamprusi, Kusasi
|
17. Dagarti, Sisala, Wala
|
18. Other
|
|
|
5. a. Age
|
|
|
BAGE
|
|
b. Age group*(*):
|
1. 15 -19 yrs
|
2. 20 - 24
|
3. 25 - 30
|
BAGEGRP
|
|
6. Profession
|
1. Farmer
|
2. Government worker
|
3.Trader
|
BPROFES
|
|
4. Student/Pupil
|
5. Other:
|
|
7.Location/Residence area
|
1. Rural
|
2. Urban
|
BLOCATN
|
3. PREMARITAL SEX HISTORY AND STI-HIV/AIDS RISK
FACTORS
|
8.Have you ever had sex?
|
1. Yes
|
2. No
|
HAVESEX
|
|
9.How old were you when you first had sex?
|
|
|
9.NA
|
HAGEFSX
|
|
10. Number of sexual partners ever had
|
|
|
9.NA
|
HASXPAR
|
4.3.4. 4.3.5. 4.
GENERAL KNOWLEDGE (AWARENESS) ON STI, HIV/AIDS, VCT AND PCT
|
11. Do you know or have you known a young adult who
suffers/suffered from
HIV/AIDS?
|
1. Yes
|
2. No
|
KPHAIDS
|
|
12. Do you know that unprotected pre-marital sex with
casual/multiple
partners is a risky behaviour that could expose to
STI-HIV/AIDS?
|
1. Yes
|
2. No
|
8. NK
|
KRISKSX
|
|
13. Can a child be born HIV positive from sexual union of his/her
parents/mother?
|
1. Yes
|
2. No
|
8. NK
|
KMTCTH
|
|
14. Do you know that HIV/AIDS does not have any effective
cure?
|
1. Yes
|
2. No
|
8.NK
|
KNOCURE
|
|
15. Are all sexual unions and marriages safe and good for health
of both
partners and offspring?
|
1. Yes
|
2. No
|
8. NK
|
KSAFEMA
|
|
16. If no to Q 15 what makes it unsafe?
|
1. Because of HIV/AIDS
|
2. Other diseases
|
3. Both 1 & 2
|
8.NK
|
9. NA
|
KUNSAFE
|
|
17. Would you consider health status as core criteria when you
choose your
marriage partner?
|
1. Yes
|
2. No
|
8.NK
|
KSCRITE
|
18. If yes to Q 17 how would you assess «Good Health
Status» of your marriage
partner before marriage?
|
1. By observing his/her appearance
|
2. By asking close family member/friends
|
KHSASS
|
|
3. Through premarital medical examination
|
4. Others:
|
8.NK
|
9. NA
|
|
19. Have you ever heard about HIV voluntary counselling and
testing (VCT)?
|
1. Yes
|
2. No
|
KHHVCT
|
|
20. Have you ever heard about HIV premarital counselling and
testing (PCT)?
|
1. Yes
|
2. No
|
KHHPCT
|
21. If yes to Q 20, how did you hear about it?
|
1. Radio/TV/Cinema/Video
|
2. Health
workers
|
3. News papers or
books or posters
|
4. Churches or mosques
|
|
5. Conference/youth camp
|
6. School
|
7. Internet
|
8. Friends/third person
|
|
9. Parents
|
10. Others
|
99. NA
|
|
21.1. How hear 1
|
|
|
KWHPCTA
|
|
21.2. How hear 2
|
|
|
KWHPCTB
|
|
21.3. How hear 3
|
|
|
KWHPCTC
|
|
21.4. How hear 4
|
|
|
KWHPCTD
|
|
21.5. How hear 5
|
|
|
KWHPCTE
|
|
21.6. How hear 6
|
|
|
KWHPCTF
|
|
22. Do you think HIV PCT is one of the main measures to limit the
spread
of HIV/AIDS in new couples in Kintampo district and in
Ghana?
|
1. Yes
|
2. No
|
8. NK
|
KPCTLIM
|
|
23. Do you know of someone or a couple who underwent HIV PCT
before marriage?
|
1. Yes
|
2. No
|
8. NK
|
KCHPCT
|
24. Who is required to undergo Premarital Counselling and Testing
(PCT)?
|
1. The male partner
|
2. The female partner
|
3. Both partners
|
8. NK
|
KPCTARG
|
25. What are some of the major advantages of HIV PCT?
|
1. To know about their health and HIV status so that they decide
responsibly about marriage.
|
2. Stability and safety in marriage
|
|
|
3. To ensure fertility in couples
|
4. It strengthens marital relationship and
enhance marriage satisfaction
|
8.NK
|
|
25.1. Advantage 1
|
|
|
KADVANA
|
|
25.1. Advantage 2
|
|
|
KADVANB
|
|
25.1. Advantage 3
|
|
|
KADVANC
|
|
*(*)*a. Score Knowledge on HIV PCT (
please leave these two questions blank)
|
|
|
KSCORE
|
|
b. Level of
Knowledge
|
1 Adequate Good
|
2. Average good
|
9. Poor
|
KSCOREA
|
5. PERCEPTIONS AND ACCEPTANCE TOWARDS PCT
26. Do you know that you or your partner [fiancé (e)]
though apparently healthy
|
can be an unknown carrier of HIV/AIDS that could be
detected
during PCT?
|
1. Yes
|
2. No
|
8. NK
|
PERRISK
|
|
27. Is HIV-AIDS a very dangerous/fatal disease that you fear very
much?
|
1. Yes
|
2. No
|
8. NK
|
PERSEVR
|
28. Do you think that there is a high risk of getting married
unknowingly to an HIV
|
infected person and of becoming HIV infected when two
fiancés do
not attend any premarital medical examination on HIV
test?
|
1. Yes
|
2. No
|
8. NK
|
PTHREAT
|
|
29. Do you believe that HIV Premarital Counselling and Testing
(PCT)
is important?
|
1. Yes
|
2. No
|
8. NK
|
PERSBEN
|
|
30. Do you believe you are self-confident and able to decide your
self to
undergo HIV PCT?
|
1. Yes
|
2. No
|
8. NK
|
PSELFFI
|
|
31. Do you believe that your family will support you or
encourage you to perform HIV PCT before getting married?
|
1. Yes
|
2. No
|
8. NK
|
PSNORMA
|
|
32. Do you believe that your peers will support you or
encourage you to perform HIV PCT before getting married?
|
1. Yes
|
2. No
|
8. NK
|
PSNORMB
|
|
33. Should HIV PCT be institutionalised in the district, the
country, the society,
as well as in churches and mosques etc?
|
1. Yes
|
2. No
|
8. NK
|
PSNORMC
|
34. If yes to Q 33, with the objective of limiting the spread of
HIV/AIDS in
|
new couples nationwide, do you think HIV
PCT should be compulsory or optional?
|
1. Compulsory
|
2. Optional
|
8. NK
|
9. NA
|
POPTION
|
|
35. In your opinion, will there be some barriers to HIV PCT
implementation in Kintampo district?
|
1. Yes
|
2. No
|
8. NK
|
PCTBARR
|
36. Do you think the following can be a barrier which can prevent
young unmarried people from going for HIV PCT
services at the Hospital?
|
36.1. Inexistence of regulatory procedures and Law/Policy on
PCT in Ghana
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARA
|
|
36.2. Mandatory imposition of PCT which is against the Human
Right of individuals
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARB
|
|
36.3. High cost (price) of premarital examinations
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARC
|
|
36.4. The location of the centre/hospital at long distances
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARD
|
|
36.5. The attitude of the service provider
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARE
|
|
36.6. Premarital sex and fear to know one's HIV status
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARF
|
|
36.7. Fear of stigma and discrimination in marriage (denial of
marriage for HIV+)
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARG
|
|
36.8. Ignorance of the importance of PCT
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARH
|
|
36.9. Reluctance of fiancés
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARI
|
|
36.10. Preference of people to get married without PCT
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARJ
|
|
36.11. Opposition of some churches
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARK
|
|
36.12. Opposition of some parents
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARL
|
|
36.13. Polygyny (Polygymous/polygamous marriages) & Islamic
religion
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARM
|
|
36.14. Marriage by convenience (outside churches & civil
registrar
officer)
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARN
|
|
36.15. Forced marriage (e.g traditional early marriage)
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARO
|
|
36.16. Unregistered marriage
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARP
|
|
36.17. Inadequate VCT/PCT facilities
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARQ
|
|
35.18. Lack or inadequate trained counsellors
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARR
|
|
36.19. Fiancés are in a hurry to get married very quickly
for any
reason
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARS
|
|
36.20. Lack of confidentiality and privacy among health
workers
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBART
|
|
36.21. Medical premarital certificate provided by doctor without
any
medical check-ups (fraud)
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARU
|
|
36.22. Re-marriage ( for divorced or widowed)
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARV
|
|
36.23. Inability for girls to negotiate for HIV PCT when boys
don't
like it
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARW
|
|
36.24. Little solution for those who test HIV (+) ( no effective
drugs
to treat AIDS)
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARX
|
|
36.25. Blind love
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARY
|
|
36.26.
Others:....................................................
|
1. Yes
|
2. No
|
8. NK
|
9. NA
|
PBARZ
|
37. Which do you prefer: HIV Voluntary Counselling and Testing
(VCT) outside
marriage context or HIV Premarital Counselling and
Testing (PCT)?
|
1.VCT outside marriage context
|
2. HIV PCT
|
3. Both
|
4. None of them
|
8. NK
|
PREFVP
|
|
38. Do you think there is the need of implementing HIV PCT
services in
Kintampo district in the fight against HIV/AIDS in new
couples?
|
1. Yes
|
2. No
|
8. NK
|
PNEEDP
|
|
39. Will you undergo HIV PCT with your fiancé (e) before
Marriage?
|
1. Yes
|
2. No
|
8. NK
|
PWILIN
|
|
40. If yes to Q 39 will you really be ready to know and accept
your
HIV test result from the doctor?
|
1. Yes
|
2. No
|
8. NK
|
9.NA
|
PRESULT
|
|
*(*)*Score Perception towards HIV PCT
( please leave these two questions blank)
|
|
|
PSCORE
|
|
Level of Perception
|
1. Adequate Positive
|
2. Average positive
|
9. Negative (Bad)
|
PSSCOREA
|
6. KEY SUGGESTIONS TOWARDS HIV PCT HEALTH PRACTICE
41. How often would you like the HIV PCT to be set before
marriage?
|
1. Once, just 2-3 months prior to
marriage
|
2. Twice, the 1st before bride price is paid, and the
2nd one prior to the celebration of the
marriage
|
SHOFTEN
|
|
3. At least once at any time
before marriage
|
4.The PCT frequency should depend and vary according to the
length of the engagement/marriage period
|
|
5. More than 2 times before the celebration of marriage, with 3-
6 months interval between 2 tests.
|
6. Others:
|
8.NK
|
42. In your opinion, who should send would-be couples to the
hospital for HIV PCT?
|
11. The registry officer in case
of civil marriage
|
12. Churches/mosques in case of
religious marriage
|
13. Parents/family of
woman
|
|
14. Parents/family of man
|
15. Parents/family of both
|
16. Both man and woman
on their will
|
|
17. Community leader
|
18. Other
|
88. NK
|
|
42.1. Who should send would-be
couples 1
|
|
|
SHSENDA
|
|
42.2. Who should send would-be
couples 2
|
|
|
SHSENDB
|
|
42.3. Who should send would-be
couples 3
|
|
|
SHSENDC
|
|
42.4. Who should send would-be
couples 4
|
|
|
SHSENDD
|
|
42.5. Who should send would-be
couples 5
|
|
|
SHSENDE
|
43. To whom should the HIV test results be communicated to by the
doctor after PCT session?
|
11. The concerned fiancé(e)
only
|
12. To both fiancé(e)s,
separately
|
13. The parents or
guardian of the fiancés
|
|
14. The church/mosque involved in
the religious marriage process
|
15. The registry officer involved
in the civil marriage process
|
16. To both fiancés together
|
|
17. The brothers or sisters of the
concerned fiancés
|
18. Other
|
88. NK
|
|
43.1. Communication of PCT
results 1
|
|
|
SRECOMA
|
|
43.2. Communication of PCT
results 2
|
|
|
SRECOMB
|
|
43.3. Communication of PCT
results 3
|
|
|
SRECOMC
|
|
43.4. Communication of PCT
results 4
|
|
|
SRECOMD
|
|
43.5. Communication of PCT
results 5
|
|
|
SRECOME
|
44. What ways/means should be used in order to promote HIV PCT
in Kintampo district/Ghana?
|
44.1. There should be a specific law (decree-law)on premarital
examinations in
Ghana
|
1. Yes
|
2. No
|
8. NK
|
SPROMOA
|
|
44.2. Mass sensitisation campaigns about PCT through durbars,
Radio, TV, news
papers, clubs, churches, mosques, NGO, schools,
university, Hotels, hospitals
etc
|
1. Yes
|
2. No
|
8. NK
|
SPROMOB
|
|
44.3. PCT should be taught in the health education &
reproduction matters in school
|
1. Yes
|
2. No
|
8. NK
|
SPROMOC
|
|
44.4. Strictly prohibit all marriage (be it civil, religious,
traditional) before PCT,
through a decree law
|
1. Yes
|
2. No
|
8. NK
|
SPROMOD
|
|
44.5. Providing care and support services for people living with
HIV/AIDS, including would-be couples found HIV positive after PCT.
|
1. Yes
|
2. No
|
8. NK
|
SPROMOE
|
|
44.6. Creating youth HIV associations/clubs like Virgin club
etc
|
1. Yes
|
2. No
|
8. NK
|
SPROMOF
|
|
44.7. PCT should be clearly mentioned in the health reproductive
policies of Ghana
|
1. Yes
|
2. No
|
8. NK
|
SPROMOG
|
|
44.8. Open discussions on Youth sexual education about HIV-AIDS
and PCT in
youth durbars such as sport.
|
1. Yes
|
2. No
|
8. NK
|
SPROMOH
|
|
44.9. Churches and mosques should teach PCT to young couple
before marriage.
|
1. Yes
|
2. No
|
8. NK
|
SPROMOI
|
|
44.10. Strictly recommend a prenuptial medical certificate from
the doctor for each
fiancé before celebration of marriage
|
1. Yes
|
2. No
|
8. NK
|
SPROMOJ
|
|
44.11. Reducing stigma and discrimination against people living
with HIV/AIDS
|
1. Yes
|
2. No
|
8. NK
|
SPROMOK
|
|
44.12. Add other premarital required tests a part from HIV test
in order to reduce
stigma associated to HIV/AIDS
|
1. Yes
|
2. No
|
8. NK
|
SPROMOL
|
|
44.13. Encouragement by providing free treatment for any other
diseases detected
among those would-be couples who come for HIV PCT.
|
1. Yes
|
2. No
|
8. NK
|
SPROMOM
|
|
44.14. Others:
|
1. Yes
|
2. No
|
8. NK
|
SPROMON
|
45. In your opinion what should be done so that unmarried young
people have easier
access to HIV PCT in Kintampo?
|
1. HIV PCT is to be free or set at affordable
cost/fees in all hospitals
|
2. HIV PCT fees are to be paid by the
government/NGO
|
|
3. HIV PCT fees are to be paid equitably
by both fiancés
|
4. Increase number of hospitals/centre
providing VCT and PCT services
|
|
5. VCT and PCT centres not at long distances
|
6. Others:
|
|
8. NK
|
//////////////////////////////////////////////////////////////////
|
|
45.1. Access to HIV PCT in
Kintampo District 1
|
|
|
SACCESSA
|
|
45.2. Access to HIV PCT in
Kintampo District 2
|
|
|
SACCESSB
|
|
45.3. Access to HIV PCT in
Kintampo District 3
|
|
|
SACCESSC
|
|
45.4. Access to HIV PCT in
Kintampo District 4
|
|
|
SACCESSD
|
46. What do you suggest for the HIV PCT practice to be more
effective, acceptable and attractive
to unmarried young people in Kintampo district?
|
11. Provide for unbiased, clear and non-judgemental advices to
would-be couples
|
1. Yes
|
2. No
|
8. NK
|
SEFECTA
|
|
12. Secure permission of patients before passing on information
to anybody (parents, pastors/bishop and other care providers.)
|
1. Yes
|
2. No
|
8. NK
|
SEFECTB
|
|
13. Provide permanent caring and support services for PLWA
|
1. Yes
|
2. No
|
8. NK
|
SEFECTC
|
|
14. Examiner/counsellor of the same sex as the client
|
1. Yes
|
2. No
|
8. NK
|
SEFECTD
|
|
15. To be counselled by knowledgeable, well trained, kind, wise
and good communicator examiner/counsellors
|
1. Yes
|
2. No
|
8. NK
|
SEFECTE
|
|
16. To be counselled by counsellors not known in the area and or
change continuously the old counsellors by new ones after a certain period.
|
1. Yes
|
2. No
|
8. NK
|
SEFECTF
|
|
17. Follow up of fiancés / newly married is done after HIV
PCT
|
1. Yes
|
2. No
|
8. NK
|
SEFECTG
|
|
18. Guarantee complete confidentiality and privacy
|
1. Yes
|
2. No
|
8. NK
|
SEFECTH
|
|
19. Provide for the presentation of test results as soon as
possible, to reduce the anxiety of waiting too long (same day result)
|
1. Yes
|
2. No
|
8. NK
|
SEFECTI
|
|
20. Affordable cost or free HIV PCT examination
|
1. Yes
|
2. No
|
8. NK
|
SEFECTJ
|
|
21. To be counselled by young adults counsellors
|
1. Yes
|
2. No
|
8. NK
|
SEFECTK
|
|
22. More than one counselling session is provided to the
fiancés
|
1. Yes
|
2. No
|
8. NK
|
SEFECTL
|
|
23. When there will be a treatment or cure for HIV-AIDS
|
1. Yes
|
2. No
|
8. NK
|
SEFECTM
|
|
24. Provide entertainment in PCT VCT centres
|
1. Yes
|
2. No
|
8. NK
|
SEFECTN
|
|
25. Others.
|
1. Yes
|
2. No
|
SEFECTO
|
|
47. In your opinion in which health facility in the district
should a PCT centre be
established?
|
|
|
SPCTFAC
|
USE THE HOSPITAL KEY BELOW TO ANSWER QUESTION 46
HOSPITALS AND CLINICS IN KINTAMPO DISTRICT
|
11. KINTAMPO Hospital, Kintampo
|
12. ADOM Mat. Home, Jema
|
|
13. JEMA Health Centre, Jema
|
14. ANYIMA Health Centre, Anyima
|
|
15. AMOMA Health Centre, Amoma
|
16. NEW LONGORO, Health Centre
|
|
17. DAWADAWA, Health Centre
|
18. PERPERTUAL Mat. Home, Apesika
|
|
19. KUNSU Health Centre, Kunsu
|
20. EBENEZER Mat. Home, Kintampo
|
|
21. ARMS Mat. Home, Ajina
|
22. ANNOA ASARE Memorial clinic
|
|
23. BUSUAMA Health Centre, Busuama
|
24. PRINCE OF PEACE Maternity clinic
|
|
25. In any one of the above facilities
|
26. In all the above facilities
|
27. In none of them
|
88.NK
|
7. DECISION-MAKING ON MARRIAGE VIS A VIS HIV TEST RESULTS
AFTER PCT
48. Assuming that after a premarital examination you are found to
be HIV negative but your
fiancé (e) is detected HIV positive and the
doctor/counsellor advises you so that you decide
responsibly. Of the following decisions which one will you
more likely make?
|
1. Marry her/him but abandon childbearing
(permanent contraception) and +protected sex
(condom use) all the time
|
2. Marry her/him but abandon childbearing
(permanent contraception),adopt children +
protected sex (condom use) all the time
|
DMNGPOS
|
|
3. Marry if my partner accepts, limit childbearing with strict
and continuous prevention of mother-to-child transmission of HIV for all
pregnancy and breastfeeding.
|
4. Break up of engagement/marriage
relationship and search/choice of
an other healthy partner
|
|
5. None of them, I will still marry her/him , have unprotected
sex and bear children irrespective of all advices, because I
love her/him and marriage is for the best and the worst
|
6. Other
|
8. NK
|
49. Assuming that after a premarital examination you are found
to be HIV positive but your
fiancé (e) is detected HIV negative and the
doctor/counsellor advises you so that you
decide responsibly. Of the following decisions which one
will you more likely make?
|
1. Marry her/him but abandon childbearing
(permanent contraception) and +protected sex
(condom use) all the time
|
2. Marry her/him but abandon childbearing
(permanent contraception),adopt children +
protected sex (condom use) all the time
|
DMPOSNG
|
|
3. Marry if my partner accepts, limit childbearing with strict
and continuous prevention of mother-to-child transmission of HIV for all
pregnancy and breastfeeding.
|
4. Break up of engagement/marriage
relationship.
|
|
5. None of them, I will still marry her/him , have unprotected
sex and bear children irrespective of all advices, because I love her/him and
marriage is for the best and the worst.
|
6. Other
|
8. NK
|
50. Assuming that after a premarital examination you and your
fiancé(e) are both found to
be HIV positive and the doctor/counsellor advises you so
that you decide responsibly.
Of the following decisions which one will you more likely
make?
|
1. Marry her/him but abandon childbearing
(permanent contraception) and +protected sex
(condom use) all the time
|
2. Marry her/him but abandon childbearing
(permanent contraception),adopt children +
protected sex (condom use) all the time
|
DMPOPOS
|
|
3. Marry if my partner accepts, limit childbearing with
strict and continuous prevention of mother-to-child transmission of HIV for
all pregnancy and breastfeeding.
|
4. Break up of engagement/marriage
relationship and search/choice of
an other healthy partner
|
|
5. None of them, I will still marry her/him , have unprotected
sex and bear children irrespective of all advices, because I love her/him and
marriage is for the best and the worst.
|
6. Other
|
8. NK
|
51. What do you think about marriage between couples where one is
HIV positive and the
other HIV negative
|
1. It should be permitted only under certain protective
precautions given by the doctor/counsellor
|
2. It shouldn't be permitted
|
DMDISCO
|
|
3. No matter if the two fiancés agree to marry
|
4. No matters if the church/mosque agrees with this marriage
|
|
5. No matters if the parents/families of both
fiancés agree with this marriage union
|
6. Other:
|
8. NK
|
52. What do you think about marriage between two HIV positive
fiancés after a PCT?
|
1. It should be permitted only under certain protective
precautions given by the doctor/counsellor
|
2. It shouldn't be permitted
|
DMBHIHI
|
|
3. No matter if the two fiancés agree to marry
|
4. No matters if the church/mosque agrees with this marriage
|
|
5. No matters if the parents/families of both
fiancés agree with this marriage union
|
6. Other:
|
8. NK
|
53. What is your last word about HIV Premarital Counselling and
Testing (PCT) implementation in Kintampo?
_________________________________________________________________________________________
_________________________________________________________________________________________
END OF FORM. THANK THE RESPONDENT AND CHECK YOUR
FORM
ANNEX 2.a: INTERVIEW GUIDE FOR HEALTH CARE
PROVIDERS
KNOWLEDGE AND PERCEPTIONS TOWARDS PREMARITAL
COUNSELLING AND TESTING (PCT) ON HIV INFECTION AMONG UNMARRIED YOUNG ADULTS IN
KINTAMPO DISTRICT
|
Interview Date:_____/_____/05
Interview No:_______
Hospital/Health centre of: ___________________
_________________________________
Time opening IDI: :
Time End IDI: :
Interviewer:
Language Translator:.....................
|
|
My name is__________________________________. I am collecting
information on «Knowledge and perception towards premarital counselling
and testing (PCT) on HIV infection among unmarried young adult in Kintampo
District» with regard to the implementation of Voluntary counselling and
testing (VCT) services. All the information you give me will help the District
Health Authorities to successfully implement VCT and HIV PCT services in the
district. It will also be used for academic purpose. Responses will be treated
as confidential. This questionnaire will take not more than 30minutes. I need
your voluntary participation in this research interview. Do you have questions
before we start? Thank you for agreeing to participate in this study.
|
Designation of respondent being interviewed
|
NO
|
RESPONDENT
|
NO
|
RESPONDENT
|
|
1
|
Medical Doctor
|
4
|
Laboratory Technician
|
|
2
|
Matron
|
5
|
Medical counsellor
|
|
3
|
Nurse
|
6
|
Others, specify
|
1.Do you some times receive would-be couples for Premarital
Medical Counselling and Testing (PCT) in your hospital? Y/N
2. If yes to Q1 what is the approximate average
frequency?.............couples/individuals per Month/Trimester/year (Tick the
correct measure)
3.If yes to Q1 what medical lab exams do you do for them?
- - - - -
4. If no to Q1 why?
................................................................................................................................................
5.Are you already trained in medical marriage counselling and
testing? Y/N
6.Do you think HIV PCT should be institutionalized in Kintampo
as a core strategy to limit the spread of HIV/AIDS in new couples and their
children? Yes/No. Why?
7.Do you think HIV PCT should be compulsory or optional?? And
why???
8. If yes to Q1, who commonly send you fiancés for HIV
PCT?
9.How do they send you fiancés for HIV PCT?
10.Among the following mains steps of PCT what do you often
do?
11. If yes to Q1 what is the current cost of (HIV) PCT in
your hospital? Per individual or per couple?
................................................................................................................................................
12.Do you think this amount is affordable to Ghanaian in
Kintampo? Y/N. If No why?
13.How do you deal with the HIV PCT results?
a) In case of no problem found:
b) In case of discovery that one fiancé(e) is HIV
seropositive?
c) In case of discovery that both fiancé(e) are HIV
seropositive?
14.What do you take as position when you face a discordant
couple or a HIV/AIDS seropositive couple after a HIV PCT?
15.In case of a STI is found through PCT to one or both
fiancés what do you decide about the marriage process?
16.Do you deliver a prenuptial medical certificate (marriage
licence) to the fiancés after (HIV) PCT? Y/N and why?
17. How often would you like the HIV PCT to be set before
marriage and why?
................................................................................................................................................
18.In your opinion what barriers can prevent young unmarried
people from undergoing HIV PCT in Kintampo?
- -
19. What existing opportunities (enabling factors) in the
society today can make easier the implementation of HIV PCT in Kintampo
district?
- -
20. Given barriers to HIV PCT (Q 18) and enabling factors to
HIV PCT (Q 19), is HIV PCT implementation workable and feasible in Kintampo
district? Why?
21. What ways/means should be used in order to promote HIV PCT
in Kintampo?
- -
22. In your opinion what should be done so that unmarried
young Ghanaian people have easier access to attend HIV PCT in Kintampo?
23. What do you suggest for the HIV PCT practice to be more
effective, acceptable and attractive for unmarried young Ghanaian people in
Kintampo?
- -
24. What do you think about marriage between HIV discordant
couple (one partner is seropositive, the other still seronegative) or HIV
seropositive fiancés after a PCT?
25. In case of marriage between discordant couples or HIV
infected couples, those couples should be given certain precautionary measures
such as permanent condom use, limitation of childbearing or prevention of
mother-to-child transmission (PMTCT) measures (e.g. Nevirapine,
breastfeeding....) so that they protect themselves and children.
a) Do you think those couples can permanently
be able to practice them all their life long? Yes /No and why?
......................................................................................................................................................
b) Can one rely on the ability of couples to practices those
measures all their life long? Yes/No why?
......................................................................................................................................................
c) Is the application of these permanent measures truly
workable and feasible? Yes/No and why?
......................................................................................................................................................
d) If no to Q c, what should rather be done?
26. What difficulties or challenges do you often encounter in
your hospital during PCT in general and HIV PCT in particular?
27.What do you suggest to the following bodies in order to
solve these difficulties/challenges?
|
A) To the government/MOH
B) To the churches/mosques
C) To the registry officer
D) To the traditional/customary chiefs
E) To the parents
|
F) To the fiancés
G) To the Ghanaian people, especially young people
H) To the health system, hospitals and health care workers
I) To Others:.....................................
|
28.Your last word about HIV PCT implementation in Kintampo
district?
End.
ANNEX 2b: IN-DEPHT INTERVIEW GUIDE FOR RELIGION LEADERS
|
|
KNOWLEDGE AND PERCEPTIONS TOWARDS PREMARITAL
COUNSELLING AND TESTING (PCT) ON HIV INFECTION AMONG UNMARRIED YOUNG
ADULTS
IN KINTAMPO DISTRICTS
|
|
Interview Date:_____/_____/05
Interview No:_______
Interviewer:..............................
Translator:.....................................
Religion:_____________
Church or Mosque :________________________
Time opening IDI: :
Time End IDI: :
|
|
My name is__________________________________. I am collecting
information on «Knowledge and perception towards premarital counselling
and testing (PCT) on HIV infection among unmarried young adult in Kintampo
District» with regard to the implementation of Voluntary counselling and
testing (VCT) services. All the information you give me will help the District
Health Authorities to successfully implement VCT and HIV PCT services in the
district. It will also be used for academic purpose. Responses will be treated
as confidential. This questionnaire will take not more than 30minutes. I need
your voluntary participation in this research interview. Do you have questions
before we start? Thank you for agreeing to participate in this study.
|
1. Do you think the church or mosque has a major role to play
towards the control of the spread of HIV-AIDS in the general population and
would-be couples particularly? Yes/No
Why? What role should the church play?
2.What actions does your church and mosque carry out in the
fight against HIV-AIDS?
3. According to you, do those actions have a positive impact
towards the reduction of the spread of HIV-AIDS in the area?
4.What of the following preventive measures does your church
or mosque support in the fight against HIV-AIDS? And why?
|
Measures
|
Yes
|
No
|
Why?
|
|
Sexual abstinence
|
|
|
|
|
Faithfulness
|
|
|
|
|
Condom promotion/use
|
|
|
|
|
STI/HIVScrening,VCT,HIV PCT
|
|
|
|
5.Do you think people respect all the preaching the church or
mosque support towards the reduction of the spread of HIV-AIDS in the area?
Yes/No Why?
6.How many marriage do you celebrate on average in your church
or mosque during a month/year?................/month/year.(statistics needed
)
7.What activities does your church or mosque conduct when
preparing young adults who are about to enter into marriage? Do you tell them
about HIV PCT? Yes No
8.Are you already trained in medical marriage guidance
counselling and testing? Y/N
Is there any church/mosque elder who is trained? Y/N
9.Does your church or mosque require HIV Premarital Medical
Counselling and Testing (PCT) for all your church/mosque members who are about
to enter into marriage? Yes/No , Why?
10. If yes to Q 9, is HIV PCT compulsory/optional in your
church/mosque? Yes No and why?
11.If yes to Q 9,what is the average
frequency?.............Month/Trimester/year (statistics needed if possible)
12.If yes to Q 9, for what purpose do you send would-be
couples for PCT to the hospital?
13. How do you commonly send fiancés for PCT to the
hospital ?
14.How do you deal with the HIV PCT results?
a) In case of no problem found:
b) In case of discovery that one fiancé(e) is HIV
seropositive?
c) In case of discovery that both fiancé(e) are HIV
seropositive?
15.What do you take as position when you face a discordant
couple or a HIV/AIDS seropositive couple after a HIV PCT?
16.Do you require would-be couples to present a prenuptial
medical certificate (marriage licence) before the church/mosque can publicize
and celebrate their weddings? Y/N and why?
17. How often would you like the HIV PCT to be set before
marriage and why?
18.In your opinion what barriers can prevent young unmarried
people from undergoing HIV PCT at the Hospital?
19. What existing opportunities (enabling factors) in the society
today can make easier the implementation of HIV PCT in Kintampo district.
20. Given barriers to HIV PCT (Q 18) and enabling factors to HIV
PCT (Q 19), is HIV PCT implementation workable and feasible in Kintampo
district? Why?
21. What ways/means should be used in order to promote HIV PCT in
your church/Mosque and in Kintampo society?
22. In your opinion what should be done so that unmarried young
people have easier access to attend HIV PCT in Kintampo?
23. What do you suggest for the HIV PCT practice to be more
effective, acceptable and attractive for young adults in Kintampo society? :
24. What do you think about marriage between HIV discordant
couple (one partner is seropositive, the other still seronegative) or HIV
seropositive fiancés after a PCT?
25. In case of marriage between discordant couples or HIV
infected couples, those couples should be given certain precautionary measures
such as permanent condom use, limitation of childbearing or prevention of
mother-to-child transmission (PMTCT) measures (e.g. Nevirapine,
breastfeeding....) so that they protect themselves and children.
a) Do you think those couples can permanently be
able to practice them all their life long? Yes /No and why?
b) Can one rely on the ability of couples to practices those
measures all their life long? Yes/No why?
c) Is the application of these permanent measures truly workable
and feasible? Yes/No and why?
d) If no to Q c, what should rather be done?
26. What difficulties or challenges do you often encounter in
your church/mosque concerning PCT in general and HIV PCT in particular?
27.What do you suggest to the following bodies in order to
solve these difficulties/challenges?
|
A) To the government/MOH
B) To the churches/mosques
C) To the registry officer
D) To the traditional/customary chiefs
E) To the parents
|
F) To the fiancés
G) To the Ghanaian people, especially young people
H) To the health system, hospitals and health care workers
I) To Others:.....................................
|
28.Your last word about HIV PCT implementation in Kintampo
district?
END!
ANNEX 3: FOCUS GROUP DISCUSSION GUIDE
(FGDG)
KNOWLEDGE AND PERCEPTIONS TOWARDS PREMARITAL
COUNSELLING AND TESTING (PCT) ON HIV INFECTION AMONG UNMARRIED YOUNG
ADULTS
|
Date:_____/_____/05
FGD Specification:.........................
Time opening FGD: :
Time End FGD: :
Moderator________________
Note-Taker:...................................
|
|
My name is__________________________________. I am collecting
information on «Knowledge and perception towards premarital counselling
and testing (PCT) on HIV infection among unmarried young adult in Kintampo
District» with regard to the implementation of Voluntary counselling and
testing (VCT) services in the District in the near future. All the information
you give me will help the District Health Authorities to successfully implement
VCT and HIV PCT services in the district. It will also be used for academic
purpose. Responses will be treated as confidential. This questionnaire will
take not more than 2 hours. I need your voluntary and active participation in
this research discussion. Do you have questions before we start? Thank you for
agreeing to participate in this study.
|
|
NB: Remember to:
§ To brief focus group members on the research topic so
that they understand the nature and the aim of the discussion.
§ Introduce yourself and the purpose of the
recorder/photograph taking
§ Rule for discussion
§ Let participants introduce themselves
§ Ask for consent of participants for recording the
discussions
§ Tell participants that the information will be kept
with confidentiality and erased after the study.
§ Tell participants that their participation is
voluntary and that no allowance will be paid
§ Tell participants that they are free to use any
language (Twi or English).
|
1. What are some of the factors pushing younger children to have
sex before marriage in Kintampo district? Can this be prevented? If yes how? If
no why?
2. a) Is HIV/AIDS a real disease killing young people in Kintampo
district? Y/N How, give examples if possible?
b) What do you think is the effect of HIV/AIDS on the right and
freedom of people towards marriage today ??
c) What should be done to limit the spread of HIV/AIDS among
would-be couples who are about to enter into marriage?
3. Must young people consider «Health status» as a
core criteria when they choose their marriage partner? why?
4. a) How is marriage organized in K'po district and what is the
place of PCT in the marriage process in K'po?
b) Do you agree with this way of doing things?
c) Is HIV PCT currently being done in Kintampo district?
d) If yes is HIV PCT being currently conducted systematically
and in a very effective way?
e) If no Why is HIV PCT not being currently conducted in
Kintampo district?
5. Do you believe HIV Premarital Counselling and Testing (PCT) is
important (beneficial)? Why?
6. a) Should HIV PCT be institutionalized in the
country/society/churches? Why?
b) Should HIV PCT be compulsory or optional and why?
7. Do you believe that families, parents and peers should support
or encourage their younger children to perform HIV PCT before getting married?
Why?
8. In your opinion, who should send would-be couples to the
hospital for HIV PCT?
9. In your opinion, how often would you like the HIV PCT to be
set before marriage and why?
10. What are some barriers which can prevent young unmarried
people from going for HIV PCT services in Kintampo district?
11. What existing opportunities (enabling factors) in the society
today can make easier the implementation of HIV PCT in Kintampo district.
12. Given barriers to HIV PCT (Q 10) and enabling factors to HIV
PCT (Q 11), do you think HIV PCT implementation is workable and feasible in
Kintampo district? Why?
13. What ways/means should be used in order to promote HIV PCT in
Kintampo district?
14. What should be done so that unmarried Ghanaian young people
have easier access to HIV PCT services in Kintampo district?
15. What do you suggest for the HIV PCT practice to be more
effective, acceptable and attractive for young adults in Kintampo district?
16. What do you think about marriage between discordant couples
(one would-be couple is HIV infected) and HIV infected couples (both are HIV
infected) in Ghana and Kintampo? Should such marriage be allowed or forbidden?
And why?
17. In case of marriage between discordant couples or HIV
infected couples, those couples should be given certain precautionary measures
such as permanent condom use, limitation of childbearing or prevention of
mother-to-child transmission (PMTCT) measures (e.g. Nevirapine,
breastfeeding....) so that they protect themselves and children.
a) Do you think those couples can permanently be
able to practice them all their life long? Yes /No and why?
b) Can one rely on the ability of couples to practices those
measures all their life long? Yes / No why?
c) Is the application of these permanent measures truly workable
and feasible? Yes/No and why?
d) If no to Q c, what should rather be done?
END!
ANNEX 4. DESCRIPTION OF VARIABLES UNDER STUDY
(Source: The researcher).
|
N° of the
Question*(*)
|
Variables
|
Definitions
|
Scale of measurement
& Scoring scale
|
|
A
|
BACKGROUND VARIABLES
|
|
1
|
Sex
|
The biological state of being male or
female
|
-Female:2
-and male:1
|
|
2
|
Educational level
|
Nature and level of studies done by the
respondent
|
None, Primary, JSS,SSS,Tertiary
|
|
3
|
Religion
|
systems of faith that are based on the belief in
the existence of a particular god or gods that the respond belongs
to
|
Christian, Moslem, Traditionalist and
others
|
|
4
|
Tribe (Ethnic group)
|
Ethnic group or class of people to which the
respondent belongs to
|
1.Akan 2.Mo3.Gonja/Dagomba
4.Konkomba/Basare 5.Frafra,
6.etc.
|
|
5
|
Age
|
Number of birth days the respondent will have had
by the time the survey is conducted
|
Age in years
-Age group:15-19
years,20-24,25-30
|
|
6
|
Profession
|
Category of profession that the respondent belongs
to.
|
1.Farmer,2. Gvnmt workers
3.Trader,4.Students/Pupils,5.Others
|
|
7
|
Place of Residence
|
Place where the respondent lives
|
Urban: 2
Rural:1
|
|
B
|
|
PREMARITAL SEX HISTORY
|
|
|
8
|
-Rate of premarital sex
|
Those who will have had premarital sex the day of interview
|
Yes/No
|
|
9
|
Age at first sex
|
Age when respondent had first sex (sexarche)
|
Age at first sex,Normal: >=18 year
Abnormal:<18 year
|
|
10
|
Sexual partners before marriage
|
Any sexual partners with who respondent had had sex before
marriage
|
N0 of partners
Normal: 0-1, Abnormal: >1
|
|
C
|
GENERAL KNOWLEDGE ON STI, HIV/AIDS, VCT AND HIV
PCT
|
|
11-25
|
Level of general knowledge on HIV PCT
|
Knowledge revealed in answering on questions 11-25 assessing
knowledge on HIV PCT
|
-Yes/No, -Yes: score 1-2, -No: score o
-Expected score: 22
-Good Knowledge: Mean score =11 (11-16.5: Average,
>16.5=Adequate)
Poor Knowledge: Mean score < 11
|
|
11
|
Knowledge of any young adults HIV/AIDS sick person.
|
The respondent knows of any HIV/AIDS sick person
|
Know: Yes = score 1
Don't know: No or NK= score 0
|
|
12
|
Knowledge of unprotected premarital sex as risk factor to
STI/HIV/AIDS
|
The respondents knows that unprotected premarital sex is a
risk factor to STI/HIV/AIDS
|
Know: Yes = score 1
Don't know: No or NK= score 0
|
|
13
|
Knowledge on mother-to-child transmission of HIV
|
The respondent knows that the HIV could be transmitted from
the mother to her child
|
Know: Yes = score 1
Don't know: No or NK= score 0
|
|
14
|
Knowledge on the Cure of HIV/AIDS
|
The respondent knows that there is not yet any effective Cure
of HIV/AIDS .
|
Know: Yes = score 1
Don't know: No or NK= score 0
|
|
N°
Question*
|
Variables
|
Definitions
|
Scale of measurement
& Scoring scale
|
|
15
|
Knowledge on safety of sexual unions and marriages
|
The respondent knows that not all marriages are safe
|
Know: No = score 2
Don't know: Yes or NK= score 0
|
|
16.
|
Knowledge of factors/diseases making some sexual unions and
marriages unsafe.
|
The respondent knows factors/diseases making some sexual
unions and marriages unsafe.
|
Know: score 1 or 2, 1.HIV/AIDS: score 1
2.Other diseases: score 1, 3.Both 1 & 2: score 2, Don't
know: score 0
|
|
17
|
Consideration of good health status is a core criteria in the
choice of a fiancé(e)
|
The respondent knows that good health status is a core
criteria in the choice of a fiancé(e)
|
Know: Yes = score 2
Don't know: No or NK= score 0
|
|
18
|
Knowledge that PCT is the right mean to assess health status
of oneself and one's fiancé(e)
|
The respondent knows that PCT is the right mean to assess
health status of oneself and one's fiancé(e)
|
Options 1-4, Know: choose option 3 (PCT): score 2, Don't know:
choose any other option: score 0
|
|
19
|
Awareness on VCT.
|
The respondent is aware of VCT .
|
Have heard: yes, score 1
Have not heard: No, score 0
|
|
20
|
Awareness on HIV PCT
|
The respondent is aware of HIV PCT
|
Have heard: yes, score 1
Have not heard: No, score 0
|
|
21
|
Source of information on HIV PCT
|
The respondent know the source of information by which he
heard about HIV PCT.
|
1-9 different possible sources of information.
|
|
22
|
Knowledge that HIV PCT is a core measure to limit the spread
of HIV/AIDS in new couples
|
The respondent knows that HIV PCT is a core measure to limit
the spread of HIV/AIDS in new couples
|
Know: Yes = score 2
Don't know: No or NK= score 0
|
|
23
|
Knowledge of any person/couple who underwent HIV PCT
|
The respondent knows of a person/couple who underwent HIV
PCT
|
Know: Yes = score 1
Don't know: No or NK= score 0
|
|
24
|
Knowledge on who are the beneficiaries of HIV PCT
|
The respondent knows who are the beneficiaries of HIV PCT
|
Right answer: both fiancés, score 1
Wrong: any other answer, score 0
|
|
25
|
Knowledge of the major advantage of HIV PCT
|
The respondent knows of the major advantage of HIV PCT
|
-Know: adv1= score 2, adv 2= Score 1
adv 4= Score 1, Total score=4
-Don't know: No or NK or 3=score 0
|
|
D
|
|
PERCEPTION TOWARDS HIV PCT
|
|
|
26-40
|
Perception of respondents towards HIV PCT.
|
The way respondents understand and consider HIV PCT.
|
-Yes /No questions;-Yes: score 1-2
-No: score 0, -Expected score:23
-Positive perception: Score =11.5 (11.5-17.5=average,
>17.5=Adequate)
-Negative perception: score < 11.5
|
|
26
|
Risk perception of oneself/one's fiancé(e) to HIV
infection
|
The respondent perceives that he/she and or his/her
fiancé(e) are at risk to be HIV infected
|
-Perceive (yes): score 2
-Don't perceive (no): score 0
|
|
27
|
Perception of severity of HIV/AIDS
|
The respondent perceives the severity of HIV/AIDS which is a
fatal disease that does not have any effective drug yet.
|
-Perceive (yes): score 1
-Don't perceive (no): score 0
|
|
28
|
Perceived threat of contracting HIV/AIDS in case one get
married to a infected HIV person when HIV PCT is not done.
|
The respondent perceives the threat of contracting HIV/AIDS in
case one gets married to a infected HIV person when HIV PCT is not done.
|
-Perceive (yes): score 2
-Don't perceive (no): score 0
|
|
29
|
Perception of benefit of HIV PCT
|
The respondent perceives the benefit of HIV PCT which is
reducing the risk of contracting HIV/AIDS in new couples
|
-Perceive (yes): score 2
-Don't perceive (no): score 0
|
|
N°
Question*
|
Variables
|
Definitions
|
Scale of measurement
& Scoring scale
|
|
30
|
Perceived self control over HIV PCT action
|
The respondent perceives self control over HIV PCT action.
(S)He feels competent to decide her/him self to undergo HIV PCT)
|
-Perceive (yes): score 2
-Don't perceive (no): score 0
|
|
31
|
Perception that family members could approve HIV PCT action
|
The respondent perceives that his/her family members support
HIV PCT action.
|
-Perceive (yes): score 1
-Don't perceive (no): score 0
|
|
32
|
Perception that peers could approve HIV PCT action
|
The respondent perceives that his/her peers support HIV PCT
action.
|
-Perceive (yes): score 1
-Don't perceive (no): score 0
|
|
33
|
Perception that HIV PCT should be institutionalized
|
The respondent perceives that HIV PCT should be made and
become part of an organized system, society or culture, so that it is
considered as a social normal.
|
-Perceive (yes): score 2
-Don't perceive (no): score 0
|
|
34
|
Perception of respondents whether HIV PCT should be compulsory
or optional
|
The respondent perceives that HIV PCT should be compulsory or
optional
|
-option 1 :compulsory: score 1
-Option 2: optional: score1
-NK or NA: score 0
|
|
35
|
Perception of barriers to HIV PCT
|
The respondent perceives barriers to HIV PCT and find that HIV
PCT benefits outweigh these barriers
|
Yes or no: score 1
Don't know : score 0
|
|
36
|
Types of eventual barriers to HIV PCT.
|
The respondent gives some types of eventual barriers to HIV
PCT
|
Yes/No per type of barrier
|
|
37
|
Preference of respondents to undergo HIV VCT for marital reason
or not
|
The respondent gives his/her preference to undergo HIV VCT for
marital reason or not
|
-Preference to do VCT outside marriage: score 1;
-Preference to do HIV PCT: score 1
-preference of both HIV VCT and HIV PCT: score 2
- NK or None of them: score 0
|
|
E
|
|
PERCEPTION OF THE NEED OF HIV PCT SERVICES
|
|
|
38
|
Perception of the need of HIV PCT services
|
The respondent perceives the need of HIV PCT services
|
Perceive (yes): score 2
Don't perceive (no): score 0.
|
|
F
|
|
WILLINGNESS TO UNDERGO HIV PCT
|
|
|
39
|
Willingness for respondents to undergo HIV PCT
|
The respondent says S(he) will undergo HIV PCT with his/her
fiancé(e) when he/she will be about to marry
|
Willingness (yes):score 2
Unwillingness (no): score 0
|
|
G
|
|
READINESS TO KNOW AND ACCEPT HIV PCT
RESULTS
|
|
|
40
|
Readiness to know and accept HIV PCT results.
|
The respondent is ready to know and accept HIV test result
after a PCT session.
|
Ready (yes):score 2
Not ready (no): score 0
|
|
H
|
KEY SUGGESTIONS FROM CLIENTS TOWARDS A VERY EFFECTIVE
AND ACCEPTABLE HIV PCT PROGRAM/POLICY
|
|
41-47
|
Key Suggestions from clients towards a very effective,
accessible and acceptable HIV PCT program/Policy
|
Respondents suggest certain recommendations for HIV PCT
services to be more effective, accessible, attractive and acceptable to
them.
|
-Yes / No
-Suggestion to be considered: suggested by = 50% of
respondents.
-Suggestion may not be considered: suggested by = 50% of
respondents
|
|
41
|
Suggestion on the number of HIV PCT needed before marriage.
|
The respondent gives the number of HIV PCT sessions he/she
think is needed.
|
6 different options:
- once, -Twice, -At least once
-Dependence to length of marriage period
-More than 2 sessions, -Others - NK
|
|
N°
Question*
|
Variables
|
Definitions
|
Scale of measurement
& Scoring scale
|
|
42
|
Suggestion of the person who should send would-be couples for
HIV PCT.
|
The respondent suggests the person who should send would-be
couples for HIV PCT
|
9 options: 11-18, 88 (see questionnaire)
|
|
43
|
Suggestion of the person to whom clients think the HIV test
results should be communicated to after HIV PCT
|
The respondent suggests the person to whom the HIV test results
should be communicated to after HIV PCT
|
9 options 11-18, 88
(see questionnaire)
|
|
44
|
Suggestion of different ways/means to be used in order to
promote HIV PCT in the district.
|
The respondent suggests different ways/means to be used in
order to promote HIV PCT in the district
|
14 options
(see questionnaire)
|
|
45
|
Suggestion of different ways/means to be used in order to have
easier access to HIV PCT in the district
|
The respondent suggests different ways/means to be used in
order to have easier access to HIV PCT in the district
|
7 options
(see questionnaire)
|
|
46
|
Suggestion of different ways/means to be used in order to make
HIV PCT more effective, acceptable and attractive to youth in the district
|
The respondent suggests of different ways/means to be used in
order to make HIV PCT more effective, acceptable and attractive to youth in the
district
|
25 options with Yes/No
(see questionnaire)
|
|
I
|
|
COST OF HIV PCT SERVICES
|
|
|
45.1
and
46.20
|
Recommendation that HIV PCT services should be provided at
affordable or free costs.
|
The respondent says HIV PCT services should be provided at
affordable or free costs.
|
Recommend (yes)
Don't recommend (no)
|
|
J
|
PERCEIVED NEED OF CONFIDENTIALITY AND PRIVACY REGARDING
HIV PCT RESULTS
|
|
46.18
|
Perceived need of confidentiality and privacy regarding HIV PCT
results
|
The respondent perceives the need of confidentiality and
privacy regarding HIV PCT results
|
Perceive (yes)
Don't perceive (no)
|
|
47
|
Facility(ties) clients think HIV PCT service should be
established
|
The respondent suggests facility(ties) in which he/she thinks
HIV PCT service should be established
|
18 options
(see questionnaire)
|
|
K
|
POSSIBLE DECISIONS RESPONDENTS COULD MAKE ABOUT
MARRIAGE GIVEN HIV PCT RESULTS
|
|
48-50
|
Possible decisions respondents could make about marriage given
HIV PCT results
|
The respondent gives possible decisions he/she is more likely
to make about marriage given HIV PCT results in 3 different scenarios
|
-7 options
-Decision to be considered: predicted by = 50% of
respondents.
-Decision may not be considered: predicted by = 50% of
respondents
|
|
51-52
|
Point of view of would-be couples about marriage between HIV
discordant couple/HIV positive couple
|
Respondent gives his/her position about marriage between HIV
discordant couple and between HIV positive couple
|
7 options
|
|
53
|
Last word about HIV PCT implementation in K'po district.
|
The respondent gives his/her last word about HIV PCT
implementation in K'po district
|
Open-ended
|
* Code : The last right columns
contain field names (codes) that will be used in data entry and analysis.
* * For every uneducated
respondent who does not remember his/her age, the interviewer can look at
him/her and estimate his/her age group.
* ** ab: Reserved to
be completed by the researcher him self.
* ** Reserved to be completed by
the researcher him self.
* * No of the
question refers to the corresponding question in the questionnaire (Annex
1).
| 


