|
CLINICAL, RADIOLOGICAL AND THERAPEUTIC ASPECTS OF THE
LUMBAR DISC HERNIATION OPERATED IN CENTRAL AFRICA (DRC/ INSHASA)
Frederick Tshibasu Tshienda MD1, Jean
Mukaya Tshibola MD PhD1, Emmanuel Ndoma Kabu MD PhD 1,
Michel Lelo Tshikwela MD PhD1 , Jean Marie Mbuyi Muamba MD
PhD2.
1. 1Division of Diagnostic Imaging, University
Hospital of Kinshasa, School of Medicine, University of Kinshasa, Kinshasa,
Democratic Republic of Congo
2. Department of Internal Medicine, Division of
Rheumatology, University Hospital of Kinshasa, School of Medicine, University
of Kinshasa , Kinshasa, Democratic Republic of Congo
Corresponding author:
Frederick Tshibasu
Tshiendafredtshibasu@gmail.com
ABSTRACT
Objectives:Showing the clinical and
radiological aspects of the lumbar disc herniation operated in hospital
environments of Kinshasa then establishing the link between radiology and
surgery results.
Materials and methods:Retrospective and
documentary study of 160 cases of lumbar disc herniation operated in Biamba
Marie Mutombo hospital over 4 years: from January, 2012 till December,
2016.Taking advantage of the fact that among 160 Computed Tomography Scans (CT
scans) of the 160 patients, 48 patients have also effectuated Magnetic
Resonance Imaging Scans (MRI scans), a data sheet allowed the collection of
clinical, radiological and surgical data.
Results: The mean age of patients is 44,
7#177;12, 3 years. The most interesting age group range from 31 to 50 years
(68, 8%). Females were the most affected with 55.6%. Housewives were more
affected with 35.6%. Sciatica L5 was found in 28.8% of cases, sciatica S1 in
15.6% and left lateralization in 48, 1%. As for imaging results, the
posterolateral type was the most common with 53.8% of cases.The disc level:
L4-L5 was the most affected in 61.1% of cases.The single lumbar disc herniation
was the most common. The discrepancy between imaging and surgery results was
6.3% for medial herniated discs and 24.4% for posterolateral disc
herniation.
Conclusion: Lumbar disc herniation is a
pathological reality in hospitals of Kinshasa. The aspects
found mainly corroborate literature observations, except for some environment
peculiarities. The discrepancy between imaging and surgery results was
statistically insignificant.
Keywords: disc herniation- Sciatic- Magnetic
Resonance Imaging- Computed Tomography scan
I. INTRODUCTION
Lumbar Disc Herniation (LDH) is a major public health issue
around the world [1], whose disabling low back pain, whether associated or not
with sciatica, is the clinical expression [2]. It is defined as an overflowing
focal disc containing, in addition to the annulus fibrosus, the nucleus
pulposus, migrated from its central position to the periphery, roughly
associated with the cartilaginous elements of plateaus, marginal listella and
inflammatory reaction tissue in the presence of nucleus pulposus [3]. According
to the World Health Organization (WHO), LDH causes 15% of absenteeism in force
workers [1]. In France, low back pain is the most common reason for consulting
in rheumatology with around 26% of hospitalized patients and 30% of outpatients
[4].In the US, 50 to 90% of Americans have low back pain that causes serious
work disabilities and LDH is responsible for 1 to 30% of low back pain (or
subjects or cases to avoid repetition) [5, 6].The incidence of LDH varies from
one country to another. In Burkina Fasso and Mali, there are, respectively, 47%
and 23.6% of cases [7, 8]. While in Ivory Coast and Tunisia, the rate is quite
low at 10.3% [9] and 2.2% [10], respectively.In theDemocratic Republic of the
Congo, observations made in Kinshasa by Mukuna in 1990 and Kutoloka in 2002
reported respectively 2.3 and 4.3 patients per year [11, 12]. Nzanzu in 2011
reported a rate of 26.4% [13]. It should be noted that until 2005, the only
scanner available at University Clinics in Kinshasa presented some difficulties
in terms of functioning [11, 12].LDH is certainly a reason for absenteeism from
work and the alteration of quality of life because of the professional
incapacity it provides. The WHO reports a rate of 15% of absenteeism from work
among forced laborers, demonstrating its economic impact in terms of
productivity [1, 2]. Its financial impact is dramatic in the industrialized
countries, then all the more so in low-income countries such as the Democratic
Republic of the Congo.In France, there are approximately 37000 surgical
procedures per year for disc herniation [4, 14]. In England, the financial
impact would be in the range of 16 to 50 billion U.S. dollars [15]. However, it
should be noted that upstream of any surgical sanction, medical Imaging
thrones, useful in the diagnostic confirmation. This is the opportunity to
wonder about the regulatory role of surgical decisions, played by medical
imaging? This is all the more relevant because, to the best of our knowledge,
no prior study has so far defined the relevance of medical imaging in the
management of lumbar disc herniation operated in hospitals in Kinshasa. In view
of this impact, we propose to meet the following objectives:
Main objective: Describe the clinical,
radiological and therapeutic aspects of LDH operated in hospitals in
Kinshasa.
Specific objectives:To determine the
sociodemographic characteristics of patients who undergone surgery forLDH,
Describe the triggers of LDH, locate the most affected intervertebral discs,
highlight the type and subtype of the operated LDH, analyze the biological
profile in the operated LDH and compare the results of the imaging before the
surgery to the intraoperative result of the LDH.
II.MATERIALS AND METHODS
It was a retrospective and documentary study conducted from
January 2012 to June 2017, a period of four and a half years. The study was
mono-centric and involved patients who received hernia treatment at Biamba
Marie Mutombo Hospital (BMMH). The study population consisted of records of
patients operated for Lumbar Disc Herniation, each having a sectional imaging
examination (CT or MRI). The sample was exhaustive and included all patients
undergoing Lumbar Disc Herniation.The study included any patients of Congolese
nationality, male or female, aged at least 15 years, operated on for Lumbar
Disc Herniation and with a medical record containing the desired variables of
interest.This study does not include patients with incomplete medical records.
Any patient operated on LDH outside the study period or in another hospital
institution or any patient before surgery on LDH, was not included in this
study.
To carry out this work, the following materials were used:
patient files, collection cards and data entry materials including statistical
software. Each file included a consultation sheet containing the information
sought.A pre-established data collection sheet was used to transcribe all data
for each patient. It included the parameters or study variables. As for the
data collection, it was carried out in two stages: the first stage consisted in
the search of the cards and the second stage consisted in the data
transcription on the card of collection of the data.A Dell computer equipped
with software: Epidata 3.1, SPSS version 21, Excel and Word 2010 was used for
data entry and analysis.The following variables were included in each data
sheet: socio-demographic characteristics (age, sex and origin of the patient),
clinical parameters (weight, height, hernia installation wayand trigger factor
for Lumbar Disc Herniation),Para clinical parameters (laboratory tests,
standard radiography, CT scan and MRI results), classification of lesions
according to level, number, type and subtype of LDH.The intraoperative result
as well as the intraoperative incidents and complications.Quantitative
variables were expressed as mean, standard deviations or median with extremes
and qualitative variables as a percentage. The Pearson chi-square test was used
in the comparison of the qualitative variables. The materiality threshold was
set at 0.05. The odd ratio (95% confidence interval) had studied the risk
existing between the variables. The results are presented in the form of tables
and figures.The principle of confidentiality was rigorously observed when
collecting, entering and analyzing data using anonymity. No manifestation of
any conflict of interest has been brought to our attention.
As operational definitions:
Ø Age was expressed in years, patients were grouped by
10-year age groups, conventionally.
Ø The body mass index (BMI) is the weight-to-height
ratio squared ( ), expressed in kilograms per square meter ), expressed in kilograms per square meter . .
· weight loss: 
· normal: 
· overweight: 
· obesity: 
Ø The admission delay was the period between the date
on which the LDH diagnosis was made on imaging and the date on which the
patient had undergone hernia repair. This period was divided into age groups:
1-7 months, 8-16 months and ? 16 months.
Ø Provenance, defined the various institutions of
origin of the operated patients.
Ø "Paralyzing" and "paresiante" sciatica was defined
as lumbar pain radiating to the lower limbs responsible for deficit of the
levator or flexor foot.
Ø The hyperalgesic sciatica defined an intense
radicular pain, causing insomniaand hardly relieved by morphine.
Ø Sciatica + having the cauda equine syndrome defined
pain related to the compression of the other lumbosacral roots with sphincter
disorders such as incontinence and anesthesia in saddle or hemi-saddle.
Ø Alternating sciatica and bilateral sciatica defined
bilateral synchronous or successive radicular pains.
Ø L3 sciatica defined radiculalgiaon the anteromedial
aspect of the thigh and then stopping at the inner side of the knee.
Ø L4 sciatica, defined the radicular pain on the
anterior aspect of the thigh, the leg and which stops on the kick.
Ø L5 sciatica, defined the root pain on the
posterolateral side of the thigh, external side of the leg, bypassing the
external malleolus and stopping at the big toe.
Ø S1 sciatica defined the radicular pain in the
posterior aspect of the buttock, thigh, leg, heel, and plantar surface of the
foot which stops at the small toe.
Ø Disc herniation, defined as a focal discal overflow
containing, in addition to the annulus fibrosus, nucleus pulposus, migrated
from its central position towards the periphery associated with the
cartilaginous elements of the plateau, the marginal listel and the inflammatory
reaction tissue to the presence of the nucleus pulposus.
Ø Sub-ligamentous disc herniation: protrusion of disc
material under LVCP. The sub-ligamentous migrated disc herniation: sliding of
the disc material between the LVCP and the vertebral body, adopting a
descending or ascending path.
Ø Extra ligamentous disc herniation: it is a protrusion
of the disc material with rupture of the LVCP.
Ø Excluded disc herniation: defined by the presence of
a disc material having lost all connection with the rest of the nucleus
pulposus and migrated into the spinal canal at a distance from its floor (or
level).
Ø The median disc herniation: protrusion of the disc
material in the medial part of the vertebral canal or in zone A. It is less
common (10%).
Ø Posterolateral disc herniation: protrusion of the
disc material in the paramedian part of the vertebral canal or in zone B. It is
the most common (80%).
Ø The foraminal disc herniation: it is a localization
of the disc material within the foramen of conjugation. It is very rare.
Ø Extraforaminal disc herniation: it is a localization
of the disc material outside the foramen of conjugation. It is very rare.
Ø The inflammatory balance sheet: divided into normal
and disturbed, was considered as disrupted when one of the exams (VS, CRP)was
elevated beyond normal values.
III. RESULTS
SOCIO-DEMOGRAPHIC CHARACTERISTICS
OF PATIENTS
SEX OF PATIENTS
The sample in this study includes 160 patients' files, 89 of
which are women (55.6%) and 71 are men (44.4%) with a sex ratio M/W of 0.8 (see
figure 1).
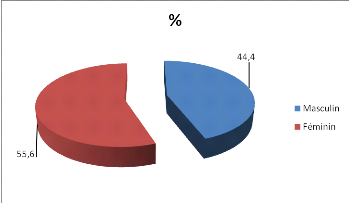
Figure 1: Distribution of patients by gender
Figure 1 shows a slight feminine predominance
COMPARED DISTRIBUTION
BETWEEN AGE AND GENDER
The average age of our patients
was 44.7 #177; 12.3 years with extremes ranging from 16 to 79 years. The
youngest was 16 years old while the oldest was 79 years old.The table below
illustrates comparative representation by sex and age group.
Table I: Distribution of patients by age and sex
|
Age group
|
Gendre
|
Total
|
|
Male
|
Female
|
|
Number of patients
|
%
|
Number of patients
|
%
|
Number of patients
|
%
|
|
=30
|
3
|
4,2
|
5
|
5,6
|
8
|
5,0
|
|
31 - 40
|
26
|
36,6
|
29
|
32,6
|
55
|
34,4
|
|
41 - 50
|
19
|
26,8
|
36
|
40,4
|
55
|
34,4
|
|
51 - 60
|
11
|
15,5
|
11
|
12,4
|
22
|
13,8
|
|
61 - 70
|
10
|
14,1
|
7
|
7,9
|
17
|
10,6
|
|
=71
|
2
|
2,8
|
1
|
1,1
|
3
|
1,9
|
|
Total
|
71
|
100,0
|
89
|
100,0
|
160
|
100,0
|
This table indicates that age groups from 31 to 50 years were
the most represented (68.8%).
PROFESSION
The distribution by occupation indicated that there were
employees, unemployed persons and persons practicing the liberal profession
(see Table II).
Table II. Distribution of patients by profession
|
Profession
|
Number of patients
|
%
|
|
Household
|
57
|
35,6
|
|
Civil servants
|
44
|
27,5
|
|
Accountants
|
20
|
12,5
|
|
Tradespeople
|
15
|
9,4
|
|
Mechanics
|
14
|
8,8
|
|
Nurses
Other (student)
|
9
1
|
5,6
0,625
|
|
Total
|
160
|
100,0
|
The distribution by occupation indicates that housewives were
the most attacked by the disease.
ORIGIN
The study also focused on patient origins. The table below
presents a summarization.
Table III. Distribution of patients according to their
origins
|
Origin
|
Numberof patients
|
%
|
|
National Electricity Company
|
53
|
33
|
|
University Clinics of Kinshasa
|
25
|
15,6
|
|
Commercial Banks of the Congo
|
23
|
14,4
|
|
Management Sciences for Health (MSH)
|
17
|
10,63
|
|
Biamba Marie Mutombo Hospital
|
15
|
9,4
|
|
Kinshasa Medical Center (CMK)
|
14
|
8,8
|
|
United Nations Observer Mission for the Stabilization of Congo
(MONUSCO)
|
13
|
8,1
|
|
Total
|
160
|
100,0
|
The majority of patients come from the National Electricity
Company with a percentage of 33%.
ANTHROPOMETRIC CHARACTERISTICS OF
PATIENTS
BODY MASS INDEX (BMI)
The study of the body mass index
gave rise to the results reported in the table below.
Table IV. Patient distribution according to BMI
|
BMI
|
Number of patients
|
%
|
|
Weight loss
|
4
|
2,8
|
|
Normal
|
38
|
23,5
|
|
Overweight
|
55
|
34,3
|
|
Obesity
|
63
|
39,4
|
Table IV indicates that the majority of patients (39.4%) were
obese.
CLINICAL PARAMETERS
*. TRIGGERING FACTORS
Figure 2 below describes the triggers for lumbar disc
herniation in this study.

Figure 2. Patient Distribution by Triggering Factors
Reading this figure indicates that in most cases, the
triggering factor was unknown. However, the uplift effort was the main
triggering factor in this study with 16.3%.
* INSTALLATION MODE
Table V below shows the various
installation modes of lumbar disc herniation.
Table V. Distribution of patients according to the mode
of installation of the herniated disc
|
Mode of installation
|
Number of patients
|
%
|
|
Sharp
|
40
|
25,0
|
|
Progressive
|
71
|
44,4
|
|
unspecified
|
49
|
30,6
|
Table V shows that 71 patients (44.4%) had a progressive mode
of installation.
* ADMISSION delay
The median time from diagnosis to actual patient
hospitalization for hernia cure was 17.5 days. This period was divided into age
groups: 1-7 months, 8-16 months and ? 16 months. Table VI below gives a
summarization.
Table VI. Distribution of patients according to the
admission delay
|
Admission delay (months )
|
Number of patients
|
%
|
|
1 - 7
|
143
|
89,4
|
|
8 - 16
|
15
|
9,4
|
|
?16
|
2
|
1,3
|
It can be seen from this table
that 89.4% of patients were admitted within 1 to 7 months and 1.3% were more
than 16 months old. The median admission time was 17.5 days.
*. RADICULAR PATH
The analysis of the various root paths is summarized in
Table VII.
Table VII. Distribution of patients by root path
|
Root paths
|
Number of patients
|
%
|
|
L5
|
|
|
|
- Left
|
23
|
14,4
|
|
- right
|
15
|
9,4
|
|
- Bilateral
|
8
|
5,0
|
|
S1
|
|
|
|
- Left
|
12
|
7,5
|
|
- right
|
8
|
5,0
|
|
- Bilateral
|
5
|
3,1
|
|
Poorly systematized
|
|
|
|
- Left
|
35
|
21,9
|
|
- Right
|
20
|
12,5
|
|
- Bilateral
|
9
|
5,6
|
|
Truncated
|
|
|
|
- Left
|
7
|
4,4
|
|
- Right
|
3
|
1,9
|
|
- Bilateral
|
5
|
3,1
|
|
Cruralgia
|
10
|
6,3
|
Table VII indicates that the left side was the most affected.
Poorly systematized lumbosciatica were the most common with 64 cases (40.0%),
while 10 patients (6.3%) had cruralgia.
CLINICAL EXAMINATION
*. SPINAL SYNDROME
Limitation of spinal mobility
Table VIII. Distribution of patients according to
spinal mobility
|
Hand-ground distance in cm
|
n=140
|
%
|
|
< 30
|
24
|
17,1
|
|
31 - 50
|
35
|
25
|
|
51+
|
81
|
57,9
|
The following table shows that in
57.9% of patients, the hand-to-ground distance was limited to 51 cm and
more.
*. RADICULAR SYNDROM
Lasègue's sign
Table IX below illustrates the distribution of patients
according to the Lasègue's sign.
Table IX. Patient distribution according to the
Lasègue sign
|
Lasègue's sigh
|
Number of patients
|
%
|
|
ipsilateral
|
|
|
|
<45
|
60
|
37,5
|
|
>45
|
50
|
31,25
|
|
contralateral
|
25
|
15,625
|
|
Absent
|
13
|
8,125
|
|
Bilateral
|
12
|
7,5
|
The sign of Lasègue was
present in 66, 75%, absent in 8,125% and bilateral in 7, 5% of cases.
NEUROLOGICAL SYNDROM
Sensitivity balance sheet
Table X below shows the distribution of patients
according to the sensitivity examination.
Table X. Distribution of patients by sensitivity
examination
|
Variable
|
Number of patients
|
%
|
|
Normal
|
120
|
75,0
|
|
Hypoesthesia
- L5
- S1
|
|
|
|
13
12
|
8,1
7,5
|
|
Anesthesia
- L5
- S1
|
10
|
6,3
|
|
5
|
3,1
|
The table above shows that
sensitivity was normal in 75% of patients and disrupted in 25%.
Motricity (or traction) balance sheet (or records)
Table XI below reports the distribution of patients
according to the motricity (or traction) examination.
.Table XI. Distribution of patients according to the
examination of motricity
|
Motricity
|
Number of patients
|
%
|
|
Normal
|
81
|
50,6
|
|
Paresis
|
35
|
21,9
|
|
Paralysis
|
34
|
21,3
|
|
Cauda equina syndrome
|
10
|
6,3
|
Table XI above shows that motor skills (motricity)
were normal in 50.6% and disrupted in 49.4%.
COMMON SCIATICS AND LDH REBELS TO
MEDICAL TREATMENT.
Table XII below illustrates the various clinical
situations that may require a hernia cure. Among the 160 patients, there are 51
cases of hernias that are resistant to medical treatment. Table XII gives a
distribution according to their clinical manifestations or etiological
diagnosis.
Table XII. Distribution of patients according to
clinical forms and LDH rebels to medical treatment
|
Clinical forms and LDH rebels to medical treatment
|
|
|
|
Number of patients
|
%
|
|
hyperalgic
|
|
|
|
80
|
50,0
|
|
paralytic
|
|
|
|
19
|
11,9
|
|
Cauda equina syndrome
Herniated discs rebel to medical treatment
|
|
|
|
10
51
|
6,3
31,9
|
Table XII shows that the hyperalgic form was the most
encountered in this series.
PARACLINIC FOCUS
*. INFLAMMATORY balance sheet (records) AND
HEMOGRAM
All patients had performed the laboratory examinations
mentioned above. The distribution of these various results is shown in Table
XIII
Table XIII. Distribution of patients according to the
results of the inflammatory balance sheet and the hemogram
|
Number of patients
|
%
|
|
Inflammatory balance sheet
Normal
|
130
|
81,3
|
|
disturbed
|
|
|
|
· Increased CRP
|
20
|
12,5
|
|
· Accelerated VS
|
10
|
6,2
|
|
Complete blood count
|
|
|
|
· Normal
|
155
|
96,9
|
|
· Disturbed
|
5
|
3,1
|
It can be seen from Table XIII
above that no inflammatory marker is specific for LDH.
MEDICAL IMAGING
* Standard radiography
Standard X-rays were performed in all 160 patients, in
whom there were 32 common X-rays. This is summarized in Table XIV below:
Table XIV. Patient distribution according to the
results of standard radiography
|
X-ray
|
Number of patients
|
%
|
|
Normal
|
32
|
20,0
|
|
Disc pinching
|
95
|
59,4
|
|
Transitional anomalies
|
|
|
|
- Lombalization de SI
|
12
|
7,5
|
|
- Sacralization de L5
|
14
|
8,8
|
|
Lumbar spine rectitude
|
7
|
4,4
|
Table
XIV shows that disc pinching was the most common anomaly with 59.3%.
*Computed tomography (CT)
The previous herniated disc was not found in any
patient. All cases were of the posterior type as summarized in Table XV
below.
Table XV. Distribution of patients by type and subtype
of lumbar disc herniation at CT.
|
Imaging Diagnosis
|
Number of patients
|
%
|
|
Herniation type
|
Sub-type
|
|
|
|
Anterior hernia
|
-
|
-
|
-
|
|
Posterior hernia
|
|
|
|
|
- Median hernia
|
80
|
50,0
|
|
- Posterolateral hernia
|
85
|
53,1
|
|
- Foraminal hernia
|
5
|
3,1
|
|
- Extraforaminal hernia
|
5
|
3,1
|
This table shows that the median
and posterolateral hernias were predominant in the proportions of 50% and
53.1%, respectively.
Nuclear Magnetic Resonance Imaging
Among 160 patients, 48 (30.0%) patients had an MRI examination
in addition to CT. Figure 2 below shows the distribution. Among these 48
patients, 47.9% had posterolateral DH, 33.3% had a median DH, and 18.8% had a
foraminal hernia.

Figure 2. Distribution of MRI findings of the lumbar spine.
This figure confirms once again that the foraminal subtype is
rare, as in the CT scan.
ANATOMICAL AND TOPOGRAPHIC DISTRIBUTION OF LESIONS
Table XVI below illustrates the distribution according
to the number and disc level concerned.
Table XVI. Distribution of patients by number and level
of disc level affected
|
Number of discfloors
|
Level of disc floors
|
Number of patients
|
%
|
|
Unique
|
L4 - L5
|
55
|
34,4
|
|
L5 - S1
|
35
|
21,9
|
|
Total
|
90
|
56,3
|
|
Double
|
L3 - L4, L4 - L5
|
10
|
6,3
|
|
L4 - L5, L5 - S1
|
45
|
28,1
|
|
Total
|
55
|
34,4
|
|
Triple
|
L3 - L4, L4 - L5, L5 - S1
|
15
|
9,4
|
Table XVI shows that multiple
localization is quite common in our environment.
ASSOCIATED PATHOLOGIES
Figure 3 below shows the pathologies associated with
hernia in this study.

Figure 3. Pathologies associated with operated lumbar
disc herniation.
Figure 3 indicates that hypertrophy of the yellow
ligament was frequently associated with lumbar disc herniation (62.5%).
STATISTICAL ANALYSIS
* RELATIONSHIP BETWEEN THE SUB-TYPES OF HERNIA AND
SEX
Table XVII represents a comparative study of the
subtypes of the encountered LDH and sex.
Table XVII. Cross representation between subtypes of
hernia and sex
|
Hernia sub type
|
Sex
|
P
|
OR (IC à 95%)
|
|
Male
|
Female
|
|
Median hernia
|
|
|
|
|
|
Yes
No
|
37 (52, 1%)
34 (37, 9%)
|
43 (48, 3%)
46 (51, 7%)
|
0,633
|
0,859 (0,460 - 1,604)
|
|
Posterolateral hernia
|
|
|
|
|
|
Yes
No
|
41 (57, 74%)
30 (42, 3%)
|
44 (49, 4%)
45 (50, 6%)
|
0,295
|
0,715 (0,382 - 1,381)
|
|
Foraminal hernia
|
|
|
|
|
|
Yes
No
|
1 (1, 4%)
70 (98, 6%)
|
4 (4, 5%)
85 (95, 5%)
|
0,265
|
3,294 (0,360 - 30,149)
|
|
Extraforaminal hernia
|
|
|
|
|
|
yes
No
|
2 (2, 8%)
69 (97, 2%)
|
3 (3, 4%)
86 (96, 6%)
|
0,841
|
1,203 (0,196 - 7,406)
|
Table XVII reveals that
there was no statistically significant relationship between subtypes and sex.
In contrast, the risk was 3 times higher in women with foraminal hernias and 1
time higher in men with extra foraminal hernias.RELATIONSHIP BETWEEN THE
SUBTYPES OF LDH AND THE LIFTING EFFORT AS A TRIGGER FACTOR.
The notion of lifting force as a triggering factor was
found in 16.3% of the patients. Below is the distribution of these cases
according to this triggering factor.
Table XVIII. Relationship between the subtypes of the
hernia and the effort of uplift.
|
Hernia subtype
|
Uplifting effort
|
|
|
|
Yes
|
No
|
P
|
OR (IC à 95%)
|
|
Median hernia
|
|
|
|
|
|
Yes
No
|
14 (53, 8%)
12 (46, 2%)
|
66 (49, 3%)
68 (50, 7%)
|
0,668
|
1,202 (0,518 - 2,790)
|
|
Posterolateral hernia
|
|
|
|
|
|
Yes
No
|
14 (53, 8%)
12 (46, 2%)
|
71 (53, 0%)
63 (47, 0%)
|
0,936
|
1,035 (0,446 - 2,444)
|
|
Foraminal hernia
|
|
|
|
|
|
Yes
No
|
25 (96, 2%)
1 (3, 8%)
|
130 (97, 0%)
4 (3, 0%)
|
0,817
|
1,300 (0,139 - 12,123)
|
|
Extraforaminal hernia
|
|
|
|
|
|
yes
No
|
0 (0, 0%)
26 (100, 0%)
|
129 (96, 3%)
5 (3, 7%)
|
0,317
|
0,963 (0,931 - 0,995)
|
Table XVIII indicates that there
was no statistically significant relationship between the subtypes and the
lifting effort. However, the risk was multiplied by 1.202 for median DH, 1.035
for posterolateral DH, and 1.300 for foraminal DH, respectively.
RELATIONSHIP BETWEEN THE SUBTYPES OF LDH AND
TRAUMATISM AS A TRIGGERING FACTOR.
The concept of trauma as a triggering factor was found in
11.9% of patients in our study. The table below summarizes its distribution.
Table XIX. Relationship between subtypes of hernia and
triggers (trauma)
|
Hernia subtype
|
Trauma
|
P
|
OR (IC à 95%)
|
|
Yes
|
No
|
|
Median hernia
|
|
|
|
|
|
Yes
No
|
4 (21, 1%)
15 (78, 9%)
|
76 (53, 9%)
65 (46, 1%)
|
0,255
|
1,901 (0,648 - 5,007)
|
|
Posterolateral hernia
|
|
|
|
|
|
Yes
No
|
10 (52, 6%)
9 (47, 4%)
|
75 (53, 2%)
66 (46, 8%)
|
0,963
|
0,978 (0,375 - 2,552)
|
|
Foraminal hernia
|
|
|
|
|
|
Yes
No
|
1 (96, 2%)
4 (3, 8%)
|
18 (97, 0%)
137 (3, 0%)
|
0,568
|
1,903 (0,201 - 17,976)
|
|
Extraforaminal hernia
|
|
|
|
|
|
yes
No
|
1 (96, 2%)
4 (3, 8%)
|
18 (97, 0%)
137 (3, 0%)
|
0,568
|
1,903 (0,201 - 17,976)
|
There is no statistically significant link between subtypes of
hernia and trauma. However, it should be noted that the risk was multiplied by
1.901 for the medial hernia, 1.903 for the foraminal hernia and 1.903 for the
extra foraminal hernia (Table XIX).
RELATIONSHIP BETWEEN THE SUBTYPES OF LDH AND SPORT AS
A TRIGGER FACTOR.
The concept of sport as a triggering factor was only found in
5.6% of the cases on our entire workforce. The table below summarizes its
distribution.
Table XX. Relationship between subtypes of hernia and sport
|
Hernia subtype
|
Sport
|
|
|
|
Yes
|
No
|
p
|
OR (IC à 95%)
|
|
Median hernia
|
|
|
|
|
|
Yes
No
|
0 (0, 0%)
9 (100, 0%)
|
80 (53, 0%)
71 (47, 0%)
|
0,002
|
0,470 (0,397 - 0,557)
|
|
Posterolateral hernia
|
|
|
|
|
|
Yes
No
|
8 (88, 9%)
1 (11, 1%)
|
77 (41, 0%)
74 (51, 0%)
|
0,027
|
7,688 (0,938 - 62,935)
|
|
Foraminal hernia
|
|
|
|
|
|
Yes
No
|
0 (0, 0%)
9 (100, 0%)
|
5 (3, 3%)
146 (96, 7%)
|
0,579
|
0,967 (0,939 - 0,996)
|
|
Extraforaminal hernia
|
|
|
|
|
|
yes
No
|
0 (0, 0%)
9 (100, 0%)
|
5 (3, 3%)
146 (96, 7%)
|
0,579
|
0,967 (0,939 - 0,996)
|
The median and posterolateral DH had a statistically
significant relationship with the sport with p = 0.002 and p = 0.027,
respectively. The risk was multiplied by 7.688 in the posterolateral hernia
(Table XX).
RELATIONSHIP BETWEEN THE SUBTYPES
OF LDH AND HYPERTROPHY OF YELLOW LIGAMENT AS AN ASSOCIATED PATHOLOGY.
Hypertrophy of the yellow ligament was the most
predominant associated pathology at 62.5%. Table XXI summarizes its
relationship with the various subtypes.
Table XXI. Relationship between subtypes of hernia and
hypertrophy of ligament.
|
Hernia subtypes
|
Hypertrophy of the yellow ligament
|
P
|
|
No
|
Yes
|
|
Number of patients
|
%
|
Number of patients
|
%
|
|
Median
Yes
No
|
7
|
61,7
|
43
|
43,0
|
0,022
|
|
23
|
38,3
|
57
|
57,0
|
|
Posterolateral hernia
|
|
|
|
|
|
|
Yes
No
|
15
|
25,0
|
60
|
60,0
|
?0,001
|
|
45
|
75,0
|
40
|
40,0
|
|
Foraminal hernia
|
|
|
|
|
|
|
Yes
No
|
60
|
100,0
|
95
|
95,0
|
0,078
|
|
0
|
0,0
|
5
|
5,0
|
|
Extraforaminal hernia
|
|
|
|
|
|
|
yes
No
|
55
|
91,7
|
100
|
100,0
|
0,003
|
|
5
|
8,3
|
0
|
0,0
|
Table XXI shows that three subtypes of posterior LDH had a
statistically significant relationship with hypertrophy of the yellow ligament:
p = 0.022 (median DH), p = 0.001 (posterolateral DH), p = 0.003 (extraforaminal
DH).RELATIONSHIP BETWEEN THE SUB-TYPES AND LOMBARTHROSIS
AS ASSOCIATED PATHOLOGY
The study sought to establish the link between subtypes of LDH
and lumbar spondylosis, which was present in 34.4% of the cases. This is well
illustrated in the table below.
Table XXII. Relationship between subtypes of hernia and
associated pathologies (lumbar spondylosis)
|
Hernia subtypes
|
LOMBARTHROSIS
|
P
|
|
No
|
Yes
|
|
Number of patients
|
%
|
Number of patients
|
%
|
|
|
Median hernia
Yes
No
|
62
|
59,0%
|
18
|
32,7%
|
0,002
|
|
43
|
41,0%
|
37
|
67,3%
|
|
Posterolateral hernia
|
|
|
|
|
|
|
Yes
No
|
45
|
42,9%
|
30
|
54,5%
|
0,159
|
|
60
|
57,1%
|
25
|
45,5%
|
|
Foraminal hernia
|
|
|
|
|
|
|
Yes
No
|
100
|
95,2%
|
55
|
100,0%
|
0,100
|
|
5
|
4,8%
|
0
|
0,0%
|
|
Extraforaminal hernia
|
|
|
|
|
|
|
yes
No
|
100
|
95,2%
|
55
|
100,0%
|
0,100
|
|
5
|
4,8%
|
0
|
0,0%
|
Table XXII shows that there is a statistically significant
relationship between the posteromedial subtype and lumbar spondylitis with a
value of P equals to 0.002.
RELATIONSHIP BETWEEN THE SUB-TYPES AND THE Lumbar spinal
stenosis AS ASSOCIATED PATHOLOGY
The Lumbar spinal stenosiswas found as an associated
pathology in 21.9% of cases. Table XXIII below illustrates the relationship
with the various subtypes.
Table XXIII. Relationship between the subtypes of the
hernia and the Lumbar spinal stenosis
|
Hernia subtypes
|
Lumbar spinal stenosis
|
P
|
|
No
|
yes
|
|
Number of patients
|
%
|
Number of patients
|
%
|
|
|
Median hernia
|
|
|
|
|
|
|
Yes
No
|
61
|
48,8
|
19
|
54,3
|
0,566
|
|
64
|
51,2
|
16
|
45,7
|
|
Posterolateral hernia
|
|
|
|
|
|
|
Yes
No
|
60
|
48,0
|
15
|
42,9
|
0,590
|
|
65
|
52,0
|
20
|
57,1
|
|
Foraminal hernia
|
|
|
|
|
|
|
Yes
No
|
120
|
96,0
|
35
|
100,0
|
0,229
|
|
5
|
4,0
|
0
|
0,0
|
|
Extraforaminal hernia
|
|
|
|
|
|
|
yes
No
|
120
|
96,0
|
35
|
100,0
|
0,229
|
|
5
|
4,0
|
0
|
0,0
|
We conclude from the table XXIII that there is no
statistically significant link between the Lumbar spinal stenosis and the
different subtypes.
RELATIONSHIP BETWEEN DIAGNOSIS OF MEDICAL IMAGING AND
INFLAMMATORY BALANCE SHEET
A relationship between the result of the inflammatory
balance sheet and the various subtypes of LDH has been sought. Table XIV below
generates a summarization.
Table XXIV. Imaging diagnosis and results of
inflammatory balance sheet
|
Imaging diagnosis
|
Inflammatory balance sheet
|
Total
|
P
|
|
disturbed
|
Normal
|
|
Number of patients
|
%
|
Number of patients
|
%
|
Number of patients
|
%
|
|
|
Median hernia
|
10
|
5,7
|
70
|
40,0
|
80
|
45,7
|
?0,001
|
|
Posterolateral hernia
|
15
|
8,6
|
70
|
40,0
|
85
|
48,6
|
|
Foraminal hernia
|
5
|
2,8
|
0
|
0,0
|
5
|
2,8
|
|
Extraforaminal hernia
|
0
|
0,0
|
5
|
2,8
|
5
|
2,8
|
|
Total
|
30
|
17,1
|
145
|
82,9
|
175
|
100,0
|
|
Table XXIV indicates that the inflammatory balance was only
disturbed in 30 of the 160 patients. A statistically significant link was noted
between the result of the imaging and the result of the inflammatory balance
sheet (p = 0.001).
MANAGEMENT
All 160 patients underwent laminectomy with hernia
repair. Table XXV below reports the concordances and discrepancies found
between the diagnosis of imaging and the intraoperative results.
Table XXV. Comparative illustration between the
diagnosis of imaging and the intraoperative results.
|
diagnosis of imaging
|
intraoperative diagnosis
|
n/%
|
P
|
|
Median hernia
|
Posterolateral hernia under ligament
|
5 (6,3)
|
<0,001
|
|
|
Medial hernia under ligament
|
75 (93,7)
|
|
|
Total
|
80 (100,0)
|
|
Posterolateral hernia
|
Bony outgrowth compressing the roots
|
1 (1,2)
|
<0,001
|
|
|
Ejected posterolateral hernia
|
5 (5,8)
|
|
|
Posterolateral hernia under ligament
|
60 (69,8)
|
|
|
Ejected median hernia
|
10 (11,6)
|
|
|
Median hernia under ligament
|
10 (11,6)
|
|
|
Total
|
85 (100,0)
|
|
Foraminal hernia
|
Foraminal hernia
|
5 (100,0)
|
<0,001
|
|
|
Total
|
5 (100,0)
|
|
Extraforaminal hernia
|
Extraforaminal hernia
|
5 (100,0)
|
<0,001
|
|
|
Total
|
5 (100,0)
|
Table XXV shows that the
discrepancies between the imaging results and the intraoperative results were
of the order of 6.3 and 24.4% concerning the medial and posterolateral disc
hernias respectively. A statistically significant link was noted between
subtypes of LDH and intraoperative diagnosis (p?0.001).
DISCUSSION
The clinical and para clinical profile of the Congolese from
Kinshasa suffering from lumbar disc herniation is that of a female individual
(55.6%), aged on average 44.7 #177; 12.3 years, obese (39.4%), complaining
mainly of lumbosciatic L5 (28.8%), more lateralized on the left (14.4%),
triggered by the lifting effort and whose neurological disorders were marked by
hypoesthesia and anesthesia respectively at (8, 1 et 7, 5%), associated with
motor disorders (49.4%).Conventional X-ray was pathological in 80.0%, CT in
100% and MRI in 30.0% of operated patients.The analysis of the results revealed
statistically significant links (69.3%) respectively between the medical
imaging results and the intraoperative results, then (82.9%) between the LDH
subtypes and the results of the inflammatory balance sheet. This led us to
point out some peculiarities of the environment, even if the study corroborates
the observations of the literature globally.
SOCIO-EPIDEMIOLOGICAL PROFILE
. The age
This study shows that 110 out of 160 patients (68.8%) were
aged between 31 and 50 years old. The mean age was 44.7 #177; 12.3 years with
extremes ranging from 16-79 years. LDH was overwhelmingly a pathology of young
adults. The latter would generally be exposed to heavy work, incriminated in
the pathogenesis of LDH. Our results are very close to those found in the
literature. Indeed, LDH lumbosciatica occur most often in young adults aged 30
to 50 years [16]. Some small variations were noted according to the series, but
most often, the age of the patients at the time of the diagnosis is 50 % of the
times between 36 and 55 years [17-18]. At CNHU Hubert Maga of Cotonou, Tononhi
studies showed an average age of 44.9 years [16]. Tchuindjang found that the
most affected age groups were between the ages of 31 and 60, with the
prevalence of the 41 to 50 age group and a median age of 45.6 years. Ouattara
had found a median age of 43.5 years with a predominant attack between 40 and
49 years. Kutoloka, in his series, found an average age of 48.4 years [12,
19].
The
sex
In this study the female predominance was found in 110 cases
(55.6%) out of a total of 160 patients, with a sex ratio of 0.8 in favor of the
woman. We believe that it is possible that the large participation of Congolese
women in the activities of survival pushes them to exert activities of effort
thus overloading their lumbar spine. The high number of maternity could also
play a role in lumbar spine imbalance.Our results would be close to those of
Bamako study in 2005 that found a female predominance with a sex ratio of
1.95.Unlike the study conducted in Burkina Faso where the sex ratio was 1.9 in
favor of men [8, 9].Our results are, on the other hand, in contradiction with
some data of the literature which are unanimous on the male predominance of the
herniated disc as well in Mali, in Africa or even in the world with a sex ratio
oscillating between 1.4 according to Diarra M and 1.9 according to Tchuintdjang
K [8, 20].
Profession
This study indicates that 57 out of 160 patients (35.6%) were
housewives. This category of the population is exposed to a sedentary life,
predisposing to develop obesity which is incriminated in the imbalance of
spinal biomechanics, because of the overload it imposes. Our observations
corroborate the data in the literature. Davis reports a higher prevalence of
LDH among sedentary people, without providing any application.This could be
explained either by obesity or by the accentuation of the early degeneration of
the disc by repeated trauma and micro trauma [22].It should be noted that
professional activity is criminalized in 36.6% of cases of forced or manual
workers and 26.7% of those in sedentary jobs [17, 23, and 24].Nevertheless, it
should be noted that, according to De Korvin et al, lumbosciatica affects all
professional sectors, that they make use of the muscles (20% of the handlers,
40% of the building workers and 40% of the caregivers) or that they are
sedentary (30% of women and 40% of men clerks) [4].
The origin
The majority of patients in the series, 53 patients or 33.1%
came from the National Society of Electricity. This can be explained by several
reasons: notably by an offer of care more granted to the National Society of
Electricity agents and their family members, the heavy work that some agents
face, not to mention the large number of the National Society of Electricity
agents who attend the hospital as part of their agreement with Biamba Marie
Mutombo Hospital.
Triggers
Uplifting effort was the most criminalized factor with 16.3%
of cases. It is a risk factor for both lumbosciaticaand lumbosciaticaon LDH
[17], concomitantly with other factors such as sports, trauma, prolonged
standing, cold, obesity and driving. . No statistically significant link was
noted between the subtype of the hernia and the lifting effort.
On the other hand, the risk was multiplied by 1,202 for the
medial hernia, 1,035 for the posterolateral hernia and 1,300 for the foraminal
hernia.The high incidence of this factor could also be explained by the fact
that the majority of patients in this series consisted of housewives who are
exposed to muscular efforts to provide for their families. Our data are close
to those of the literature: Deshayes and Mandour had also incriminated the
lifting effort in their series with respectively 38% and 49.1% of cases [25,
26]. This difference in percentages could be explained by the fact that in this
series the triggering factor was not specified in 66.3% of cases.
ANTHROPOMETRIC PARAMETERS OF PATIENTS
Body mass index (BMI)
In this series, obesity was found in 39.4% of cases. The
housewives were the most frequent professional category. This category of
people is subject to a sedentary life, exposing them to obesity that is one of
the triggers of the LDH [21]. Another reason is that the abdominal musculature
counterbalances the powerful action of the extensors. Its deficiency, its
distension in obese or pregnant women, as well as its inefficiency accentuate
lumbar lordosis, which, in turn, accelerates disc degeneration [21].
CLINICAL STUDY
Installation mode
This study showed that 71 patients (44.4%) had a progressive
mode of LDH installation. This could be explained by a high rate of
self-medication with analgesics and anti-inflammatories in our environment.It
should be noted that LDH sciatica are installed in two modalities: acute and
progressive. In the first, pains occur from the start in lightning, associated
with a more or less marked functional impotence. As for the second, it spreads
in a few days and follows a history of low back pain or lumbago.In this series,
acute onset was noted in 25% of cases. This is in accordance with the results
generated by Mandour and Lazorthes with 27.5% and 28% respectively [26, 27]. On
the other hand, the progressive start of the 44.4% recorded in this series was
far lower than the observations of Mandour and Deshayes, who reported
respectively 58.8% and 60% [25, 26]. This difference was probably due to the
fact that the installation method was not specified in our series in 49
patients (30.6%).
The admission period
The admission delay in this series ranged from 1-7 months in
143 patients (89.4%). This delay corresponds to the time elapsed between the
date when the diagnosis of disk herniation was made in imaging and the
hospitalization for a surgical cure for LDH. During this period, patients
consulted several doctors and received various therapeutics. The median
admission delay was 17.5 days in this series. This is probably due to the
terror that the surgical procedure caused in many people. In the different
series of the literature, the admission period ranges from one week to 10 years
with a maximum frequency between 1 month and 1 year [23]. Our results are close
to those of the literature on this point.
Mode of admission to the hospital
This study showed that 50.6% of patients were admitted to the
hospital in emergency, against 49.4% of patients admitted to hospital by
appointment. This is explained by the fact that the majority of patients
operated on (68.2%) had symptomatic forms of LDH hernia (the hyperalgic,
paralyzing, and Cauda equina syndromes), which were found in 50%, 11.9% and
6.3% of cases respectively, while the LDH rebels to medical treatment were
found in only 31.9% of cases.
The radicular path
The study of radicular path in our series showed a
predominance of poorly systematized lombosciatalgia in 46 cases (28.8%),
followed by L5 locations in 46 cases (28.8%) and S1 in 25 cases (15.6%). This
large number of poorly systematized lumbosciatalgia could be explained by the
fact that the neurological examinations were probably brief, carried out by the
general practitioners. The frequent attack of the L5 root could be explained by
the vulnerability of the root L5 with respect to the root S1, whose lesion can
evolve slowly for a long time before manifesting itself. Our data are in
agreement with the results of Mandour and Lazorthes [26, 28].The predominance
of lateralization on the left was noted in this series in 77 cases (48.1%)
compared to 46 cases (28.8%) in the right side. We have no explanation to give
in this regard.Bilateral sciatica was found in our series in 19.3% of cases. We
do not have a particular reason to provide against this observation.
Nevertheless, our data are close to the results of Gandin who reported 16% of
cases [29].
PHYSICAL EXAMINATION
Spinal syndrome
Low lumbar stiffness was assessed by hand-to-ground distance
in all patients,among which 116 patients (82.9%) had a distance greater than 30
cm. This rate was slightly higher than that reported by Mandour, accounting for
53.2% of cases [26].Lasègue's maneuver was the most explored gesture in
the neurological examination. It was noted in 147 patients (91.9%), 68.75% of
these patients are noted with an ipsilateral positive Lasegus, 15.625% with a
contralateral positive Lassec and 7.5% with a bilateral positive Lassec.
Indeed, following its impact on the nerve root, disc herniation, in most cases,
reduces the normal amplitude of root slip in the inter-disco-apophyseal parade
[30]. This is why it shows correlations with the degree of progression of LDH
[31]. For Klat M and Mbuyi M, the first degrees of the sign of Lasègue
are the most determining for the diagnosis of sciatica of disc origin [31]. A
Lasègue sign below 25 ° -30 ° indicates severe sciatica. When
the sciatic pain of the patient is reproduced by the elevation of the
contralateral lower limb, it is a contralateral Lasègue. At Gandin and
El Azhari the sign of Lasègue was positive in 75% and 87% respectively
[29, 32].
The neurological syndrome
Sensitivity study
In this series, these disorders were investigated in all
patients, 120 of these patients (75%) had normal sensitivity, 25 patients
(15.6%) had hypoesthesia, while anesthesia was found in 15 patients
(9,4%).Sensitivity disorders generally consisted of hypoesthesia, see,
superficial anesthesia in the L5 or SI territory (on the antero-external part
of the leg, the back of the foot and the big toe in case of L5 involvement and
On the Achilles' tendon, the heel, the sole of the foot when suffering from
SI).These sensitivity disorders were also found by Deshayes in 25% of cases and
by El Azhari in 42% of cases [25, 32].
Study of motricity
Segmental motricity function was evaluated in all patients in
this series. Eighty-one patients (50.6%) had no motor deficit, 35 patients
(21.9%) had paresis and 34 patients (21.3%) had complete paralysis. Our results
are in agreement with the observations of Dheshayes who reported paralytic
sciatica in 9.1% and paresiant sciatica in 23.9% [25]. Similarly Guieu reported
paralyzing sciatic in 10% and paresiant in 14% [33]. As for Brement, he had
reported 5.8% of paralytic sciatica and 10.8% of parasiant sciatica [34].
Clinical forms of common sciatica
Hyperalgic sciatica
It prohibits any spinal mobilization. The pain is
excruciating, not relieved by the decubitus. After radiological assessment and
when this pain does not give way under medical treatment, it can impose a
surgical intervention. In our series, hyperalgic sciatica was found in 80
patients (50% of all patients). Our results are close to those of the study of
Davis who found in his series 76% of hyperalgic forms [21].Nevertheless, our
observations were in contradiction with the data of Brement which had found a
frequency of 24, 16% [34]. Barhourhe, on a sample of 266patients? , found a
frequency of 25.93% [24]. This high rate of the hyperalgesic form explained why
nearly 50% of patients had an admission time of around 17.5 days.
Paralyzing forms
This form was observed in 19 patients (11.9%) of this series.
In general, paralytic sciatica presents itself first as a common or hyperalgic
sciatica and then, the pain disappears, leaving room for a brutal or sub-acute
motor deficit. This most often concerns the antero-external compartment of the
leg. In some cases, electromyography can quantify the motor impairment and
follow its evolution. Our observations are consistent with those of Guieu [33]
and Deshayes [34] who reported a frequency of 10% and 9.1% respectively.
Barhoure [24] had a frequency of 14.27%.
Cauda equina syndrom
This syndrome was noted in 10 patients (6.3%) of this series.
It translates a compression of the roots of the Cauda equina by a bulging
hernia, often in a postero median position. This syndrome is rare both in
literature and in our series. Our observations are close to Pierron's data [35]
which reported a frequency of 5.4%. As for Rafik [36], he reported a frequency
of 2.7%.
Forms depending on the age
Operated LDH remains rare in the elderly. Our series
identified 3 patients (1.9%) aged 71 years or older, including 2 men and one
woman. This could be explained by the fact that neurosurgeons and
anesthesiologists avoid taking risks because surgery and anesthesia at this age
remains very delicate. In children and adolescents, LDH was also rare. Our
series had noted a single case operated at the age of 16 years. Our results are
close to those of Rafik [36] and Mrabet [37] who reported respectively 1.1% and
3%.
PARACLINIC EXAMINATIONS
Biology
? Inflammatory balance sheet and hemogram
Our study shows that of the 160 patients, 130 patients
(81.3%) had a normal inflammatory balance sheets. Thirty patients (18.7%) had a
disturbed inflammatory balance, of which 12.5 with increased CRP and 6.2% with
accelerated VS. Note also that the blood count was disrupted in 3.1% of
cases.
A relationship has been sought between the inflammatory
balance and the different types of LDH. It follows that of the 80 cases of
median DH, 10 cases (5.7%) had a disturbed inflammatory balance. Similarly, of
the 85 cases of postero-lateral DH, 15 cases (8.6%) had a disturbed
inflammatory balance, whereas 5 out of 5 cases of foraminale DH had a disturbed
inflammatory balance. The study found a statistically significant relationship
between imaging diagnoses and inflammatory outcome (p = 0.001).
However, it should be noted that LDH is a degenerative
affection that does not positively influence the rate of sedimentation [34,
37]. It should be noted that accelerated VS and elevated CRP in some patients
in our study may be due to other conditions that were not likely to be
investigated or reported in the charts. Some authors also found high levels of
CRP in LDH [38]. According to the latter, the disc pathology is marked by a
systemic inflammatory response related to the degree of progression of the
herniated mass.
MEDICAL IMAGING
· Standard radiography
The results of standard radiography in this study had shown an
overall pinch of the disc in 95 patients (59.4%). The examination was normal in
32 patients (20%). Transitional abnormalities were found in 26 patients
(16.2%), whereas spinal rectitude was seen in 7 patients (4.4%). The standard
radiography is the first examination to realize before the failure of the
medical treatment. El Azhari [32] and Czorny [39] had also noted a global disc
narrowing respectively in 32% and 25% of cases.
· Computed tomography (CT)
Posterior LDH was found in 100% of patients in our series. The
median DH was observed in 80 patients (50.0%), posterolateral DH in 85 patients
(53.1%), foraminal DH in 5 patients (3.1%) and finally the extra foraminal
hernia also in 5 patients (3.1%).In our series, single disc herniation's were
frequently found in 90 cases (56.3%). Disc level L4 - L5 was the most highly
affected in 55 cases (34.4%). These results corroborate the work of Suk, Rompe,
Porchet, Kimn and Kutoloka [40]. The predominance of impairment at the L4-L5
level may be due to the fact that this disk is probably more constrained than
the L5-S1 stage.Double disc herniation's were found in 55 cases (34.4%) with a
predominance of discs L4 - L5 and L5 - S1 in 45 cases (28.1%). These last two
discs are the most mobile of the lumbosacral hinge, hence the predominance of
the attack on their levels. Triple disc herniation's were found in 15 cases
(9.4%) in L3 - L4, L4 - L5 and L5 - S1. Our results are consistent with those
of the literature for both disc stages and topography of lesions. In Destandau
[41], the stages (L3-L4, L4-L5 and L5-S1) were concerned in 15%, 51% and 25% of
cases, respectively. This confirms that the L4-L5 and L5-S1 disks are the most
affected because of the importance of the stresses and pressures exerted there
[42].Note that the first two disks: L1-L2 and L2-L3 were not affected in our
series.
· Magnetic resonance imaging (MRI)
In our series, 48 patients had benefited from the CT-lumbar
MRI pair, i.e. 30% of cases. We did not notice a discrepancy of results between
these two techniques. This can be explained by a small number of patients who
have done both exams at the same time. Which makes it impossible to draw
realistic conclusions.
ASSOCIATED PATHOLOGIES
Our series shows that hypertrophy of the yellow ligament was
the spinal pathology most commonly associated with lumbar disc herniation's in
62.5% of cases, followed by narrow lumbar canal in 21.9% of cases. Transitional
abnormalities and retrolisthesis were the least recovered in 6.2% of cases.A
statistically significant link was noted between the three subtypes of
posterior LDH and hypertrophy of the yellow ligament with p values 0.022
(median LDH), 0.001 (posterolateral LDH) and 0.003 (extraforaminal LDH),
respectively.The narrow lumbar canal can be primary or secondary. It seems that
fibrosis occurring during any herniated disc is at the origin of the formation
of osteophytes and hypertrophy of the facet joints, causing the compression of
bone structures still called primary structures. This is called the primary
narrow lumbar canal [2].The hypertrophy of the yellow ligament concerns only
the ligamentous structures of the rachis still called secondary structures.
Hence its name narrow secondary lumbar canal.Lumbar osteoarthritis is the most
common degenerative pathology. It constitutes more than a quarter of the
etiologies of lumbosciaticaaccording to the literature. This hypothesis has not
been confirmed in this series. Moreover, these three pathologies are
degenerative pathologies of the spine like herniated discs. This is why their
association is frequent. In addition, the transitional anomalies of the lumbar
hinge had a negligible percentage.
CONFRONTATION BETWEEN THE ADMISSION DELAY AND THE
SURGICAL ACT.
The surgical treatment of LDH had to be well qualified in some
cases. In this study, the notion of admission delay and its comparison with
literature data allowed us to identify three operative indication groups:
· A delay
of less than or equal to 7 months: 89.4% of patients operated on for surgical
emergencies, including hyperalgic sciatica, paresis, paralyzing sciatica and
Cauda equina syndrome. Our observations are consistent with those in the
literature, which report an admission period ranging from one week to 10 years
with a maximum frequency between 1 month and 1 year [23].
· Delay between 8-16 months: 9.4% of patients operated on
tramp sciatica who were resistant to medical treatment.
· A delay greater than or equal to 16 months: 1.3% of
patients operated for sciatics not amenable to medical treatment.
CONFRONTATION OF RESULTS FROM IMAGING TO RESULTS BY
OPERATIVES
- The confrontation of the results of the medical imaging
(CT-MRI) with those of the surgery of the LDH operated allowed to create the
following:
- With respect to median hernias, out of 80 cases, the study
found a discrepancy in results in 5 patients (6.3%).
- Regarding postero-lateral lumbar disc herniation, out of 85
operated cases, there was a discrepancy in 21 patients (24.4%).
- As for foraminal and extraforaminal hernias, the results
were confirmed by intraoperative imaging.
- The other point of disagreement was due to the fact that the
CT scanner was silent with the lumbar disc herniation ejected, which became
anxious intraoperatively.
The significant rate of discordance in posterolateral lumbar
disc herniation could be attributed to an error in the evaluation of the
various disc zones by the radiologist or simply to the following regression of
hernia volume in patients who received medical treatment based
anti-inflammatory before surgery. Note a statistically significant statistical
link established between the results of the imaging and the results per
operation with a value (p?0.001).
MERITS AND WEAKNESSES OF THE STUDY
To the best of our knowledge, this study is the first to be
conducted in a hospital in Kinshasa and to set the stage for a confrontation
between the radiological and intraoperative results of the LDH operated. This
would avoid unjustified surgical indications and insufficient diagnoses in
terms of imaging in our environment. However, we recognize that it has some
weaknesses including:
· The lack of precision of some clinical data in a larger
number of patients.
· The small number of patients who performed the MRI
examination
· The absence of a prospective study allowing the
re-reading of certain images of examinations carried out with a view to a
diagnostic requalification.
IV. CONCLUSION
The present study revealed the clinical, radiological and
therapeutic aspects of LDH operated in hospitals in Kinshasa. It allowed us to
compare the results of medical imaging with those of surgery.It turned out
that, LDH is the prerogative of young patients, 110 patients(68.8%) with a peak
between the age groups of 31 to 50 years.
A slight female predominance was observed in 89 cases, i.e.
55.6% with a sex ratio of 80 men per 100 women.The effort of uprising was more
incriminated as the triggerof the pathology disc. Sciatica L5 was more common
with lateralization preferentially on the left.Floors L4-L5 and L5-S1 were the
most affected. Posterolateral LDH was the most common subtype with 53.1%.The
discrepancy between the results of the imaging and those of the surgery was
statistically insignificant(6.3%) for median LDH and 24.4% for posterolateral
LDH.
REFERENCES
1. Organisation mondiale de la santé. Identification et
prévention des maladies liées à la profession:
série de rapports scientifiques. Genève, OMS 1995.
2. Mukaya J, Mbuyi J. La sténose rachidienne lombaire
de l'adulte congolais de Kinshasa : Radio-morphométrie des canaux.
Thèsed'agrégation, Université de Kinshasa 2017, pp 195.
3. Le Manuel du Résident.
Radiodiagnostic-Neuroradiologie-Appareil locomoteur. Edition
Tsunami 2009, pp 5244.
4. DE Korvin G, Blamoutier A .Orthopédie et
réadaptation: La hernie discale lombaire. http :
www.orthopédie-et-réadaptation.com/rachis/hernie discale
lombaire/2001;
5. Rasmussen C, Nielsen G, Hansen V. Rates of lumbar disc
surgery before and after implementation of multidisciplinary non surgical spine
clinics. Spine 2005;30:2469?2473.
6. Deyo R. Back surgery-who needs it? N Engl J Med.
2007;356:223?224.
7. Millogo A, Bamouni A, Taoko A et al. lombosciatiques :
profil radio clinique et étiologique au centre hospitalier
Bobo-Dioulasso (Burkina Faso) Rev Med Af Noire.1999 ; 46 :16-18.
8. Diarra M. Etude des pathologies neurochirurgicales
opérées dans le service d'ortho traumatologie de l'hôpital
Gabriel Touré de Novembre 2000 à novembre 2001 ; A propos de
106 cas. Thèse de médecine, Bamako 2002, pp250.
9. Kouakou N, Akissi N, Eti E et al. Données
épidémiologiques élémentaires sur la rhumatologie
en milieu hospitalier ivoirien. Rhumatologie 1994;46:239-42.
10. Younes M, Béjia I, Aguir Z et al. Prévalence
et facteurs associés à la sciatique commune dans une population
urbaine tunisienne. Rev Rhum. 2006;73: 927-931.
11. Mukuna B. La chirurgie vertébro-médullaire
de l'adulte aux cliniques universitaires de Kinshasa (230 observations).
Mémoire de spécialisation, Université de Kinshasa 1990, pp
75.
12. Kutoloka M. Aspects cliniques et thérapeutiques de
la hernie discale lombaire aux Cliniques Universitaires de Kinshasa .A
propos de 104 patients hospitalisés au Département de chirurgie
de 1966 à 1999 .Mémoire de Spécialisation,
Université de Kinshasa 2002,pp 84.
13. Nzanzu I. Profils clinique et tomodensitométrique
de la pathologie lombaire chez les congolais de Kinshasa. Mémoire de
spécialisation, Université de Kinshasa 2011, pp 78.
14. Sandjon. Coût de la prise en charge des malades
opérés dans le service de traumatologie et d'orthopédie du
CHU Gabriel Touré de Janvier à Juin 2003. A propos de 130 cas.
Thèse de médecine, Bamako 2004, pp 250.
15. http :
www.chirurgie_vertebrale.com/pathologies/HDLomb/hdlomb.html,
16. Tonnonhi C. Les hernies discales au CHU Hubert Maga de
Cotonou ; à propos de 78 cas. Thèse de médecine .Cotonou
2004 ; pp 25O
17. Berney J, Jean prêtre M, Kostli A et al. Facteurs
épidémiologiques de la hernie discale lombaire. Journal
neurochirurgie1990 ; 36 : 354-365.
18. Guyot-Drouot M, Cortet B, Delcamne B et al
.Spondylodiscites. Revue du praticien 1996 ; 10 :343.
19. Diomande M, Ouattara B, Eti E, et al .La hernie discale
lombaire au CHU de cocody (Abidjan): aspects épidémiologiques,
cliniques, radiologiques et thérapeutiques. Revue Cames sante 2013 ;
1:1-2.
20. Tcuindjang K. Aspects épidémiologique,
clinique et thérapeutique des hernies discales opérées
dans le service de traumatologie et d'orthopédie du CHU Gabriel Toure.
Thèse de médecine, Mali 2003, pp 250.
21. Davis R. Along-term outcome analysis of 984 surgically
treated herniated lumbar discs. Neurosurg. 1994 ; 80 :415-421.
22. Khoo L, Fessler R. Microendoscopic decompressive
laminotomy for the treatmentof lumbar stenosis. Neurosurgery 2002 ; 51:
146-154.
23. Zufferey P, Cedrashi C, Vischer T. Prise en charge
hospitalière chez des patients lombalgiques : Facteurs prédictifs
de l'évolution à deux ans. Revue Rhumatologie 1998 ; 65: 346-354.
24. Barhourhe O .Sciatique par hernie discale en milieu
militaire au service de neurochirurgie CHU Ibn Roch de casablanca. Thèse
de médecine, Casablanca 1996 ; pp 135.
25. Deshayes P, Baron J, Leloyet X et al. Résultats du
traitement médical en milieu hospitalier des sciatiques d'origine
discale. Revue de rhumatisme 1981;48: 7-9.
26. Mandour A. Les sciatiques par hernie discale au service de
neurochirurgie du CHP de Meknès ; à propos de 102 cas.
Thèse de Médecine, Casablanca 2000 ; pp 120.
27. Dreiser R, Maheu E, Ghozlan R et al. Etude
épidémiologique des stratégies diagnostiques et
thérapeutiques dans les lombalgies et dorsalgies subaiguës et
chroniques en médecine ambulatoire. Comparaison des attitudes en
médecine générale et en rhumatologie. Revue Rhumatologie
1997 ; 64 : 27-36.
28. Lazorthes Y, Richaud J, Roguer B et al. Sciatiques
chirurgicales et chimionucléolyse. Neurochirurgie 1985 ; 31: 471-493 .
29. Gandin J, Lamoureux G, Boye P et al. Bilan critique du
traitement chirurgical de 600 lombosciatiques : Orientation diagnostique et
thérapeutique. Chirurgie1982 ; 108: 311-321.
30. Kapandji I. Physiologie articulaire du tronc et du rachis.
Paris Maloine S.A. 1972 ; 100-127.
31. Klat M, Mbuyi M. Guide diagnostique en rhumatologie.
Kinshasa, La sève 1989 ; 250- 261.
32. El azhari A, El kamar A, Ouboukhlik A et al. La sciatique
paralysante par hernie discale. Rev. Mar. Méd. Sant. 1992 ; 14:39-41.
33. Guieu R, Roussel P, Sedan R et al. Réflexe
nociceptif de flexion de la jambe. La pressemédicale1996 ; 343 : 22.
34. Brement J. A propos de 120 sciatiques par hernie discale
opérées au service de neurochirurgie du Centre hospitalier
Chambéry. 1977 ; pp 78.
35. Pierron D, Fahim R, Halimi P et al. La place de l'examen
tomodensitométrique dans le diagnostic des complications de la chirurgie
discale lombaire. Journal de radiologie1985 ; 66 : 8-9.
36. Rafik M. Sciatique par hernie discale à propos des
180 cas. Thèse médecine ; Casablanca 1990 ; 215 :105 .
37. Mrabet H. Sciatique par hernie discale au CHU Ibn Rochd de
Casablanca à propos de 278 cas. Thèse de Médecine
Casablanca 1994 ; 262.
38. Kim NH. Anterior inter body fusion in the treatment of the
lumbar herniated nucleus pulposus. Yousei Med J. 1999 ; 40 : 256-264.
39. Czorny A, Forloudou P, Kilik C et al. Les hernies discales
lombaires de l'enfant ; à propos de 12 cas. Neurochirurgie 1988 ; 34:
389-393.
40. Renier J, Bregeon C. Autres manifestions douloureuses en
rapport direct ou indirect avec la détérioration discale lombaire
; Appareil locomoteur. Paris, EMC 1984 ; B-10 :15-840.
41. Weinstein J, Lurie J, Olson P. United States' trends and
regional variations in lumbar spine surgery 1992-2003.Spine 2006;31:270-271.
42. Deyo R, Mirza S. Trends and variations in the use of spine
surgery. Clin. OrthopRelat Res. 2006;443:139-146.
43. Cherkin D, Deyo R, Loeser J. An international comparison
of back surgery rates. Spine 1994;19:1201-1206.
44. Sandjon. Coût de la prise en charge des malades
opérés dans le service de traumatologie et d'orthopédie du
CHU Gabriel Touré de Janvier à Juin 2003. A propos de 130 cas.
Thèse de médecine, Bamako 2004, pp 250.
45. Ngongang O. Aspects épidémiologique et
étiologique des lombalgies au service orthopédique et
traumatologique de l'hôpital Gabriel Touré de Janvier à
Décembre 2003. A propos de 411 cas. Thèse de médecine,
Bamako 2004, pp 250.
46. Bagayoko N. Les lombalgies non
traumatiques dans le service de chirurgie orthopédique et
traumatologique de l'hôpital Gabriel Touré de Janvier 1998
à Août 1999. A propos de 106 cas. Thèse de médecine,
Bamako 2000, pp 250.
47. Hijikata .Percutaneous nucleotomy: a new concept technique
and 12 years expérience. ClinorthopedrelRess. 1989 ; 238 : 9- 23.
48. Laredo J, Wyber M, Bonneville J. La nucléotomie
percutanée. Feuillets de radiologie1990 ; 4 :30.
49. Destandau J. Aspects techniques de la chirurgie
endoscopique des hernies discales foraminales lombaires ; A propos de 191 cas.
Neurochirurgie 2004; 50 : 6-10.
50. Pinel B, Leloet X, Thomine J. Les radiculalgies
sciatiques foraminales à propos de 16 observations. Revue Rhumatologie
1983; 50 : 603-606.
51. Hajjaji-Hassouni N. Les sciatiques. Journal du praticien.
2002 ; 3 : 13-16.
52. Lodenet C. Les sciatiques par hernie discale à
propos de 354 cas. Thèse de Médecine ; Dijon 1978 ; pp 138.
53. Blond S, Armignes PH, Parker F. et al. Sciatalgies
chroniques par désafférentation sensitive après chirurgie
de la hernie discale lombaire: Aspects cliniques et thérapeutiques
à propos de 10 patients. Neurochirurgie 1991 ; 37: 86-95.
54. Lagarrigue J, Lazorthes Y, Verdie J et al. Analyse des
résultats de la chirurgie et de la nucléolyse à la
papaïne dans 1085 cas de hernies discales lombaires. Neurochirurgie1991 ;
37 :97-105.
55. Richard A, Davis M. A long out-come analysis of 984
surgically treated herniated lumbar discs. Neurosurgery 1994 ; 80.
56. Cofer. Les lomboradiculalgies des membres
inférieurs en rhumatologie. Paris, Masson 2000 ; 589-602.
57. Revel M, Loty B, Vallee C. Le traitement des
lomboradiculalgies. Editions Techniques, appareilLocomoteur. Paris, EMC 1994 ;
15-840 F 110 : 100.
58. Mankin H. Douleurs dorsales et cervicales. In T R
Harrison, Principes de Médecine Interne. Paris, Flammarion.
Médecine Science 1992 ; 5: 116- 124.
59. ANAE. Prise en charge diagnostique et
thérapeutique des lombalgies et lombosciatiques communes de moins de
trois mois d'évolution. Revue de chirurgie orthopédique et
réparatrice de l'appareil moteur 2000 ; pp 45.
|
|



