|
_
SCHOOL OF PUBLIC HEALTH
COLLEGE OF HEALTH SCIENCES
UNIVERSITY OF GHANA, LEGON
DEVELOPMENTOF A COMPUTERIZED PROVIDER ORDER ENTRY
SYSTEM FOR LABORATORY
BY
GERARD BISAMA MUTSHIPAYI
(10509422)
A PROJECT WORK SUBMITTED TO
THE SCHOOL OF PUBLIC HEALTH, COLLEGE OF HEALTH
SCIENCES, UNIVERSITY OF GHANA, LEGON, IN PARTIAL FULFILLMENT OF THE REQUIREMENT
FOR THE AWARD OF MASTER OF HEALTH INFORMATICS
JULY 2015
DECLARATION
I Gérard Bisama Mutshipayi the author of this
dissertation, do hereby declare that with the exception of references to the
literature and works of other researchers which have been duly cited the work
in this dissertation is the result of my original work.
Gérard Bisama Mutshipayi
........................................
(Student)
(Supervisor)
......................................
.................................................
Date: ......................... Date:
...........
DEDICATION
For my family, the reason I wrote this dissertation and the
raison I was able to. Francine Kukamba Kawesi, my lovely wife and Ethan
Mutshipayi Bisama, my son. My parents Alphonse Mutshipayi and Josée
Bakafua, I can barely find the words to express all the wisdom and support you
have given me.
This work is dedicated to you.
ACKNOWLEDGEMENT
I am very grateful to all individuals and groups who
contributed to making this study a successful one.
First and foremost, all my thanks to God. You have given me
the strength to believe in my passion and pursue my dreams. I could never have
done this without the faith I have in you, the Almighty.
A special thanks to my supervisor Mr. Seth K. Afagbedzi, for
his guidance, assistance and counsel. Without his continuous support and
assistance it would not have been possible to finish this dissertation.I also
thank all lecturers for the knowledge imparted to me.
Thanks to all MHI course mates for their contribution and
advices.
I would like to thank all my friends, especially Mary Anita
Quist, for her support in the academic work.Thanks to Patrick Tshibangu, my
friend, roommate and compatriot for listening, offering me advices.
Finally, we are extend our most sincere gratitude to the BEBUC
(Bourse d'Excellence Bringmannaux Universités Congolaise) scholarship
program and The Holger-Poehlmann-Foundation for supporting this master program
financially and morally, particular thanks to Prof. Gerhard Bringmann and Prof.
Mudugo Virima respectively the president and the vice-president of BEBUC. To
all members of the BEBUC panel I express also my gratitude.
1. ABSTRACT
The laboratory services play important role in health care
provision since it provides clinicians and other health care professional
information that will help them to detect disease and to confirm or reject the
diagnostics. (McPherson & Matthew R. Pincus, 2011). Managing the follow up
of radiological as well as diagnostics test is a complex process since it
requires information exchange between different health care practitioners
across different services within the health facilities. (Callen, Georgiou, Li,
& Westbrook, 2011). Error in the management of laboratory result can
carries a risk of harm of patient life and these errors are more present to the
pre and post-analytical steps of the total testing process then during the
chemical analytical phases inside the laboratory. (Plebani, 2009)
In this study, we havedevelopeda Computerized Provider Order
Entry (CPOE) systemto capture and shared laboratory data of the patient across
clinical services in the district hospital by the automation of the main pre
and post analytical process that are main source of errors. We have focused a
particular attention of the modelling of the workflow to identify business
process that involve communication between different services and the
laboratory. Through the analysis of business process we have identify the main
actors and describe the system requirements. A particular attention has been
paid to improve patient communication in the proposed workflow.
The system was designed using C# programming language over
.Net Framework 4.0 and PostgresSQL to capture patient and laboratory order data
from the Out-patient department to patient assignment in clinical services. The
result of lab test also has been captured andShort Message Service (SMS) and
email notification features have been integrated to send information to both
patient and clinician where the lab result was available.
TABLE OF CONTENTS
DECLARATION
DEDICATION
ii
ACKNOWLEDGEMENT
iii
ABSTRACT
iv
TABLE OF CONTENTS
vi
LIST OF FIGURES
ix
LIST OF TABLES
xi
LIST OF ABBREVIATIONS
xii
CHAPTER 1
1
1. INTRODUCTION
1
1.1. Background
1
1.2. Problem statement
5
1.3. Framework of the laboratory test order
management system
7
1.4. Justification of the study
9
1.5. Objectives
11
1.5.1. General objectives
11
1.5.2. Specific objectives
11
CHAPTER 2
12
2. LITERATURE REVIEW
12
2.1. The use of automated laboratory data
management with an EMR
12
2.2. The benefits of improving laboratory
data management on the patient safety in care delivery
13
2.3. The importance of laboratory data for
public health monitoring of diseases and epidemics
14
2.4. The benefits of Electronic Health
Record and problems associated with their implementation.
15
2.5. The mobile Health (mHealth)
16
2.5.1. Cell phone text messages for
communication of lab results in Uganda
16
2.5.2. The Mobile Technology for Community
Health (MoTeCH) Initiative in Ghana
17
2.6. The common categories of Computerized
Provider Order Entry (CPOE)
18
2.7. Works on the design and implementation
of Health Information system
19
2.7.1. Design of the Open Medical Record
System (OpenMRS) to support HIV treatment in Rwanda
19
2.7.2. The LabPush system in Swaziland
21
2.7.3. Design of an application for the
chemotherapy treatment process at University Hospital of Geneva
22
2.8. Conclusion
24
CHAPTER 3
26
3. METHODOLOGY
26
3.1. Data collection
26
3.2. System development life cycle
28
3.3. The planning phase
29
3.4. The analysis phase
30
3.4.1. The existing situation
30
3.4.2. Improvements identification
31
3.4.3. Requirements definition
31
Business requirements
32
Functional requirements
32
Nonfunctional requirements
34
3.5. System design
35
3.5.1. System Architecture
35
3.5.2. The process modelling
36
Activity Diagrams
37
Use case diagrams
38
Class diagrams
41
Sequences diagrams
43
3.5.3. The data modelling
45
Conceptual data design
45
Logical data design
48
Physical data design
52
CHAPTER 4
53
4. SYSTEM DEVELOPMENT
53
4.1. The users and system administration
module
54
4.2. The medical staff management module
56
4.3. The patient management module
57
4.4. The appointment and consultation
module
58
3.1. The laboratory test order management
module
59
4.5. The laboratory test result management
module
61
4.6. The report module
65
CHAPTER 5
67
5. DISCUSSION
67
5.1. The design consideration
67
5.2. Benefits of the system
68
5.3. Limitation
69
5.4. Future works
69
6. CONCLUSION AND RECOMMENDATION
71
6.1. Conclusion
71
6.2. Recommendation
72
Reference
74
LIST OF FIGURES
Figure 1.1:Adapted framework of CPOE system in the
district hospital
2
Figure 3.2: System architecture
36
Figure 3.3: Activity diagram
38
Figure 3.5: Use case diagram for patient and
medical staff management subsystem
39
Figure 3.6: Use case diagram for the laboratory
test order management subsystem
40
Figure 3.8: Use case diagram for the lab order
result management subsystem
41
Figure 3.9: Class diagram for the user's management
package
42
Figure 3.10: Class diagram for the location
package
42
Figure 3.11: Class diagram for the order and result
management package
43
Figure 3.12: Sequence diagram for order laboratory
test scenario
44
Figure 3.13: Sequence diagram for record lab test
result scenario
45
Figure 3.14: First ER diagram
47
Figure 3.15: Final ER diagram
50
Figure 4.2: System login form
55
Figure 4.3: Main form of the system
55
Figure 4.4: Users security system access
configuration
56
Figure 4.5: User change password form
56
Figure 4.6: Medical staff personal details
registration
57
Figure 4.7: Patient search form
58
Figure 4.8: Patient registration form
58
Figure 4.9: Patient assignment to clinician
59
Figure 4.10: Laboratory test group order for a
patient.
60
Figure 4.11: List of order place by a clinician
60
Figure 4.12: Laboratory specimen deposit record
62
Figure 4.13: Lab result record and notification
62
Figure 4.14: SMS lab result notification format for
the patient
63
Figure 4.15: SMS lab result notification format for
the clinician
63
Figure 4.16: E-mail lab notification format for the
patient
63
Figure 4.17: E-mail lab result notification format
for the clinician
64
Figure 4.18: Lab result view and treatment
registration form
64
Figure 4.19: Resend of lab result notification to
patient and/or clinician
65
Figure. 4. 20: Patient lab history report
66
Figure. 4. 21: Case-based surveillance reporting
form
66
LIST OF TABLES
Table 3.1: List of laboratory tests for malaria,
tuberculosis and HIV based on WHO IDSR and CDC.(CDC, 2015a, 2015b)(CDC, 2014a,
2014b)(WHO & CDC, 2010)(CDC, 2012)(Caminero, 2005)
2
Table 3.2: Recommended minimum data element of
patient identification based on WHO RSS. (WHO, 1999)
28
Table 3.3: List of attributes of the first ER
diagram
48
Table 3.4: List of attributes of the final ER
diagram
52
LIST OF ABBREVIATIONS
|
AFB
|
:
|
Acid-Fast Bacilli
|
|
API
|
|
Application Programming Interface
|
|
ARV
|
:
|
anti-retroviral
|
|
CDC
|
:
|
Centers for Disease Control and Prevention
|
|
CPR
|
:
|
computerized patient record
|
|
CPOE
|
:
|
Computerized Provider Order Entry
|
|
DBDL
|
:
|
Data Base Definition Language
|
|
DST
|
:
|
Drug susceptibility testing
|
|
EHR
|
:
|
Electronic Health Record
|
|
eLAB
|
:
|
electronic Lab order Entry Management
|
|
ELR
|
:
|
electronic laboratory reporting
|
|
e-mail
|
:
|
electronic mail
|
|
EMR
|
:
|
Electronic Medical Record
|
|
ER
|
:
|
Entity relationship
|
|
ELISA
|
:
|
Enzyme-linked Immunosorbent Assay
|
|
GHS
|
:
|
Ghana Health Service
|
|
HIS
|
:
|
health information system
|
|
HL7
|
:
|
Health Level 7
|
|
HIV
|
:
|
human immunodeficiency virus
|
|
ICT
|
:
|
Information and Communication technologies
|
|
IS
|
:
|
information system
|
|
IDSR
|
:
|
Integrated Disease Surveillance and Response
|
|
IHE
|
:
|
Integrating Healthcare Enterprise
|
|
IIBA
|
:
|
International Institute of Business Analysis
|
|
LOINC
|
:
|
Logical Observation Identifiers Names and Codes
|
|
MOH
|
:
|
Ministry of Health
|
|
MDR
|
:
|
Multi drug resistance
|
|
NAA
|
:
|
Nucleic acid amplification
|
|
OpenMRS
|
:
|
Open Medical Record System
|
|
PC
|
:
|
personal computer
|
|
PIN
|
:
|
Personal Identification Number
|
|
PCR
|
:
|
Polymerase Chain Reaction
|
|
RDT
|
:
|
Rapid diagnostic test
|
|
RSS
|
:
|
Recommended Surveillance Standard
|
|
RDBMS
|
:
|
Relational Database Management System
|
|
SMS
|
:
|
Short Message Service
|
|
SQL
|
:
|
Structured Query Language
|
|
SNOMED-CT
|
:
|
Systematized Nomenclature of Medicine-Clinical Terms
|
|
SDLC
|
:
|
systems development life cycle
|
|
HUG
|
:
|
the University Hospitals of Geneva
|
|
TB
|
:
|
Tuberculosis treatment
|
|
UML
|
:
|
Unified Modeling Language `
|
|
USA
|
:
|
United States of America
|
|
USB
|
:
|
Universal Serial Bus
|
|
WB
|
:
|
Western blot tests
|
|
WHO
|
:
|
World Health Organization
|
CHAPTER 1
2. INTRODUCTION
2.1. Background
The laboratory services play important role in health care
provision and an estimation of 70% of all medical decisions made by clinicians
are based on the results of laboratory test. The laboratory provides clinicians
and other health care professionals information that will help them to detect
disease or predisposition to a certain disease, to confirm or reject as
diagnostics, to establish prognostic and to monitor efficacy of therapy
followed by a patient.(McPherson & Matthew R. Pincus, 2011)
Managing the follow up of radiological test as well as
diagnostics test is a complex process since it requires information exchange
between patients, doctors, nurses and laboratory technician using a combination
of information systems, including paper-based, telephone and electronic
systems. This environment with multiple steps, players and information systems
increases the risk of errorswhich could lead to suboptimal clinical outcomes.
It is also shown that the rate of missed results test is highin hospitals which
used entirely paper-based systems and in those which used amixture of paper and
electronic systemsdue to the error in the communication workflow between actors
within the health care setting. (Callen et al., 2011)
In a qualitative study conducted in United States of America
(USA) in 2010 by Nancy C. Elder and al, practicingfamily physicians confirm
that the implementation of an Electronic Medical Record (EMR) was the most
important achievementdone to decrease testing process errors. Custom results
management information systems have been reported to improve both physician and
patient satisfaction then a standard EMR.(Elder, Mcewen, Flach, Gallimore,
& Pallerla, 2010).
Computerized providerorder entry (CPOE)allows medical staff to
enter electronically orders for medications, diagnostic tests, and regiments as
well as procedures before a surgery, with the objective to improve the clarity
and specificity of physician orders, to facilitate the rapid communication of
orders, and to providesignificantly enhanced decision support capabilities
compared to traditional handwritten orders.(Maslove, Rizk, & Lowe, 2011)
Continuous quality audit requirementssuch as electronic system
that providescapacity for clinicians to acknowledge that they have viewed test
results and document their follow-up actions in the systemhasbeen advocated to
improve the communication workflow in the management of test result. But many
facility still continue to use the traditional practice in the laboratory
result management andone of the most used is to telephone results for urgent or
critical tests to clinician. It has proved to be time-consuming with potential
for errors and the one of using mobile phone calls has also been proved to be
expensive.(Callen et al., 2011)
The computerized system for managing the laboratory test
result do not solve the communication process problem between actor involved in
patient care even if some improvement has been recognized. A systematic review
conducted in 2011 on the implication of missed test result for hospitalized
patient, reveals that by replacing the telephone call notification of urgent
laboratory result with a computer system,28.8%(529/1836) of the urgent
biochemistry lab results during a six-month period were never accessed. The
radiology follow-up assessment using an email alert system for important
radiology investigation reported that 20.0% (10 598/52 883) of email were not
viewed by the referring physician.(Callen et al., 2011)
The communicationbetween health care providers and patients
isalso an essential component of the patient care. Traditionally, face-to-face
and telephone communication have been the primary means for the patients to
interact with their health providers. However, with advances in technology,
internet applications for communications, particularly electronic mail (e-mail)
or mobile technology like Short Message Service (SMS) can be also used as
viable media for patient communication. While benefits of e-mails in enhancing
communication were recognized by both patients and providers, concerns about
confidentiality and security were also expressed.(Ye, Rust, Fry-Johnson, &
Strothers, 2009)
In rural and resource-limited settings area of Africa, where
internet still present some logistic problems, the widespread availability of
mobile communication, along with its ease of use and relatively low cost make
it a promising medium to improve health related communications.(Siedner,
Haberer, Bwana, Ware, & Bangsberg, 2012)Recently severalinitiatives has
been conducted to Internet connectivity to a growing number of remote locations
within the rural area but the internet traffic demands was not able to deliver
basic quality services needed for simple web application due to the poor
infrastructure, lack of economic interest from telecommunication providers and
lack of the governmental support result in a relatively disconnection in large
part of rural area.(Johnson, Pejovic, & Belding, 2011)
Cell phone text message (SMS) is been demonstrate to be an
important tool to improve communication with patient and to solve challenges
related to transportations and access to clinicians in rural area. In a study
conducted in southwestern Uganda in 2012 to assess the acceptability of using
SMS for communication with human immunodeficiency virus (HIV)-infected
patients, all participants expressed interest to receive information about
laboratory results by cell phone text message, stating benefits of increased
awareness of their health statusand decreased transportation costs due to the
reduction of movement between the house and the health facility.(Siedner et
al., 2012)
Even though issues related to privacy and confidentiality of
information has been raised, some measures like the use of the Personal
Identification Number (PIN) code and deletion of the message after receiving
the notification have been retained as measures to protect
confidentiality.(Siedner et al., 2012)
Despite of EHR benefits, in most African country, public and
private hospitals are still running paper based system for laboratory order or
semi-automated system combining stand alone or web application and use of email
to share result between clinicians and laboratories technician. Only a few
established ones has implemented an Electronic Medical Record (EMR) or a
Computerized Provider Order Entry system for radiology, pharmacy and laboratory
department.(Jiagge, 2007)
In Ghana thereare four main categories of health care delivery
systems:«the public, private-not-for-profit, private-for-profit, and
traditional systems» centered on the Ministry of Health (MOH). The MOH is
the policy maker body and all the health sector actors are responsible to it.
MOH uses the Ghana health service for the implementation of the policies.
Established by the Ghana Health Service and Teaching Hospitals Act 525, 1996,
the Ghana Health Service (GHS) is responsible for the administration and
management of the hospitals owned by the government and excluding teaching
hospitals and quasi-state institutions such as the universities and security
services (Military and police hospital).(MOH Ghana, 2009)
The health services are organizedon a three-tier system of
care; from primary through secondary to tertiary services. They are run at five
levels from bottom to top: community, sub district, district, regional and
national. The community and sub-district levels health facility provide primary
care. Thedistrict and regional hospitals provide secondary health care. The
teaching hospitals are the top inproviding tertiary services and they are
responsible for the most specialized clinical and maternity care. (MOH Ghana,
2009)
Clinical care at the district level are assured by the
district hospital and they are supposed to serve an average population of
100,000-200,000 people in a clearly defined geographical area. District
hospital contains between 50 and 60beds and should provide the following
services: «Curative care, preventive care, and promotion of heath of the
people in the district. Quality clinical care by a more skilled and competent
staff than those of the health centers and polyclinics.Treatment techniques,
such as surgery, laboratory and other diagnostic techniques appropriate to the
medical, surgical, outpatient and in-patient services». (Ghana Health
Service, 2015)
The aim of this project is to use information system approach
to improve the management of the laboratory orderwithin the district hospital
by taking into account the data workflow between clinical services and improve
patient communication experience using notification alert based on SMS and
email capabilities provide by mobile technology and internet.
2.2. Problem statement
Clinicians rely heavily on laboratory data to make medical
decisions. Even though there is evidence that the Electronic Medical Record
(EMR) introduction in the clinical setting has improved the management of
patient related medical record, there is still some problem to solve. One of
them is the follow up of the laboratory test result by both the referring
clinician and the patient and the exchange of information between care givers
in the facilities.(POON, KUPERMAN, FISKIO, & BATES, 2002)
Although the CPOE for laboratory result has improved the
management and access to the test result, many studies have shown that passive
retrieval of information in CPOEsystem since the clinician have to use the
computer to pull the information from the test management system has created a
loss of follow-up of the lab result, especially for outpatient comparing to
inpatient and those in emergency department.(Callen et al., 2011)
Another commonly cited problem in lab information management,
is the breakdown of communication between actors that are involved in the
patient care. The traditional practice of telephoning results to the referring
clinicians is time-consuming with potential for errors, and left other actors
like nurse out of the communication process meanwhile they are those who gave
treatments to the patient based on the guideline recommended by the clinician.
Most of laboratory management information system also do not take into account
the cross-boundary communication process with integration of the
actorsinvolved. The patient should also be associated by getting informed on
the action that should be taken for his care. Thus, sharing the right
information in time between actors involve in the patient care allow to improve
the outcome of patient care since critical test result will be shared between
actors and serviceswithin the health facility (Callen et al., 2011)
Provision of reliable internet connectivity to support use and
deployment of web based EHR as well as integration of web based Application
Programming Interface (API) is a challenge in rural area due to the lack of
interest of internet provider to invest in expensive equipment for area of low
economics opportunity.
A desktop computerized provider order entry system that will
provide an effective and efficient managementcapabilities of laboratoryorderand
facilitates the exchange of lab test information across clinical service
boundary, can be used as part of solution to this problem. Patient and
physician interactions and communication experience with the laboratory in the
proposed solution are based on the use of SMS over GSM and email to send alert
and notification.
2.3. Framework of the laboratory test order management
system
The Integrating Healthcare Enterprise (IHE) initiative defines
the laboratory order schedule workflow based on a description of interaction
processes and exchange of information in the form of use-cases, actors,
transactions. The IHE schedule workflow provide international standard of
software requirement in radiology, imaging and laboratory diagnostic
techniques.Itinvolves intensive collaboration and communication among actors by
using transaction to meet the identified process management in clinical
setting. (Spronk, 2012)
The IHE schedule workflow identified actors in term of their
applications roles in the system and the interaction between them is based on
exchange information protocol like Health Level 7 (HL7).According to the IHE,
the mains transaction identified are: patient registration and update
management, order place management, order fill management, test result
management, work order management, order result management. (Spronk, 2012)
The transactions between different actors across the clinical
setting ensure the laboratory data workflow and failed to establish one the
transactions in the system requirement implies breakdown communication of
workflow that lead to the problems cited above such as: patient
misidentification, specimen misidentification and collection error, lost to
follow up of order, poor communication between clinical services and poor
patient communication with the health facility(Plebani, 2010).
According to the requirement of a district hospital in Ghana,
the following adapted workflow (Figure 1.1) will be used as the study
framework. The framework of laboratory order in the district hospital
identifies different interactions between actors involves in the test
management processes.The Computerized Provider Order Entry (CPOE) system is the
hub of the flowchart diagram and aims to establish link between actors in term
of process management. The actorswho are involved in the lab test management of
the proposed workflow are: the patients, the nurses, the physicians, the
laboratory technicians and the public health departments.
The interaction of patient is done in the system in term of
visit at the Outpatient department and in term of reception of notification of
laboratory result. The patient can also interact with the laboratory service
without passing through the OPD in case that the laboratory order come from
another health facility. Physician, nurse and lab technician interactions are
done through the test order, the lab test management and patient appointment
with the physician inside the specific department. Public health department
receives periodic report for decision making and to produce report on disease
surveillance event (Ghana Health Service).

Figure 1.1:Adapted framework of CPOE system in the district
hospital
2.4. Justification of the study
The laboratory play an important role for medical decision,
and clinician rely on it to provide better treatment to patient. The clinicians
therefore need to have a tool that will assist them to make laboratory test
order, to check if the result of the lab test ordered are available and if
neededto be notified by the laboratorywhen results are available. The
laboratory service should be able to record accurate data on disease diagnosed
and to produce efficient report for the disease surveillance. The patient also
as the most concerned person should have the possibility to know if his/her
laboratorytest results are available so he can schedule a meeting with the
clinician.
Since the use of mobile devices in healthcare has been proven
to facilitate coordination of patient care, care standardization, communication
between patient and health care providers.(Hao et al., 2015) Using this
technology in the proposed solution will allow patient and medical staff to
improve their communication experience with the health facility. Since internet
is still a challenge in a lot of African rural area to support a good quality
of service (QoS) for the use of web application, the system architecture will
be based on a client-server desktop application with alert notifications based
on SMS over GSM network instead of using internet API. The email notification
will be based on the use of internet but no component will be hosted on
internet.
In Ghana, the district hospital is one of the five functional
levels of health care distributionthat provide the first level of advance
clinical care, laboratory and diagnostic techniques. And we think that there is
need to provide this facility with heath information system that will allow to
manage their laboratory data with good coordination and exchange between
different services. Developing a Computerized Provider Order Entry system for a
district hospital will allow:
1. The Outpatient Department (OPD) to manage efficiently
patient information
2. The different clinical servicesto keep accurate
information on patient and their related laboratory test history
3. To provide better access to patient laboratory result test
by sharing the treatment guideline and the lab result between attending medical
practitioners (nurses, laboratory technician and physician)
4. To establish fast and timely notification of the laboratory
result by SMS and /or email to both patient and clinician.
5. To provide accurate information to the public health
department for disease surveillance
2.5. Objectives
2.5.1. General objectives
The main objective of the study is to developa Computerized
Provider Order Entry (CPOE)to capture, to track and exchange patient laboratory
order and related test result across the clinical services in a district
hospital.
2.5.2. Specific objectives
- To develop a Computerized Provider Order Entry (CPOE)
systemto capture information on the laboratory order and related test.
- To propose an adapted workflow that will facilitate the
exchange of patient laboratory information between the patient management
system, the clinical services and the CPOE.
- To establish anautomated and an efficient communication of
laboratory result between the patients, medical practitioners and the
laboratory technicians using mobile technology and internet.
CHAPTER 2
3. LITERATURE REVIEW
To help understanding the most recent development and
achievement on the capability of a laboratory test management information
systemto improve patient communication within the health facilities, the
communication of medical practitioners within the clinical setting, and the
efficiency and the health care quality, we will conduct the review onthe use of
automatedlaboratory data management within an EMR, on the benefits of improving
laboratory data management on the patient safety in care delivery, on the
importance of laboratory data for public health monitoring of diseases and
epidemics, on the benefits of the Electronic Health Record (EHR) and their
implementation problems, and then on the mobile health (mHealth). The review on
the common categories of CPOE and a particular focus on the laboratory order
and lab result management automation will be also be done, then we will
conclude with the review on some cases on the design and implementation of
health information system (HIS)that involve the automation of management of
the laboratory data.
3.1. The useof automated laboratory data management with an
EMR
Laboratory, radiology results serveclinicians in healthcare
for screening, diagnosis of the disease and medication management.In the study
conducted by Nancy Elderand others in 2010, focused on «the documentation
of results management steps in patients charts at eight primary care offices in
the southwest Ohio region» (Elder et al., 2010)in USA.The research team
assessed whether results managed by an Electronic Medical Record (EMR)or by a
specialized lab management system improve the lab test documentation comparing
to manual and paper based practices. Observations, interviews with clinical
staff, and chart audits of twenty five (25) patient in each offices as been
used to assess the efficiency of the two systems. In this study, the clinicians
have expressed concern that EMR for managing test results just as part of
patient medical record are not satisfactoryeven if they have recognized a
significance improvement, compared to in-build system focus on laboratory data
management. (Elder et al., 2010)
Since, there are multiple steps involved in the management of
test results, beginning with offices tracking their orders and the return of
results to the clinician's office,one of the concern expressed is related to
the breakdown of communication process between clinician, lab technician and
nurses.The lost to follow up of laboratory test result by the practitioner
involved in patient care is also cited as a major problem in lab result
management. The research team has found that 64% of results managed with the
laboratory data management system had a follow-up plan documented compared to
only 40% of paper managed results. They find also thathaving two or more
standardized results management steps did not significantly improve
documentation of any stepsince there are not take into account in the standard
EMR. Instead all offices fall short in notifying patients and in documenting
interpretation of the laboratory result. (Elder et al., 2010)
3.2. The benefits of improving laboratory data management on
the patient safety in care delivery
Qualitymeasurement inhealthcare is going to be focused on
accountability for patient care outcomes and not onlyon quality assurance
sinceevery step in the process of patient care carries a risk of harm.In
relation to the quality assurance within the clinical laboratory, recent
improvements have been done to significantly decrease the rates of errors, but
the procedures before and after the clinical test are more prone to the
introduction of errors.(Plebani, 2009) In the study conducted by Mario Plebani
in Italy, to assess quality indicator of laboratory test. The author mentioned
that event if a lot ofefforts have been donein the last decade to implement
quality indicators for laboratory tests focused on the analytical performance,
a systematic framework for laboratory quality measurement is still not
available. The evaluation is based on the laboratory capability to provide
service that is safe, timely, efficient, effective, equitable, and
patient-centered. This study demonstrates that pre and post-analytical steps of
the total testing process are more error-prone than the analytical phase inside
the laboratory since the diagnostic process, which consists of numerous
clinical steps, stretches across multiple care providersin the hospital. Some
of the identified error are:the inappropriate test request from clinician,
error in patient identification and specimen collection, lost to follow up the
lab test. (Plebani, 2009)
3.3. The importance of laboratory data for public health
monitoring of diseases and epidemics
The improvement of laboratory result management does not only
improve patient care but it is also essential for disease monitoring and
surveillance. The reports of disease notifiable conditions from laboratories
and health care providers to public health authorities, is fundamental to the
prevention and control of population health related problems.(Overhage,
Grannis, & McDonald, 2008)
In the study conducted by J.Marc Overhage and others in 2008
in Mario County in Indianapolis, the research team examines whether the
information produced by the automated electronic laboratory reporting of
notifiable-diseases are more complete, accurate and timely produced than those
produced by the paper based reporting procedure. Two source of data has been
compared: the first source is an automated electronic laboratory reporting
(ELR) system, the Indiana Network for Patient Care (INPC) notifiable condition
database that link laboratories, radiology centers, and public health
departments in central Indiana in a shared database, and he second source the
Marion County Health Department usespaper-based records. (Overhage et al.,
2008)
After 3month study period, the team found that the ELR
identified 4.4 times as many cases as traditional spontaneous reporting methods
which show that automated system more-timely report the notifiable diseases
conditions than does traditional spontaneous reporting. And the data produced
by the electronic reporting of notifiable conditions can be easily mapped and
scale with the Logical Observation Identifiers Names and Codes (LOINC) for
laboratory test result and the Systematized Nomenclature of Medicine-Clinical
Terms (SNOMED-CT) clinical condition according to the Centers for Disease
Control and Prevention (CDC). (Overhage et al., 2008)
3.4. The benefits of Electronic Health Record and problems
associated with their implementation.
Electronic Health Record (EHR), «has the aimof providing
comprehensive, cross-institutional, longitudinal records of patients health and
healthcare data», it provides the following benefits: cost reduction
explained by future increases in revenue and cost savings, reducing errors in
pharmacy, laboratory and in medication order as well as in finance and
accounting. The improvement of coordination can be also cited as a benefit
since it improve organizational coordination within the health care facility
and between health care providers like health insurance.(Kimble, 2014)
But the organizational coordination can result to the cross
border interoperability problem between stakeholder information systems.
Instead of all these benefits a lot of EHR implementation program failed, the
EHR-IMPLEMENT program under the auspices of a European Union initiative can be
cited as an example of the large EHR implementation failure. In the study
conducted by Chris Kindle in 2014, to underlying problems that prevent EHR
systems from delivering its benefits, mains causes of failure has been
identified using the ethnographic studies of EHR systems to assess the waythat
such systems are used within the clinical setting .The problems ofpaper
persistence information exchange between services and organizations after the
introduction of the automation, the breakdown of coordination and communication
across the professional boundary in health care, and limited share of knowledge
between medical professional group since the documentation of patient actions
and treatment is managed separately by each specialty services within the
hospital are the main causes of the failure apart of those who are related to
all information system. (Kimble, 2014)
3.5. The mobile Health (mHealth)
The widespread availability of mobile communication, along
with its ease of use and relatively low cost make the mobile technology an
improvement tools in health data management.(Siedner et al., 2012) According to
the International Telecommunication Union, mobile phone subscriptions in
developing country have increased over 4-fold globally to nearly 1213 to 5,400
million subscriptions during the period 2005-2014. The most substantial
increases in cell phone access have occurred in sub-Saharan Africa.(ITU,
2014)
3.5.1. Cell phone
text messages for communication of lab results in Uganda
A study conducted in Uganda in 2012 by Mark J Siedner and
Others, to assess the acceptability for SMS to improve communication of
laboratory results with HIV-infected patients, the cell phone use practices and
literacy among them, and the issues about privacy and confidentiality of
receiving private health related information by Short Message Service on their
cell phone. The interview techniques to assess their understanding of the
subject as defined in the study objectives.(Siedner et al., 2012)
The researcher's team finds that a significant proportion of
patients preferred the SMS notification of laboratory results to the existing
system of learning laboratory results at the next clinic visit. Participants
also cited secondary benefits like improvement of relationship with clinic
staff and providers, and decreased of transportation costs when using SMS to
communicate laboratory result information, even thoughaconcern has been raised
about the confidentiality. According to the privacy and confidentiality
issuean interest of using Personal Identification Number (PIN) code activation
and deletion of SMS message after reading has been recognized to be efficient.
As such, it is important that patients understand and accept these risks prior
to receivingsensitive SMS information. (Siedner et al., 2012)
3.5.2. The Mobile
Technology for Community Health (MoTeCH) Initiative in Ghana
In Ghana, in 2009, Columbia University, the Grameen
Foundation, and the Ghana Health Service launched a program of technology
development and research designed to evaluate the potential uses of mobile
technology in supporting community health operations, known as the Mobile
Technology for Community Health (MoTeCH) Initiative. In the study conducted by
Bruce Macleod and others to describe the software architecture of a system that
is designed in response to the health development potential trend of the rapid
expansion of community health worker deployment and the global proliferation of
mobile technology coverage; and their use in poor countries, the research team
analyzes the problem of the need of high quality and accurate information in
the management of pregnant woman and labor information in the health
administration.The awareness of the young pregnant women in the follow up of
the antenatal and postnatal care has been also analyzed. One of the method they
used to address the issues cited above is the integration of the mobile phone
into the rural health system to bridge key health information gaps. (Macleod,
Phillips, Stone, Walji, & Awoonor-Williams, 2012)
In the solution proposed by the MoTech system, some of the
particular scenariorelated to the use of mobile phone that illustratethe
potentials of mobile health (mHealth) benefits are: the reception of voice
messages in health education by pregnant woman,the collection of patient data
using low cost mobile phone and the reception of a weekly SMS message onwomen
who are delayed for routine schedule care by nurses.(Macleod et al., 2012)
3.6. The common categories of Computerized Provider Order
Entry
In the study conducted by Timothy Huerta and others in 2013,
to evaluate the contribution of an automated laboratory test order management
system (eLAB)on the duplication and unnecessary ordering of laboratory and
diagnostic tests within U.S hospital, they have identified three major class of
CPOE prior the analysis. The first and the most frequently discussed in
litteratre is the electronic prescribing (ePrescribing or eRx).due to the focus
on patient safety, and the significant role that medication errors play in
compromising care quality. The second isthe CPOE involves the standardization
of clinical order set entry that describe the activities of care that a patient
should receive prior or after an intervention. We can cite the dietary
restrictions, physical therapy and wound care. The use of the second class
CPOEhas been the slowest due to the complexity and workload to manage that
category of data.(Huerta, Thompson, Ford, & Ford, 2013)
The third class of CPOE, and the subject of our study, is the
use of electronic Lab order Entry Management(eLAB )systems for ordering of
diagnostic tests that are conducted in a controlled manner such as imaging and
microbiology test. eLAB systems provide a structured and auditable framework in
which laboratory data may be captured and communicatedthrough the establishment
of a single point of contact for laboratory ordering and results.The basic
principal of eLAB systems is that redundant tests can be minimized and clinical
decision-making is further supported.(Huerta et al., 2013)
3.7. Works on the design and implementation of Health
Information system
3.7.1. Design of
the Open Medical Record System (OpenMRS) to support HIV treatment in Rwanda
In the study conducted by Chritian Allen and others in Rwanda
in 2007, to support the process of patient registration, therapy initiation and
treatment monitoring' of HIV-affected person, the research team has developed
and implemented the OpenMRS system to support their user's requirements. Open
Medical Record System (OpenMRS) is a web-based electronic medical record system
that has been developed to address the problem of configuring EMR systems to
suit new sites, languages and diseases after the deployment. (Allen et al.,
2007)
The user's requirements of Rwanda was based on the management
of HIV patient on active anti-retroviral (ARV)treatment and Tuberculosis
treatment (TB). In their methodology to find the system that will meet the need
to support new HIV and Multi drug resistance (MDR)-TB treatment projects, the
research teamneeded a system that isvery flexible and scalable andthat will not
require expert programming skills to add new forms or tailor it to new sites,
languages or diseases requirements.The system should alsoshould be web based
andshould allow local «offline» data entry. (Allen et al., 2007)
After looking for an existing EMR systems,they found thateven
though some commercial EHR system could fulfill a part on their requirements,
they areclosed, proprietary and, typicallyexpensive and not designed to be
extended on the sites after the system deployment. And, the small number of
open source EMR available do not have the characteristics required for the
project. So the team decided to develop a new system architecture called
openMRS.(Allen et al., 2007)
The OpenMRS system is built in Java using the Spring
application framework and the Hibernate for back-end data persistence over
MySQL database or any Relational Database Management System (RDBMS) that
support hibernate. The originality of OpenMRS comparing to other open source
system is the integration of a comprehensive data dictionary for all clinical
data that allow new data model to be added without programming and altering the
database structure.(Allen et al., 2007)
The laboratory data collection and management system was not
part of the initial project and the specific need of order entry system did not
allow the integration of this module in OpenMRS. To solve this problem, a Java
standalone systemhave been developed as asimple laboratory data collection
application using MySQL database to meet thestandard needs of the country.This
module willallow to search the patient, to register lab orders and results, to
send sent alerts as an SMS message to a clinician's mobile phone using the
Skype™ Application Programing Interface (API). The lab data can be
synchronized with openMRS using health level 7 (HL7). Other functional modules
as Report module and pharmacy data management have been also integrated later
easily with the use of HL7. (Allen et al., 2007)
But the main challenge in the openMRS system architecture is
the data synchronization of all local site with the main server on line, since
OpenMRS need reliable internet connection to correctly synchronize the
data.(Allen et al., 2007)
3.7.2. The LabPush
system in Swaziland
Mobile technologies are widely available and can play an
important role in health care at the regional, community, and individual
levels. In Swaziland, although National laboratoryis usually able to accomplish
the requested test and produce the result within two days after receiving the
samples, the time for the results to be delivered back to clinics is quite
variable depending on how often the motorbike transport makes trips between the
clinic and the laboratory. (Hao et al., 2015)
In the pilot study conducted by Wen-Rui Hao and others in
2014, to assess factors facilitating and hindering the adoption of mobile
devices in the Swaziland healthcare through the evaluation of the end-users
experiences, the Taipei Medical Universityperform a feasibility studyfor the
development of a system that will allow the physicians to receive laboratory
test result on the mobile phone through SMS. The research team
conductsinterview with medical staff and come out with a software requirement
document that serve as input to the software development team.According to the
users' requirement, ten laboratories test has been considered the most urgent
to be communicate by the medical staff. Those one should be notify to
clinicians prior the receptions by the traditional ways (Motorbike mail) of the
full report details on paper.(Hao et al., 2015)
Due to the limitation of internet access in health facility
the SMS has been chosen as the better way of notify lab result through the
country. The system will be installed at the national laboratory and the
notification are sent to the remote clinic through SMS. The SMS should also
contains the patient information and the code number for the laboratory test
which should be enter in the system and submit after the validation. A mobile
phone with a SIM card was provided to each participating clinic, and the use of
this mobile phone was restricted to only receiving laboratory results via SMS.
Missing lab result can be requested to the National laboratory that can be
resend by SMS that improve follow up of missing lab result(Hao et al., 2015)
At the end of the pilot study, the participant has recognized
the improvement of communication of laboratory result between the National
laboratory and the clinics. But the participant has expressed the concern about
the workloadwith the introduction of the labPush system since they have to
transcribe the result from the phone to the paper based log book to keep
thehistory of the patient result test.(Hao et al., 2015)
3.7.3. Design of an
application for the chemotherapy treatment process at University Hospital of
Geneva
Decision support, order entry, drug and care administration
with their respective documentation cannot be seen as independent actions,
especially in term of medical approach and patient safety. Chemotherapies
errors in the process cited above can have dramatic effectson the patient life.
In this study, Stéphane Spahni and otherspresent the overall approach
leading the computerization of order entry, drug and medication
administration.The research team conduct also the first evaluations about the
potential benefits of the computer-aided controls during the care
administration phaseat the University Hospitals of Geneva (HUG). (Spahni et
al., 2007)
In an effort to minimize the potential for
chemotherapy-related errors, the HUGinitiated a project that start with the
centralizationofthe pharmacy and the laboratorydata to manage the preparation
of the right chemotherapies provide to the patient. All the related actions
involved the laboratory test and the preparation of the right chemotherapies
arecalled the protocol. HUG as already at the time of the study an in-house
developed computerized patient record (CPR) systemdeployed in thirtyfacilities
and runs on more than 4,500 personal computers.After setting up a global
database, an application has been developed over this data repository for
managing the request of new preparations, for organizingthe concrete
preparations and managing the traceability before, during and after the
production process. The Application has 3 main modules: the prescription side,
the pharmacy side and the drug administration or the nursing side.(Spahni et
al., 2007)
The prescription side is the features of the system that help
the oncologist to follow their patients and the current status of all running
protocols.It is a powerful feature that allow the management of the patient
treatment and the following up of the associated side effects through the
production of alert such as the overlapping dates, regimens and some anomalies
in the laboratory results. The pharmacy side allow the management of most of
the logistics needed to produce drugs from raw substances since some regiment
are produced specifically by the HUG's central pharmacy.The protocol production
for a patient is computerized during the drugs validation and laboratory
analyses.(Spahni et al., 2007)
The Drug administration side, is the complex side of the
system, it gives for each patient the treatment to follow, the side effects of
the treatment and the precaution to follow. The bedside traceability of patient
in the ward and the nurse who gives treatment is also managed by this module. .
This module is deployed on the pocket personal computer (PC) The patient, the
nurse and the treatment are both identified using an international numbering of
objects code called GS1 that can be read by the Pocket PC.(Spahni et al.,
2007)
After the evaluation of the impact of the introduction of the
system, the benefits in patient safety, the acceptance by the users and the
integration of the system in the workflow process of the hospital has been
observe as positive outcomes.However, it must be emphasized that the
formalization and the validation of all processes, including each protocol,
require a significant amount of time, especially from oncologists.(Spahni et
al., 2007)
4. Conclusion
During the review of the literature, we have identify the
following key point that will be considered in our study as guideline in the
solution we are seeking to provide on the computerization and automation of the
laboratory test order and result:
1. The testing process is complex since it involve many actors
from the order to the identification of the patient and the management of
laboratory test data.
2. The difference between clinical services creates a
breakdown of communication of flow of information of the test orders and
results since each specialties has a specifics group of diagnostics
investigation and, documents the patient record in a particular way that can
create duplication of patient information in the same hospital.
3. The automation of the management of the laboratory and
related diagnostics with a standard EMR has been proven to bring significant
improvement comparing to the paper based method. But specific health
information tools like CPOE has been proved to be more efficient for laboratory
data management than the customization of an EMR.
4. Even though some success stories has been cited and the
benefits of the electronic medical record has been proven after a lot of
implementation, the case of failure has also been recognized since the
deployment of the system does not provide the expected satisfaction. Those
challenges should be solve prior and during the deployment of the all health
information system.
5. A participatory involvement of medical stall in the system
requirement is an important step in the deployment of any health information
system and a qualitative assessment should be conducted to have feedback of the
medical practitioner on their user experience to avoid the case of abandon of
health system observed in some project.
6. The patient satisfaction should be key factor when
developing any health information system and the impact of the information
system on the medical staff workload should be minimized as possible.
7. theavailability and low cost of mobile phone even in poor
setting area makes mobile technology a viable medium to improve patient and
clinician communication experience in health care .
CHAPTER 3
5. METHODOLOGY
In this chapter, we describe the method used to analyze and
design the CPOE. We describe the mains source of the data used to build the
system starting from the chosen workflow to the business requirement
definitions. The workflow has been adapted to fit the need of a district
hospital in Ghana. We also describe the various stages in the system
development process as well as tools and techniques used to model and design
the system.
5.1. Data collection
The study was focused on the laboratory test used in the
diagnosis ofthree infectious diseases: malaria, tuberculosis and Drug
susceptibility testing (DST), and human immunodeficiency virus
(HIV).(M'ikanatha, Lynfield, Beneden, & Valk, 2013). For each of these
three diseases cited above the laboratory tests technique was based on the
criteria used by laboratory to confirm diseases, as described in case
definition for Integrated Disease Surveillance and Response in Ghana which is
based on technical guide for Integrated Disease Surveillance and Response
(IDSR) in the African region edited by World Health Organization (WHO) and
Centre for Disease Control and Prevention (CDC).(WHO & CDC, 2010) the table
3.1 shows for the chosen infectious disease the common laboratories test that
are used for diagnosis.
|
Diseases
|
Specimen
|
Laboratory tests
|
|
Malaria
|
Blood
|
Rapid diagnostic test (RDT).
|
|
Polymerase Chain Reaction (PCR) test.
|
|
Detection of parasites in thick or thin peripheral blood films
|
|
Tuberculosis and related drug resistance test
|
Sputum
|
Sputum specimen positive for Acid-Fast Bacilli (AFB) by
microscopy.
|
|
Sputum specimen positive on culture forAFB.
|
|
No specimen
|
The Mantoux tuberculin skin test.
|
|
Sputum
|
Isolation of M. tuberculosis
|
|
Nucleic acid amplification (NAA) tests
|
|
Drug susceptibility testing (DST)
|
|
HIV
|
Blood
|
Enzyme-linked Immunosorbent Assay (ELISA)
|
|
Western blot tests(WB)
|
|
P24 HIV antigen based testing.
|
Table 3.1: List of laboratory
tests for malaria, tuberculosis and HIV based on WHO IDSR and CDC.(CDC, 2015a,
2015b)(CDC, 2014a, 2014b)(WHO & CDC, 2010)(CDC, 2012)(Caminero,
2005)
The identification of patient information was based on the
recommended minimum data element, data analyses, report and presentation as
described in WHO Recommended Surveillance Standard (RSS) document. Phone number
and email of the patient will also be collected to allow the reception of SMS
and email notification.The identification information of the clinicians
ordering the laboratory test has beenalso collected with his/her phone number
and email, to allow the system to send laboratory results alert to the
clinicians. The Table 3.2 contains the set of data for the patient and
clinicians based on the WHO RSS
|
Disease
|
Minimum set of data
|
|
All (Malaria, Tuberculosis, HIV)
|
- Names of Patient
- Date of birth
- Sex
- Patient ID number or folder number (if available)
- Patient cell phone number (Compulsory)
- Patient e-mail (optional)
- Names of clinician who ordered the test
- Licence number of the clinician who ordered the test
- Cell phone number of the clinician who ordered the test
- Email address of the clinician who ordered the test
- Specimen condition
- Final lab results
- Notification type chosen by the clinician
- Date at which the clinician ordered the test
- Date Lab receive the specimen
- Date of final lab results
- Date of notification of the result to the patient
- Date results sent to the clinicians
- Location of patient ( at least at the District level)
- Location type (Urban/Rural) of patient
|
|
Malaria
|
- Pregnancy status
|
|
Tuberculosis
|
- Is it the first test for TB
- Reason: diagnosis, follow-up
- Date of the first diagnosis
- Treatment failed
- Treatment interrupted
|
|
HIV
|
- Pregnancy status
|
Table 3.2: Recommended minimum
data element of patient identification based on WHO RSS. (WHO, 1999)
5.2. System development life cycle
The systems development life cycle (SDLC)was applied to
provide a descriptive or prescriptive characterization of how the CPOE
systemwas developed. The SDLC describes phases of the software cycle and the
order in which those phases are executed. (Ragunath, Velmourougan, Davachelvan,
Kayalvizhi, & Ravimohan, 2010).
According to the SDLC approach, we followed the phases cited
below for the design of the system (Parsons & Oja, 2014):
1. The planning phase
2. The analysis phase
3. The design phase
4. The development and testing phase
5. The implementation phase
6. The maintenance phase
The implementation and the maintenance phase involve the
installation of the new information system and the conversion of the
organization procedures to use it. In this study the deployment of the new
system in a hospital is not planned so the implementation and the maintenance
phase was not part of the study.
5.3. The planning phase
The planning phase is the fundamental process of understanding
the main reason for building the new information system (IS).Itdetermines how
the project team will proceed to achieve the goal. It has two steps: the
project initiation and the project management (Dennis, Wixom, & Roth,
2012).
During project initiation, we have to identify the task
performed by different actors in the lab order management and the challenges of
using manual system or no optimized system to manage lab test data. The
structured interview technique is one of the efficient way of collecting
information on the user needs. Based on the information found in the literature
reviewrelated to our study, the laboratory order communication between medical
staff within the hospital, the risk of miss to follow-up of the patient lab
results and the notification of the test results to both referring clinicians
and patients are the main problems identified at the health facility that
provide advance clinical care, laboratory and diagnostic techniques to a lot of
people in a clearly defined area. Thus, these problems could correspond to the
problems found at the district hospital based on the functional levels of
health care distribution in Ghana. Since we did not work with a particular
district hospital due to time constraint and the limited budget we have
consider the district hospital structure in Ghana as study setting, and the
information used at this step are based on existing literature as stated in the
background section of the work. The project management step plan correspond the
research study plan and the deliverable is the CPOE system.
At the end of this phase, the recommendation done to the
hospital management can be formulated in the terms of designing a Computerized
Provider Order Entry System for laboratoryorder management with notification
capabilities using SMS and Email.
5.4. The analysis phase
5.4.1. The existing
situation
According to the study, a district hospital with a manual and
paper laboratory based system constitute our study setting, and the aim of the
project is to create a new automated system for laboratory order management.
The loop-holes found in the manual system according to the literature reviews
are: inappropriate test request from clinician, error in patient identification
and specimen collection, failure in communicating laboratory result to both
patient and referring clinician (Plebani, 2010) and breaking in the workflow
communication process between clinical staff within the hospital
setting.(Maslove et al., 2011)
5.4.2. Improvements
identification
Based on the proposed framework for the district hospital
illustrate in the Figure1.1 (Chapter 1), we have identified five business
processes to automate for the improvement of the laboratory test order
management:
1. Patient administration management: provides patient
demographics information to the system. This process involves the management of
patient identification information such as names, record number, ID number and
patient location. The patient is uniquely identified with the medical record
number.
2. Staff administration management: provides basics
information on the profile of the medical staffs in terms of their working
categories or the duties they are supposed to perform to provide care to the
patient. The medical staff are identified by their professional identification
number such as license number.
3. Place order management: provides information on the
laboratory order requested by clinician for patients. Each order created by the
clinician should be identified with an Order Number.
4. Test result management: provides information on the
specimen collection for an order, their identification and management. Result
entry is also included in this process.
5. Order result management: provides information on the
follow-up and the tracking of the order result.
5.4.3. Requirements
definition
A requirement is simply a statement of what the system must
perform or what characteristics it should have. During a systems development
project, requirements are created to describe the business needs (business
requirements), what the software should do (functional requirements), the
characteristics that the system should have (nonfunctional requirements).
Business requirements
The business requirements are the statements that describe the
reasons for proposing the system development project. This section refer to the
justification of the study.
Functional
requirements
A functional requirement relates directly to a process that
the system has to perform to support the user tasks. The International
Institute of Business Analysis (IIBA) defines functional requirements as
«the product capabilities, or things that a product must do for its
users». By the analysis of main user tasks that should be performed from
the five business processes to be automated, the functional requirements listed
below have been identified.
§ Patient administration management:
The system will allow the clerk:
- To record new patients
- To subscribe the patient to receive notification of
laboratory result by SMS and/or e-mail
- To search a patient using his/her identification
information
- To update demographic information of the patient
- To view the list of the patient of the hospital
§ Staff administration management:
The system will allow the clerk:
- To record new medical staff
- To update identification information of the medical staff
- To view the list of the staff of the hospital
§ Place order management
The system will allow
- The clinician to request laboratories test for the
patient
- The clinician to choose to receive the lab result by SMS
and/or email
- The clinician to view the ordered laboratory group test for
a patient;
- The nurse to refer a patient to a clinician
- The nurse to view laboratory test request by the clinician
for a patient.
§ Test result management
The system will:
- Allow the laboratory technician to record the reception of
specimen;
- Allow the laboratory technician to identify the referring
clinician and patients;
- Allow the laboratory technician to record result of lab
test
- Allow the laboratory technician to record new external
laboratory order
- Send automatic SMS and/or email notification to both patient
and referring clinicianwhen the result are validated.
§ Order result management
The system will allow:
- The referring clinician to view the result of the lab tests
ordered
- The referring clinician to view laboratory test that have
been performed or not
- The referring clinician to enter treatment guideline for a
patient after viewing the lab result
- Any clinician who is authorized to access the system to view
lab order requested by another clinician and to enter treatment guideline
- Any clinician who is authorized to access the system to view
on the work station the alert notification of new results available
- The nurse to view the treatment guideline and the laboratory
test request for an identified patient and referring physician.
Nonfunctional
requirements
The IIBA defines the nonfunctional requirements as the quality
attributes, design, and implementation constraints, and external interfaces
which a product must have. The followings requirements have been identified:
§ Operational
Defines the physical and technical environments in which the
system will operate:
- The system should run on a PC (Windows 7 Operating system or
above, 1 Gb of RAM, and at least 1Gb of Hard Disc) used by medical and
administrative staff;
- The system should work in the existing wired or wireless
intranet network
- The system should use the existing internet connection
- The system should use available GSM network for SMS
notification
§ Performance
- The system should support 5 users in minimum
- The system should allow to resend notification when the GSM
network or the internet network is down.
§ Security
- No clinician can cancel the laboratory order requested by
another clinician
- Only the referring clinician can choose to be notified by
e-mail and SMS
- The patient should give his/her agreement for being notified
by e-mail and SMS when the laboratory result is available
- Laboratory test details should be sent to the clinician
only, the patient receive just the notification on the availability of the
result
§ Cultural and political requirement
- Patient medical record information should be protected by
local or regional law related to Data Protection Act
- Policy on confidentiality and privacy of the patient record
should be implemented and disseminated prior to the system deployment
5.5. System design
The following step consist on the technical modelling of
therequirements. In engineering discipline model is crucial and is used to
describe the shapes or actions of any construction that must be built. The
benefits of the model are the requirement clarification and performance of a
construction. The main objectives of design model is to support system
complexity and reduce the error in the software development processes.(Ali,
Shukur, & Idris, 2007)
5.5.1. System
Architecture
In the study the client-server architecture is the base system
architecture, since it attempts to balance the processing between client
devices and one or more server devices. In the client-server architecture, the
client is responsible for the presentation logic, whereas the server is
responsible for the data access logic and data storage.(Dennis et al., 2012) We
will use thick or fat client approach wherethe client contains most of the
application logic and the server contains the data repository so the proposed
system will be a stand-alone application.

Figure 3.2: System architecture
5.5.2. The process
modelling
Unified Modeling Language `(UML) is increasingly used as the
standard for software modelling and design. The most recent version (UML 2.0
under OMG 2004) includes 13 distinct modelling notations ranging from
high-level use case diagrams, which illustrate the scenario of the interactions
between actors and major business tasks, through to low-level object diagrams
which capture instances of individual data objects. The various modelling
notations are essentially divided into three main views: the behavior, the
structure and the interaction views.(Russell, Aalst, Hofstede, & Wohed,
2006)
The behavior views contains diagrams that describe the set of
functionality of the software at a relatively high level of abstraction. The
structure view, contains diagrams that capture the data structure of objects
involve in task performance. And, the interaction view contains diagrams that
illustrate the interactions between objects involve in the execution of a
business function.(Blanc & Mounier, 2006)
Activity Diagrams
The activity diagram notation is the most detailed form of
flowmodelling within UML. (Russell et al., 2006)Activity modeling focuses on
the execution and flow of the behavior of a system.It will be used to represent
the workflow of laboratory order process in the district hospital according to
the framework of CPOE system in Figure 1.1.
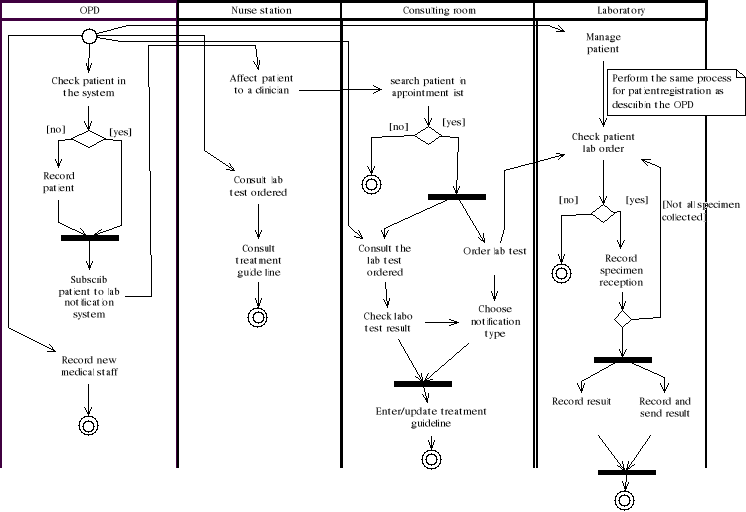
Figure3.3: Activity diagram
Use case diagrams
Since one of the goals in the systems development project is
to create usable software, it is important to clearly determine the user's
needs. Use cases help to understand and clarify the users' required
interactions with the system by illustrating the interactions between users and
business function to perform an activity in the workflow process. (Dennis et
al., 2012) To allow the better view of the use case diagram we will split the
use case diagram into three subsystem:
1. The authentication subsystem
2. The patient and medical staff management subsystem
3. The laboratory order management subsystem
4. The laboratory result management subsystem
 Figure 3.4: Use case diagram for authentication
subsystem Figure 3.4: Use case diagram for authentication
subsystem
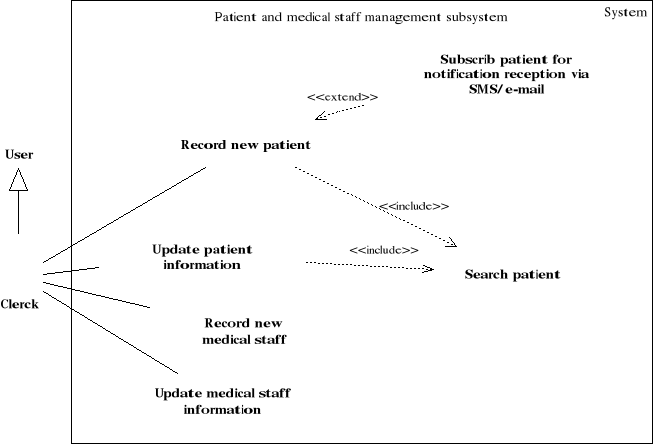
Figure3.5: Use case diagram for patient and medical
staff management subsystem
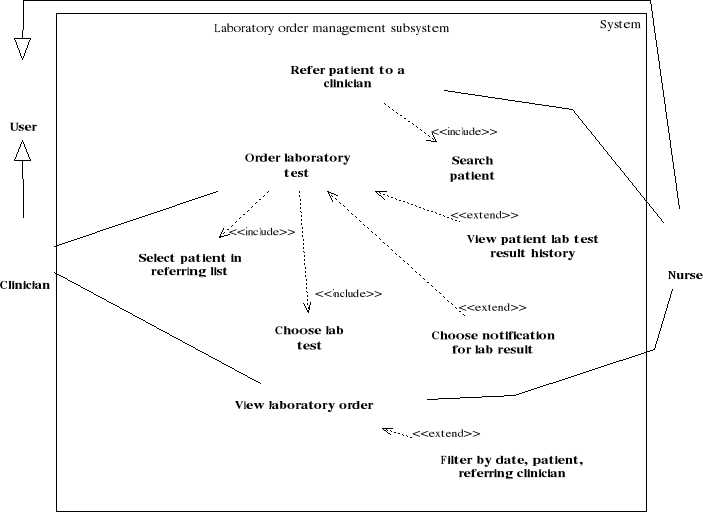
Figure 3.6: Use case diagram for the laboratory test
order management subsystem
 Figure 3.7: Use case diagram for the laboratory test result
management subsystem Figure 3.7: Use case diagram for the laboratory test result
management subsystem
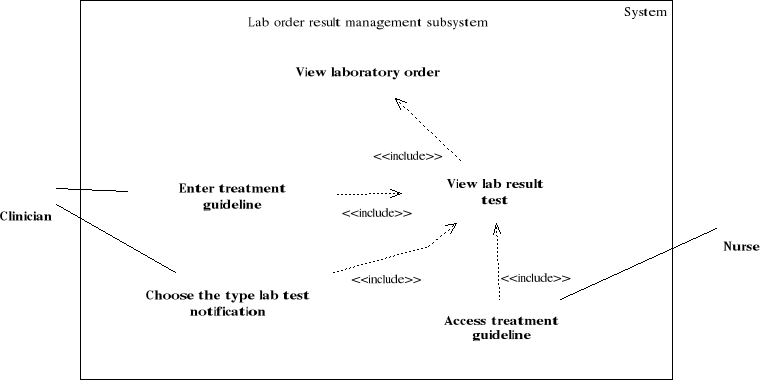
Figure3.8: Use case diagram for the lab order result
management subsystem
Class diagrams
The structure view of UML language is the most used to specify
an application requirements. The main objective of this view is to model the
structure of different classes of an object oriented (OO) application and their
interaction.(Blanc & Mounier, 2006)The main building block of a class
diagram is the class, which stores and manages information in the system. The
classes refer to the people, places, events, and things about which the system
will capture and process data. Later, during coding phase, classes can refer
also to coding-specific component like windows, forms, and other objects used
to construct the system.(Dennis et al., 2012)
To make the diagrams easier to read and keep the models at a
reasonable level of complexity, the classes is grouped into packages. In our
diagrams, only mains attributes are illustrates to make the diagram as simple
as possible and classes methods are not illustrates since they are more useful
during the coding phase. We will devise the class diagram to three package:
1. The user management package
2. The location package
3. The laboratory order and result management package
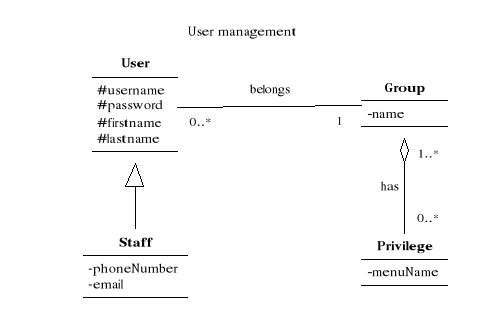
Figure3.9: Class diagram for the user's management
package
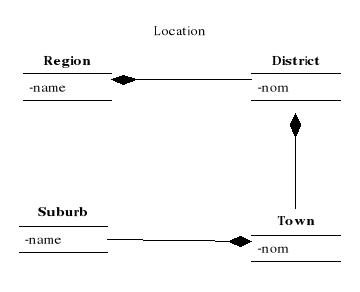
Figure3.10: Class diagram for the location
package
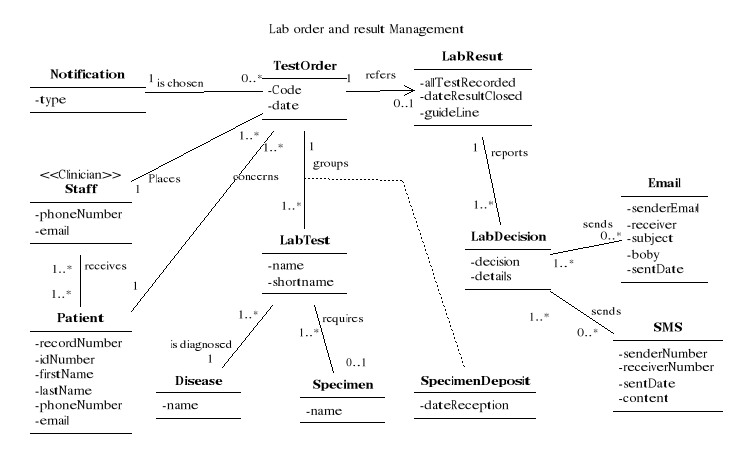
Figure3.11: Class diagram for the order and result
management package
Sequences diagrams
The behavioural aspect of an OO application is defined by the
way the objects of the system are interacting between them. The execution of
the program is essentially the exchange of the messages between application
objects to perform a particular treatment. (Blanc & Mounier, 2006)Since
sequence diagrams emphasize the time-based ordering of the interactions that
takes place among a set of objects, they are very helpful for understanding
real-time specifications and complex use cases.(Dennis et al., 2012)
We will focus on sequence diagrams of the most important use
cases to make our design simple: Order laboratory test and record laboratory
test result. The others sequences diagrams are also important but they will not
be illustrated to simplify the process modelling as they are more related to
the coding of system features.
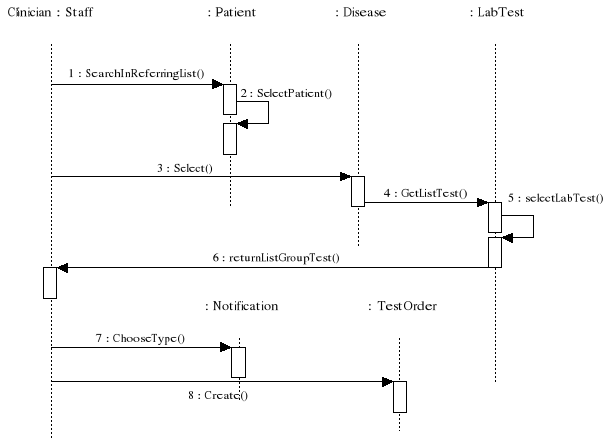
Figure3.12: Sequence diagram for order laboratory test
scenario
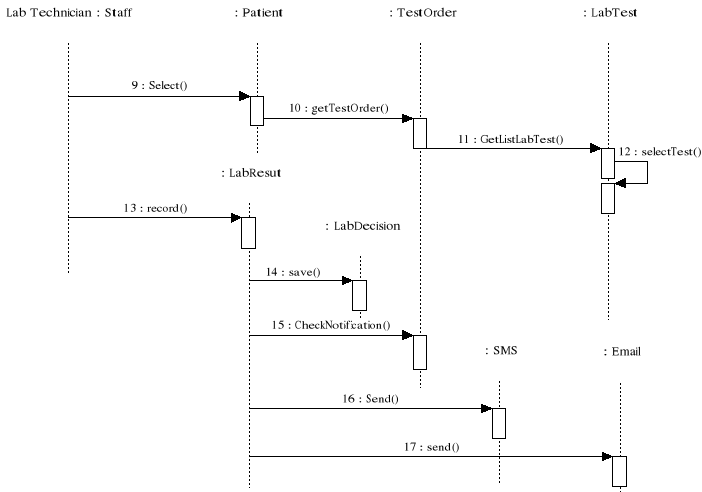
Figure3.13: Sequence diagram for record lab test
result scenario
5.5.3. The data
modelling
The data model presents the logical organization of data
without indicating how the data are stored, created, or manipulated. Entity
relationship (ER) diagram will be used for the data model.(Dennis et al.,
2012)The database modelling approach in the study, will be based on the three
main phases of the database design methodology: conceptual, logical, and
physical database design.
Conceptual data design
The conceptual data design is the process of constructing a
model of the data independent of all physical considerations. This process
involve building the first ER diagram based on the functional requirements. The
following steps are used in the conceptual data modelling: (CONNOLLY &
BEGG, 2005)
§ Entity identification: In this step, we have identified
the main objects that the users are interested in, based on business and
functional requirements. The attributes of each entity are also identified.
§ Attribute domain determination: A domain is a pool of
values for an attributes. The objective of this step is to determine domains
for all the attributes in the model. Simple, composite, single, multi-valued,
and derived attributes are also identified.
§ Relationship identification: we search for the
relationship that exist between entities and we determine the cardinality
constraints for each relationship. The cardinality constraints are used to
check and maintain data quality since it precises how many instances of each
entity participate in the relationship.
§ Design the first ER diagram showing entity and their
relationship
The figure 3.15 below shows the first ER diagram. The
different attributes of the entities are listed in the table 3.3.
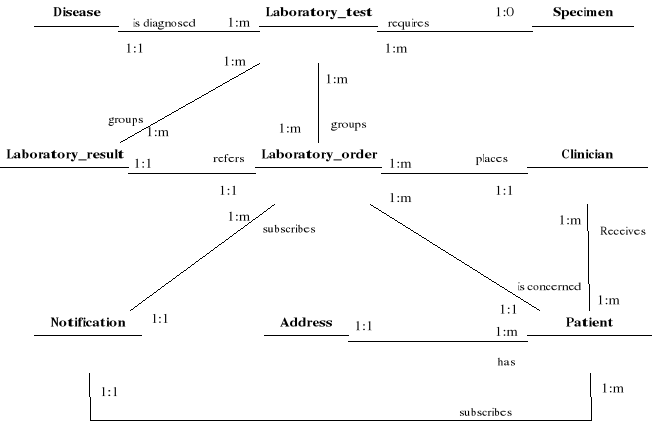
Figure 3.14: First ER diagram
|
N°
|
Entity set
|
Attribute name
|
|
1
|
Disease
|
Name
|
|
2
|
Laboratory_test
|
Name
Description
|
|
3
|
Specimen
|
name
|
|
4
|
Patient
|
Id number
Names
Date of birth
Sex
Phone
email
|
|
5
|
Clinician
|
Names
License number
Phone
email
|
|
6
|
Address
|
Suburb
Town
District
Region
|
|
7
|
Notification
|
Type
|
|
8
|
Laboratory order
|
Date of order
Date reception specimen
|
|
9
|
Laboratory result
|
Date of final result
Date notification clinician
Date notification patient
Treatment guideline
|
Table3.3: List of attributes of
the first ER diagram
Logical data design
The logical data model provides the physical database designer
with a vehicle for making tradeoffs that are very important to the design of an
efficient database. The main objective is to translate the conceptual data
model into a logical data model and, then to validate this model bychecking
whether it is structurally correct and able to support the required
transactions. The following steps are used in the logicaldata modelling:
(CONNOLLY & BEGG, 2005)
§ Relationship derivation for logical data model: We
identify many to many relationships to derive new entity followed by foreign
key identification. At this step parent and child entities are determined to
manage the foreign key mechanism.
§ Normalization: The purpose of normalization is to
ensure that the set of relations has a minimal and yet sufficient number of
attributes necessary to support the data requirements of the enterprise.The
relations should have minimal data redundancy to avoid the problems of update,
delete and insert anomalies. The third Normal Form (3NF) rules has been chosen
as sufficient level of optimization of the database schema.
After going through the conceptual and logical design, we have
obtained the final ER diagram shown in the Figure 3.16 below, only primary and
foreign keys will be represented to make the diagram simpler, other attributes
are illustrated in the Table3.4.

Figure 3.15: Final ER diagram
|
N°
|
Entity set
|
Attribute name
|
|
1
|
Disease
|
Disease id
Name
|
|
2
|
Laboratory_test
|
Test id
Name
Description
Specimen id
|
|
3
|
Specimen
|
Specimen_id
Name
|
|
4
|
Patient
|
Patient_id
Id number
First name
Las tname
Date of birth
Sex
Phone
email
Notification_id
|
|
5
|
Clinician
|
Clinician_id
Licence_number
Firstname
lastname
Phone
email
|
|
6
|
Referring_list
|
Clinician_id
Patient_id
date
|
|
7
|
Suburb
|
Suburb_id
name
|
|
8
|
Town
|
Town_id
name
|
|
9
|
District
|
District_id
name
|
|
10
|
region
|
Region_id
name
|
|
11
|
Notification
|
Notification_id
type
|
|
12
|
Laboratory_order
|
Order_id
Clinician_id
Patient_id
Date
Notification_id
date_of_order
|
|
13
|
Order_test_list
|
Order_id
Test_id
Date_specimen_reception
|
|
14
|
Laboratory_result
|
Lab_result_id
Order_id
Date of final result
Treatment guideline
|
|
15
|
Result_test_list
|
Result id
Test id
Date notification clinician
Date notification patient
notes
|
Table3.4: List of attributes of
the final ER diagram
Physical data design
The physical design translate the logical data model for
target Relational Database Management System (RDBMS) to produce a relational
database. After selecting the RDBMS on which the relational database will be
implemented, the main step in logical design is the definition of different
relations using the Data Base Definition Language (DBDL). A relational database
is principally the collections of tables, each of which has a primary key, and
in which the tables are related to each other by the placement of the primary
key from one table into the related table as a foreign key. (Dennis et al.,
2012). As the DBDL is more related to the implementation of database relations
in the RDMS, we will not illustrate the Structured Query Language (SQL)
definition of each relation in PostgreSQL since the main objective of the DBML
is to implement the entity in the RDMS.
CHAPTER 4
4. SYSTEM DEVELOPMENT
The development or the coding phase has been performed using
two mains tools: the Visual Studio 2010 IDE and PostgreSQL 9.0. Visual Studio
2010 was used for the programming of the client side (front end) of system
using the C# programming language. The physical design step of the database was
performed using SQL over PostgreSQL RDMS. The GSM modem is connected on the
Universal Serial Bus (USB) port of the PC that will be used to send the alert
and notification, according to the workflow the GSM modem can be installed
either on the lab computer or on the clerk work station.
The CPOE is designed to meet the system requirement of lab
order management within a district hospital in Ghana. It hasseven functional
modules:
1. The users and system administration module
2. The medical staff management module
3. The patient management module
4. The appointment and consultation module
5. The laboratory test order management module
6. The laboratory test result management module
7. The report module
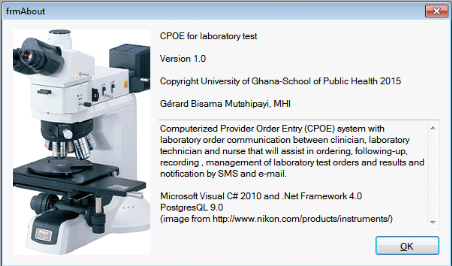
Figure 4.1:The CPOE system information form
4.1. The users and system administration module
To access the system, the user should have a valid user name
and password. The user is created by the system administrator. The system
administrator is a super user and his account is created during the system
installation. The user of the system are physician, nurses and administrative
staff. To access the system any staff member should be first registered in the
system.
The first task of the system administrator is to register the
medical staff and to associate a credentials (user name and password) to them.
During the user creation, the system suggest a username and generate randomly a
password for each associated staff. Those credentials should be communicated to
each user by the system administrator and then the user can change the
generated to ensure the security of their account. Each user should be assigned
to the group system which is associated to a collection of features that a user
can access in the system. So each user access only the information associated
to his role within the organization. By this mechanism the system ensure the
confidentiality of the patient information. The user registration and
management processes are shown in figures 4.2 to 4.5.
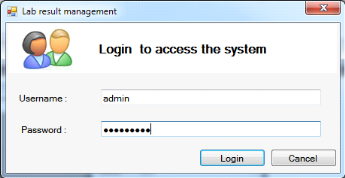
Figure 4.2: System login form
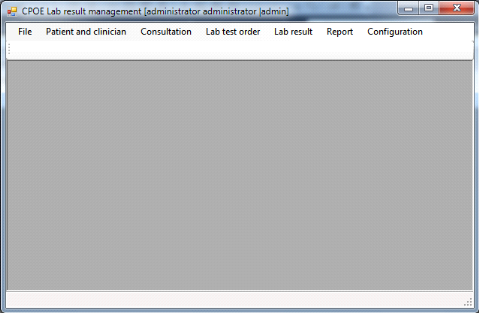
Figure 4.3: Main form of the system
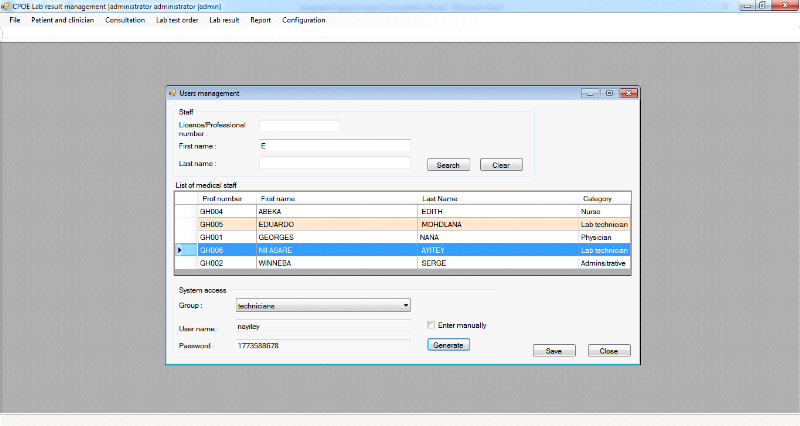
Figure 4.4: Users security system access
configuration
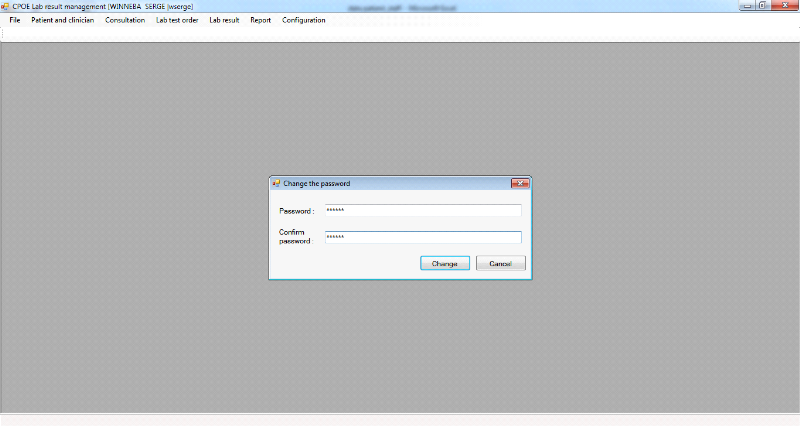
Figure 4.5: User change password form
4.2. The medical staff management module
All staff should be first registered prior of being associated
to a credential. Medical personnel like physician, nurses and laboratory
technicians will provide their license number that will serve as their primary
identification. For other administrative categories, they will provide their
national identification number (ID) or any other type of identification number.
Phone numbers and e-mails are not required for all group of system users but
for the purpose of receiving laboratory notification, clinicians are required
to provide their cell phone numbers and/or email to be able to subscribe to SMS
and email notification of laboratory result (Figure 4.6).
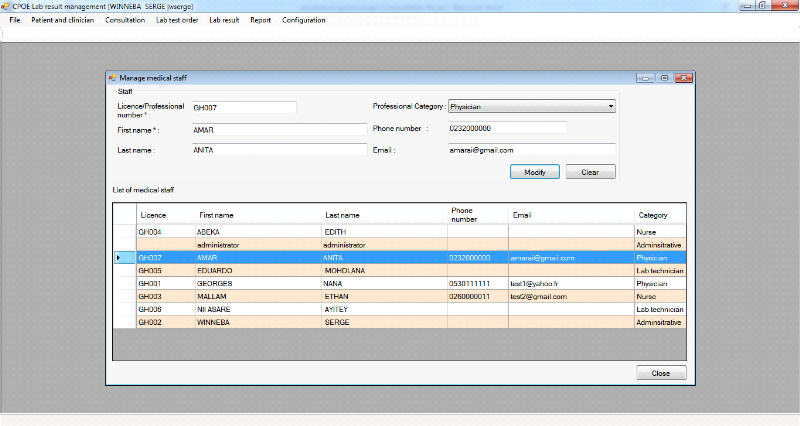
Figure 4.6:Medical staff personal details
registration
4.3. The patient management module
During the patient registration the national ID number can be
entered if available. The system generate for each patient a new record number
to allow identification for patients without the national ID numbers. For the
purpose of receiving the laboratory notification by SMS and/or email, the phone
number and e-mail information should be entered in the system after the patient
subscription. To prevent the duplication of the patient information, the system
have a search module that uses multi criteria variables to check if the patient
is already in the system prior to his registration. The patient registration
processes are shown in Figure 4.7 and Figure 4.8
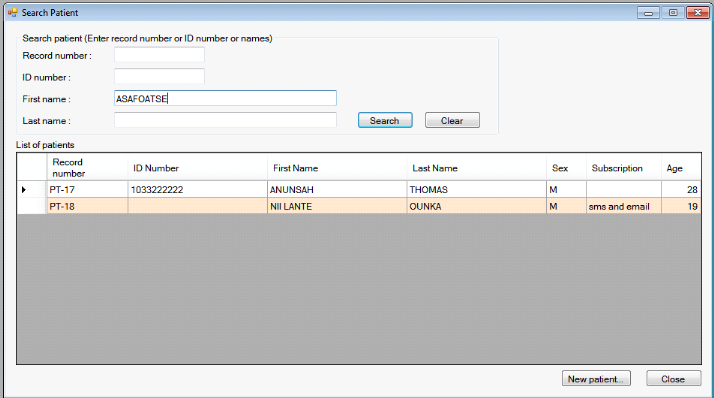
Figure 4.7: Patient search form
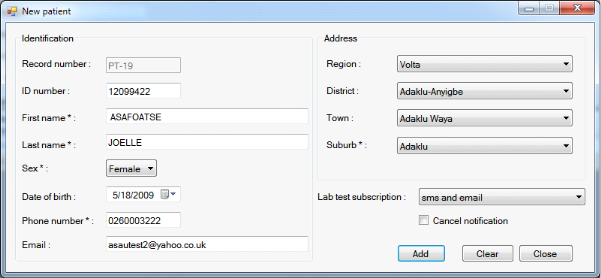
Figure 4.8: Patient registration form
4.4. The appointment and consultation module
Before having access to the consulting room to see a physician
the patient should be received at the nurse station and then being assigned to
the right clinician according to his/her case (Figure 4.9).
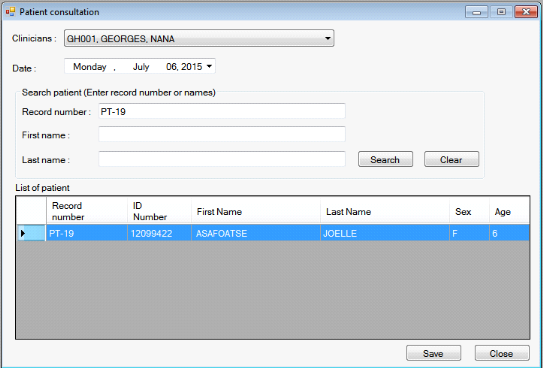
Figure 4.9: Patient assignment to clinician
3.1. The laboratory test order management module
After assigning a patient to a physician for the consultation,
the physician can only order a group of lab test for the patients that are
assigned only to him. During this step, the physician can decide to receive the
laboratory test results by SMS or e-mail. A laboratory test order can contain
many tests and the system issue a lab order number to allow unique
identification of the test order. The physician can also track his orders or
the lab orders requested by other clinicians. The figures 4.10 to 4.11
illustrate the lab order management process.
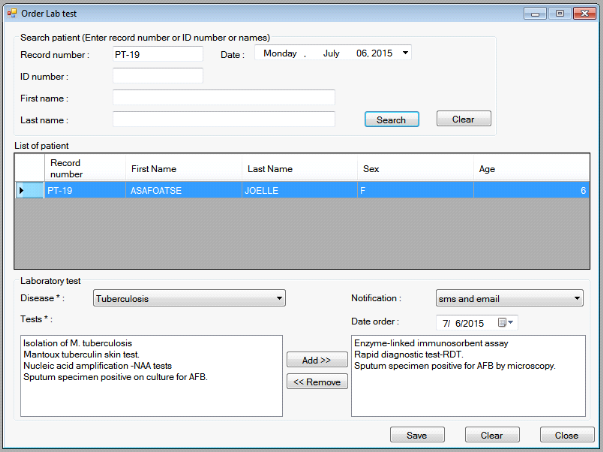
Figure 4.10: Laboratory test group order for a
patient.
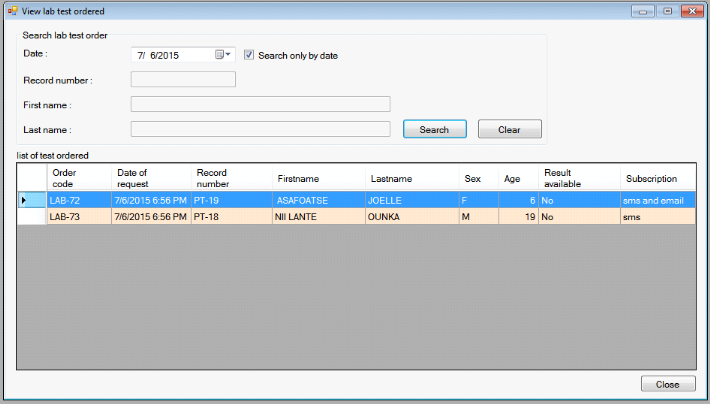
Figure 4.11: List of order place by a
clinician
4.5. The laboratory test result management module
After requesting order for the patient by the clinician during
the consultation. The Laboratory technician can consult the requested lab
orders and record the information on specimens deposit, and enter the lab
result for each tests performed. As all test cannot be done at the same time,
for example the RDT for malaria comparing with to the culture of sputum test
which can take more time, the laboratory technician can decide during the
record of test results to send notification for only one or a group of test, or
to send the notification after all test has been performed (Figure 4.12 to
4.18). To send notification by SMS, a GSM modem should be connected to the work
station reserved for that. For the e-mail notification, the system should be
also be connected to an internet network. If one of the connections is not
available, an error message appears at the status bar to inform the user on the
absence of the connection. But the network problem does not prevent the result
to be saved in the system.
The system also allow the message to be send/resend later if
necessary, since the email or the SMS could not reach the clinitian or the
patient due to the network provider service errors (Figure 4.19). The clinician
can consult the result for each lab order requested at the workstation and give
the treatment guide line for the patient which can also be viewed by the
nurses. The clerk or the administrative personnel can also check if the lab
result of the patient is available or not, without accessing to the details of
the laboratory test which are exclusively reserved to medical personnel. When
some results are available the system show a message at the status bar to alert
the clinician.
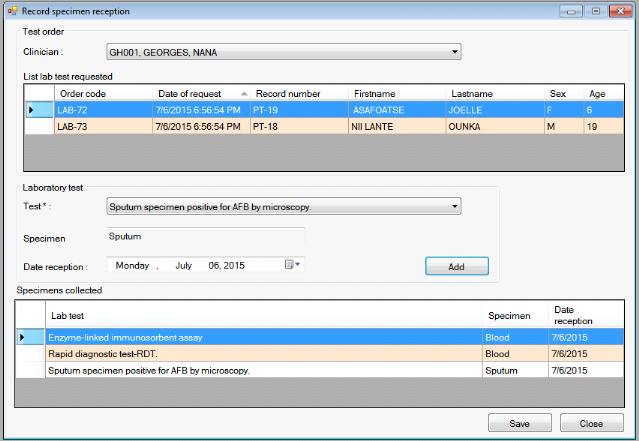
Figure 4.12:Laboratory specimen deposit record
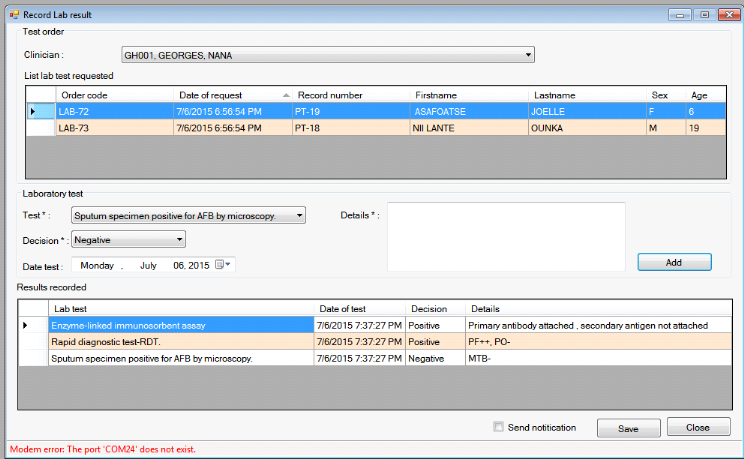
Figure 4.13: Lab result record and
notification
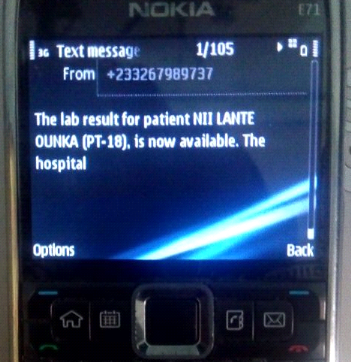
Figure 4.14: SMS lab result notification format for
the patient
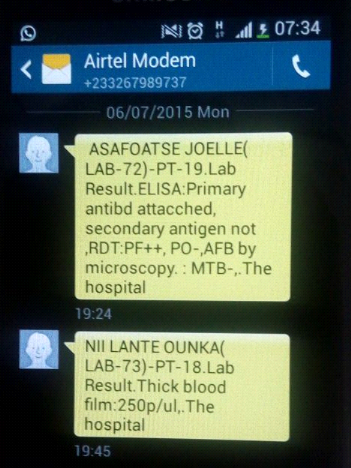
Figure 4.15: SMS lab result notification format for
the clinician
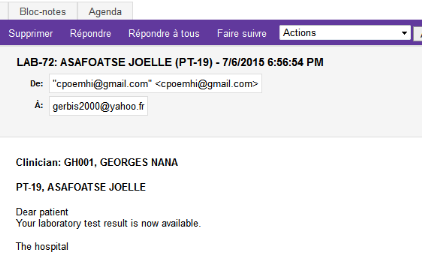
Figure 4.16: E-mail lab notification format for the
patient
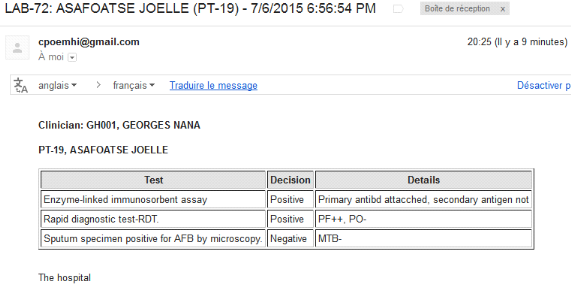
Figure 4.17: E-mail lab result notification format for
the clinician
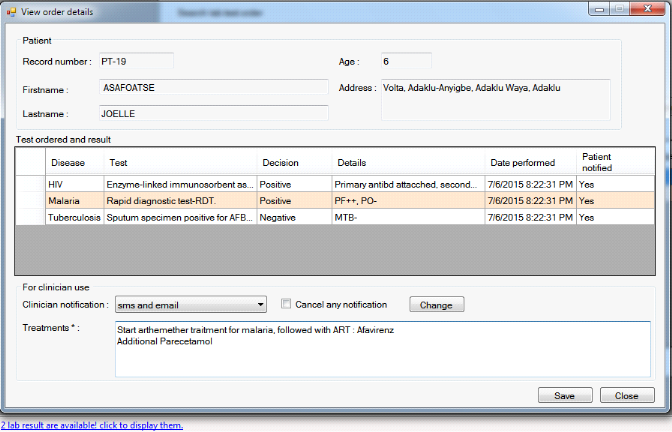
Figure 4.18: Lab result view and treatment
registration form
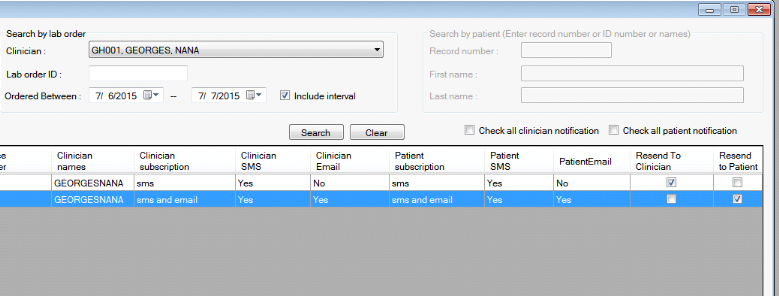
Figure 4.19: Resend of lab result notification to
patient and/or clinician
4.6. The report module
The report module provide the laboratory history and treatment
guideline for a specific patient across the time. It provides detailed
information on all lab exam requested, the clinicians in charge, the result of
the lab test as well as patient detailed information. This report can be
exported in word, excel and pdf document format. Additional report on such as
the case-based surveillance report form and the notifiable disease report form
are also produced. (Ministry of Health of Ghana, 2002)
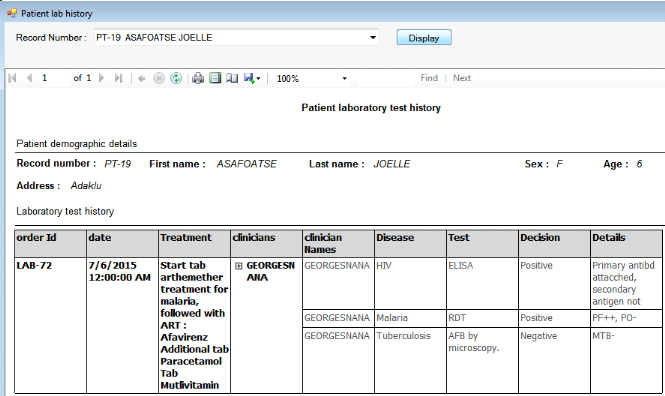
Figure. 4. 20: Patient lab history report
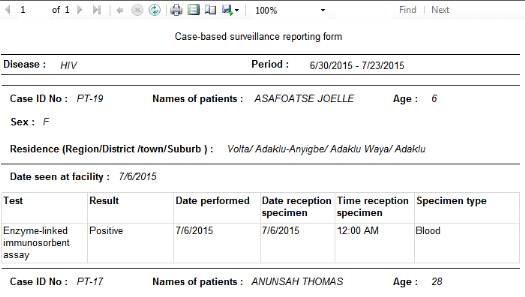
Figure. 4. 21:Case-based
surveillance reporting form
CHAPTER 5
5. DISCUSSION
The CPOE for laboratory test management design provides
capabilities to clinician to automate the order of lab test and performed the
follow up of the result in a district hospital. The automation of the pre and
post diagnostics task reduces errors such as identification of patient and
specimen, redundant ordered test, lost to follow up.
According to the proposed framework which is based on the HIE
laboratory order schedule workflow, the CPOE as the hub of lab order system
ensures a improvement in workflow by establishing the connection between the
patient management system, the medical history management of patient within the
clinical services and the laboratory order in a centralized architecture.
By using SMS and email notification of laboratory result, the
patient communication experience is improved as well as the referring
clinician, since they can receive respectively the notification and the result
of the laboratory tests on their phone and by email.
5.1. The design consideration
After conducting a literature review of main topic related to
our study subject, we have found that the lack of health information system
integration in the clinical workflow and the clinical relationship between
services has been cited as one of the main raison of abandonment of a medical
record after his deployment. (Maslove et al., 2011)
To take into account this limitation observed in others study
on the design HIS, we first start our study by identifying the important
workflow in data exchange between clinical services and the main actors
involved in lab order management. We analyzed the circulation of information
between the outpatient department, the laboratory service and other clinical
services prior to the identification of system business requirements. Business
process management approach has been used to identify different actors involved
in the circulation of information and the tasks to automate. We think that this
methodology provide the system more flexibility to be integrated in the
hospital workflow and to introduce organization change without breaking
communication between actors.
5.2. Benefits of the system
- The CPOE provide clinicians at the district hospital with a
tools to easily order a group of laboratory test for a patient with a
relatively simple users friendly interfaces where most of the task are
selection based.
- The CPOE allows the clinician to perform the follow up of
the laboratory test by visualizing the test that has been performed and those
in pending status.
- Provide laboratory service in the district hospital with a
tools to organize and managed all the result as well as specimen reception
information on patient.
- The CPOE has the potential to enhance clinician'sawareness
of the patient situation by receiving alert and notification of the laboratory
result on the mobile phone and by email.
- The CPOE has the potential to improve patient communication
experience with the district hospital by receiving by SMS and email
notification when the lab result is available.
- The system use the existing GSM network for SMS notification
instead of internet API that make it most adaptable at limited setting area
where the internet access is a challenge.
5.3. Limitation
Despite of the benefits of the CPOE system, the study has some
limitations. We can cite:
- The feasibility study was not conducted on the field to get
real input on a district hospital using data collection technique like a
structured-interview. We have based our system and user requirement on existing
literature.
- Due to the time constraint the implementation of the system
on the field could not be conducted as well as the system assessment to get
users feedback
- The system used synchronous mode to send notification of SMS
and e-mail, that can create a delay with a relative long time of waiting when
sending the notification if the GSM network and the internet connection are not
good.
- To view the patient treatment guide line, the nurse has to
access the computer. Knowing that they are moving within the ward to provide
treatment to patient, this module should be deployed on mobile device such as
mobile phone or pocket PC and linked to the system through the wireless
intranet network.
5.4. Future works
Several work can be done in future to make the system more
efficient.
System interoperability
To allow the system to be very scalable and allow the exchange
of information with others system (OpenEMR, DHIS2), we have planned to use HL7
data exchange standard for communication between the client and the server
instead of simple SQL request based. With data exchange standard new module
(web or mobile) client can be added and deployed easily without the need to
reinstall or update the all client and server module.
New nurse interface module
The nurse has to be connected on the workstation to view
patient laboratory treatment guideline which is not a very friendly solution.
We have planned to develop a mobile application for cell phone or pocket PC
that will allow the nurses to access patient treatment guideline anywhere in
the hospital.
New specimen identification module
To allow an efficient identification of the specimen bring by
the patient, we have plan to update the specimen deposit feature in such a way
that a the patient ID and the associated bar code can be print and paste to the
specimen container to avoid physical error in patient identification.
CHAPTER 6
6. CONCLUSION AND RECOMMENDATION
7. Conclusion
Information and Communication technologies (ICT) used to
manage, generate and communicate health-related information have been widely
proved to be used as the way to improve the quality, safety, and efficiency of
health care delivery in both developed and developing countries. Health
Information Technologies tools provide a significant enhanced capabilities to
the traditional manual system. (Maslove et al., 2011)
Some common challenges has been recognized as obstacles to the
success of the implementation of the electronic medical record like the limited
computer literacy among the medical practitioners, lack of unique
identification numbers for patient, lack of skilled health information system
analyst. (Blaya et al., 2006) But a very important aspect to take into account
when a health information system is designed, is the integration in the
clinical workflow between services and the clinical relationship between
actors. (Maslove et al., 2011).
We have developed a computerized provider order entry system
for laboratory order data management that take into account the workflow of
information related to the laboratory data within a district hospital to help
the hospital to manage efficiently and effectively data related to laboratory
test. Adding the SMS and the e-mail notification of laboratory result to both
patient and clinician have the purpose to improve their communication
experience.
This study is the initial step of building a CPOE for the
district hospital in Ghana, we believe that the developed system will allow
medical staff in the district hospital to improve the laboratory order
management and provide satisfaction to patient.
5.5. Recommendation
To implement the system and get full benefits of it, the
following recommendations are necessary for the health informatician
(implementation team), the hospital administration and other health related
institutions:
1. The hospital administration and the implementation team
should plan a working meeting that will involve the laboratory techniciansand
the physicians, to identify the practical terminology used on the field to
order and record laboratory test, and map them to the standard terminology used
in the system, to allow smooth introduction and use of the system.
2. The hospital administration and the medical staff should
put in place a team to decide on the format and the content of information send
by email and SMS, to both patient and medical staff ;
3. The hospital administration should put in place a security
policy to ensure confidentiality of data inside and outside the clinical
setting, by implementing a Security Education Training and Awareness Program
(SETA) for both patient and medical staff. National Institute of Standards and
Technology (NIST) Special Publication (SP) 800-50 can be used to design and
implement the security program and it should be based as possible on National
Data Protection Acts.
4. The hospital should acquire a network environment
(wireless or wired) to get the full benefit of the system and, appoint a
network and system administrator to provide technical support in the health
facility.
5. Since the system used bulk SMS technology, the
implementation team should contact a GSM provider to allow the hospital to
acquire a short telephone number format and optimize the time out of SMS to
avoid the lost laboratory notification message with SMS.
Reference
Ali, N. H., Shukur, Z., & Idris, S. (2007). Assessment System
For UML Class Diagram Using Notations Extraction, 7(8), 181-187.
Allen, C., Jazayeri, D., Miranda, J., Biondich, P. G., Mamlin, B.
W., Wolfe, B. a, ... Fraser, H. S. F. (2007). Experience in implementing the
OpenMRS medical record system to support HIV treatment in Rwanda. Studies
in Health Technology and Informatics, 129(Pt 1), 382-386.
Blanc, X., & Mounier, I. (2006). UML2 pour les
développeurs. (Eyrolles, Ed.) (1ère Editi.).
Blaya, J. A., Shin, S. S., Yagui, M. J. A., Yale, G., Suarez, C.
Z., Asencios, L. L., ... Fraser, H. S. F. (2006). BMC Medical Informatics and A
web-based laboratory information system to improve quality of care of
tuberculosis patients in Peru?: functional requirements , implementation and
usage statistics, 11, 1-11. doi:10.1186/1472-6947-7-33
Callen, J., Georgiou, A., Li, J., & Westbrook, J. I. (2011).
The safety implications of missed test results for hospitalised patients: a
systematic review. BMJ Quality & Safety, 20(2), 194-9.
doi:10.1136/bmjqs.2010.044339
Caminero, J. (2005). Drug-susceptibility testing in tuberculosis:
methods and reliability of results, 25(1), 564-569.
doi:10.1183/09031936.05.00111304
CDC. (2012). Menu of Suggested Provisions For State Tuberculosis
Prevention and Control Laws. Retrieved May 18, 2015, from
http://www.cdc.gov/tb/programs/laws/menu/laboratory.htm
CDC. (2014a). Malaria Diagnosis (U.S.) - Rapid Diagnostic Test.
Retrieved May 18, 2015, from
http://www.cdc.gov/malaria/diagnosis_treatment/rdt.html
CDC. (2014b). Tuberculosis (TB) testing and diagnosis. Retrieved
May 18, 2015, from http://www.cdc.gov/tb/topic/testing/
CDC. (2015a). National Notifiable Diseases Surveillance System
(NNDSS) - Tuberculosis (TB) (Mycobacterium tuberculosis). Retrieved May 18,
2015, from
http://wwwn.cdc.gov/nndss/conditions/tuberculosis/case-definition/2009/
CDC. (2015b). National Notifiable Diseases Surveillance System
(NNDSS)-Malaria (Plasmodium spp.). Retrieved May 18, 2015, from
http://wwwn.cdc.gov/nndss/conditions/malaria/case-definition/2014/
CONNOLLY, T. M., & BEGG, C. E. (2005). Database
systems. (Pearson Education, Ed.) (4th Editio.). Pearson Education.
Dennis, A., Wixom, B. H., & Roth, R. M. (2012). Systems
analysis and design. (Wiley, Ed.) (5th Editio.).
Elder, N. C., Mcewen, T. R., Flach, J., Gallimore, J., &
Pallerla, H. (2010). The Management of Test Results in Primary Care?: Does an
Electronic Medical Record Make a Difference??, 42(5).
Ghana Health Service. (2015). Regional and District
Administration. Retrieved July 8, 2015, from
http://www.ghanahealthservice.org/ghs-subcategory.php?cid=2&scid=44
Hao, W.-R., Hsu, Y.-H., Chen, K.-C., Li, H.-C., Iqbal, U.,
Nguyen, P.-A., ... Jian, W.-S. (2015). LabPush: a pilot study of providing
remote clinics with laboratory results via short message service (SMS) in
Swaziland, Africa - a qualitative study. Computer Methods and Programs in
Biomedicine, 118(1), 77-83. doi:10.1016/j.cmpb.2014.10.005
Huerta, T. R., Thompson, M. a., Ford, E. W., & Ford, W. F.
(2013). Implementing electronic lab order entry management in hospitals:
Incremental strategies lead to better productivity outcomes. International
Journal of Information Management, 33(1), 40-47.
doi:10.1016/j.ijinfomgt.2012.05.008
Jiagge, G. N. (2007). A laboratory reporting system for the
trust hospital laboratory. (University of Ghana, Ed.) (University.).
University of Ghana, School of Public Health.
Johnson, D. L., Pejovic, V., & Belding, E. M. (2011). Traffic
Characterization and Internet Usage in Rural Africa. Proceedings of the
20th International Conference Companion on World Wide Web, 493-502.
doi:10.1145/1963192.1963363
Kimble, C. (2014). Electronic Health Records?: Cure-all or
Chronic Condition??, 33(4), 63-74. doi:10.1002/joe.21554
M'ikanatha, N. M., Lynfield, R., Beneden, C. A. Van, & Valk,
H. de. (2013). Infectious Disease Surveillance. Wiley-Blackwell.
Macleod, B., Phillips, J., Stone, A. E., Walji, A., &
Awoonor-Williams, J. K. (2012). The Architecture of a Software System for
Supporting Community-based Primary Health Care with Mobile Technology: The
Mobile Technology for Community Health (MoTeCH) Initiative in Ghana. Online
Journal of Public Health Informatics, 4(1), 1-17.
doi:10.5210/ojphi.v4i1.3910
Maslove, D. M., Rizk, N., & Lowe, H. J. (2011). Computerized
physician order entry in the critical care environment: a review of current
literature. Journal of Intensive Care Medicine, 26(3),
165-71. doi:10.1177/0885066610387984
McPherson, R. A., & Matthew R. Pincus. (2011). Henry's
Clinical Diagnosis and Management by Laboratory Methods. (Saunders, Ed.)
(22 nd.).
Ministry of Health of Ghana. (2002). Technical guidelines for
Integrated Disease Surveillance and Response in Ghana.
MOH Ghana. (2009). WHO pharmaceutical situation assessment -
level II - health facilities survey in Ghana. Retrieved from
http://www.moh-ghana.org/UploadFiles/Publications/Ghana_baseline_WHO_level_II_Health_Facility_Survey140204075637.pdf
Overhage, J. M., Grannis, S., & McDonald, C. J. (2008). A
comparison of the completeness and timeliness of automated electronic
laboratory reporting and spontaneous reporting of notifiable conditions.
American Journal of Public Health, 98(2), 344-50.
doi:10.2105/AJPH.2006.092700
Parsons, J. J., & Oja, D. (2014). New Perspectives on
Computer Concepts 2014: Comprehensive. (C. Learning, Ed.). Learning,
Cengage.
Plebani, M. (2009). Exploring the iceberg of errors in laboratory
medicine. Clinica Chimica Acta, 404(1), 16-23.
doi:10.1016/j.cca.2009.03.022
Plebani, M. (2010). The detection and prevention of errors in
laboratory medicine. Annals of Clinical Biochemistry, 47(Pt
2), 101-10. doi:10.1258/acb.2009.009222
POON, E. G., KUPERMAN, G. J., FISKIO, J., & BATES, D. W.
(2002). Real-time Notification of Laboratory Data Requested by Users through
Alphanumeric Pagers, 9(3), 217-222.
Ragunath, P. K., Velmourougan, S., Davachelvan, P., Kayalvizhi,
S., & Ravimohan, R. (2010). Evolving A New Model ( SDLC Model-2010 ) For
Software Development Life Cycle ( SDLC ), 10(1), 112-119.
Russell, N., Aalst, W. M. P. van der, Hofstede, A. H. M. ter,
& Wohed, P. (2006). On the Suitability of UML 2 . 0 Activity Diagrams for
Business Process Modelling *. Australian Computer Society,
53, 95-104.
Siedner, M. J., Haberer, J. E., Bwana, M. B., Ware, N. C., &
Bangsberg, D. R. (2012). High acceptability for cell phone text messages to
improve communication of laboratory results with HIV-infected patients in rural
Uganda: a cross-sectional survey study. BMC Medical Informatics and
Decision Making, 12(1), 56. doi:10.1186/1472-6947-12-56
Spahni, S., Lovis, C., Ackermann, M., Mach, N., Bonnabry, P.,
& Geissbuhler, A. (2007). Securing chemotherapies: fabrication,
prescription, administration and complete traceability. Studies in Health
Technology and Informatics, 129(Pt 2), 953-957.
WHO. (1999). WHO Recommended Surveillance Standards.
(WHO, Ed.) (2nd Editio.). WHO. Retrieved from
http://www.who.int/csr/resources/publications/surveillance/WHO_CDS_CSR_ISR_99_2_EN/en/
WHO, & CDC. (2010). Technical guideline for INTEGRATED
DISEASE SURVEILLANCE AND RESPONSE IN THE AFRICAN REGION. (WHO & CDC,
Eds.) (2nd Editio.). WHO, CDC.
Ye, J., Rust, G., Fry-Johnson, Y., & Strothers, H. (2009).
E-mail in patient-provider communication: a systematic review. Patient
Education and Counseling, 80(2), 266-73.
doi:10.1016/j.pec.2009.09.038
| 


